This study aimed to examine associations of the impact of COVID-19 pandemic on family life with emotional and behavioral health among preschool children.
MethodsA longitudinal study including 1595 preschool children aged 3–6 years and their families was conducted in Anhui Province. The linear regression was applied to examine associations between the impact of COVID-19 pandemic on family life and emotional and behavioral health.
ResultsResults of the multivariable linear regression indicated that the severe impact of COVID-19 pandemic on family life was significantly associated with more sleep problems, poor dietary behavior habits, more anxiety symptoms, and more problematic behaviors; and these effects exhibited gender and age differences.
ConclusionsThe severe impact of COVID-19 pandemic on family life significantly increased the risk for exacerbated emotional and behavioral health among preschool children. It is considered vital to identify risk factors for vulnerable families and then to implement precise interventions when necessary for emotional and behavioral health of children in these families.
With the emergence of the coronavirus disease 2019 (COVID-19) and its rapid spread worldwide, the World Health Organization defined it as a global pandemic on March 11, 2020 (Mahase, 2020). Many countries had to immediately adopt national or regional restrictions on outdoor activities and social distancing to effectively curb the spread of COVID-19. Particularly in China, strict restrictions were first implemented in the early period of the pandemic, which became an unprecedented challenge for families and children. Several families encountered unemployment, financial insecurity, food insecurity, social isolation, and confinement-related stresses, which are expected to pose an acute threat to parents and children (Patrick et al., 2020).
The sudden outbreak of the COVID-19 pandemic may have a dramatic impact on children's mental health (Duan et al., 2020). Researchers have alarmed that disruptions to routines and services, increasing family stressors, social isolation, and domestic violence are creating conditions that augment the scale of children's mental health problems (Russell, Hutchison, Tambling, Tomkunas & Horton, 2020). Early evidence has indicated that the prevalence of depression, anxiety, problematic behaviors, sleep disorders, and post-traumatic stress symptoms among children is higher during the COVID-19 pandemic (Liu et al., 2021a; Ma et al., 2021; Tang, Xiang, Cheung & Xiang, 2021). Another cohort study indicates that children are experiencing significantly more mental health problems versus the pre-pandemic period (Ravens-Sieberer et al., 2021). Hence, children's emotional and behavioral health merits special attention during the global pandemic.
As the primary support system and socializing institution for children, a family provides a stable and secure environment for children of different age groups in the unprecedented COVID-19 pandemic (Kocayörük, 2016). Furthermore, parents play an important role in the family (Fong & Iarocci, 2020). The pandemic has resulted in prolonged school and childcare closures in China. Parents had to make efforts to plan new caregiving methods, work, and education routines. Occasionally, parents may be at aggravated risks for role stress as they adapt to changing between work and family demands, especially in terms of potential conflict (Brock & Laifer, 2020). In families experiencing severe hardships, children's mental health seems to be worse (Gassman-Pines, Ananat & Fitz-Henley, 2020). A recent study has indicated that disruptions to family life and parenting during the pandemic predict subsequent children's internalizing and externalizing problems (Fosco, Sloan, Fang & Feinberg, 2021). Preschool children may be more vulnerable to the impact of stressful events such as the COVID-19 outbreak due to their developing cognitive capacities and their dependence on caregivers’ help to cope with such events (De Young & Landolt, 2018; Salmon & Bryant, 2002). One study has revealed the relationship between family factors and sleep health among preschool children, especially in families which struggle with dramatic lifestyle changes during the pandemic (Liu et al., 2021b). We speculate that any aspects of family life changing will alter children's supportive environment and then affect their emotional and behavioral health. However, research on the association of the impact of COVID-19 pandemic on family life with emotional and behavioral health among preschool children is relatively scarce. Therefore, it is worthwhile to explore the association between such impact and preschool children's emotional and behavioral health.
However, most studies mainly addressed emotional and behavioral health in the early stage of the COVID-19 outbreak (Liu et al., 2021b; Ma et al., 2021; Tang et al., 2021). The long-term pandemic impact on children's emotional and behavioral health has not been deeply tracked. Especially in China, the COVID-19 pandemic has gone through the outbreak, restraint of spreading, resumption of work and school, and the regular epidemic prevention and control. In this context, the impact on emotional and behavioral health seems to be long-term rather than limited to a particular time point. Meanwhile, as the global pandemic is ongoing, this study may provide a better reference for other countries that continue to suffer the effects of the pandemic. Based on a longitudinal study, we directly assessed the overall impact of COVID-19 pandemic on family life (including multiple aspects such as family income, family daily activities, family relationship, family members’ physical health, and so on) during a whole year. In addition, it was hypothesized that the long-term pandemic impact on family life might contribute to aggravating emotional and behavioral health among preschool children. Hence, the association of the impact of COVID-19 pandemic on family life with children's emotional and behavioral health was explored.
MethodStudy design and participantsThe data was from an ongoing longitudinal study on psychosomatic health among preschool children in Anhui Province. Anhui Province located in the middle of China is next to Hubei Province which is the most affected areas in early 2020. At the early period of COVID-19 pandemic in 2020, strict restrictions were immediately implemented in this province. In addition, according to the statistic data in 2020, there were 19.674 million migrant workers from Anhui Province accounting for 11.6% of the 31 provinces in China (Anhui Provincial Bureau of Statistics, 2021; National Bureau of Statistics of China, 2021). And it is always called as a large province of migrant workers.
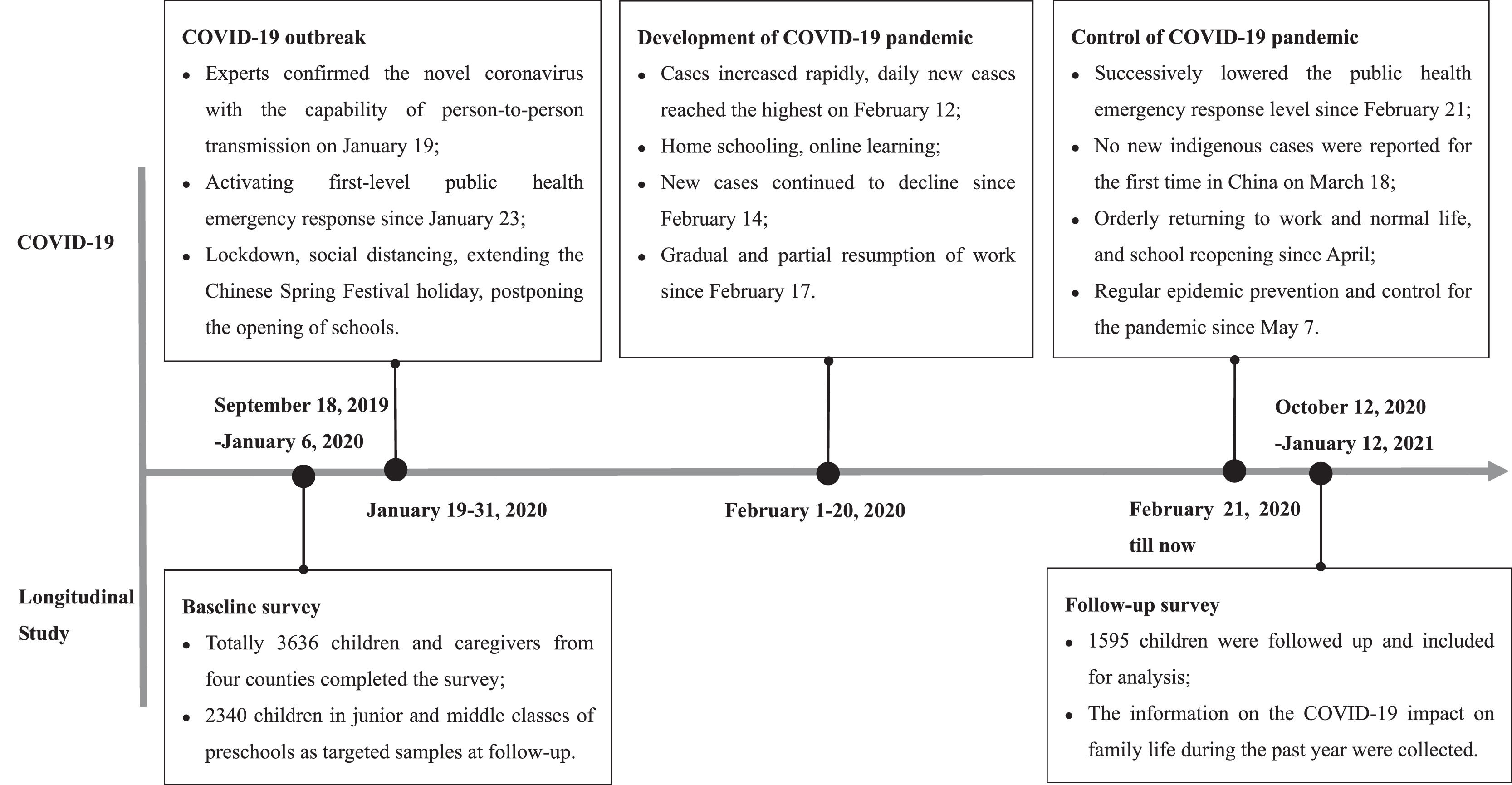
The baseline survey was conducted in September 2019-January 2020 (before the COVID-19 outbreak in China). The follow-up survey was conducted in October 2020-January 2021. The baseline survey via convenience sampling included 3636 preschool children of 26 preschools in Funan County of Fuyang City, Changfeng County and Fexi county of Hefei City, Bowang District of Maanshan City, respectively located in the northern, middle, and southern areas of Anhui Province, China. Participants included children aged 3–6 years and their primary caregivers who voluntarily participated in the survey. Participants with communication barriers, cognitive impairment, deafness, or aphasia and children with severe physical or mental illnesses were excluded. Caregivers were invited to provide informed consent before data collection and then complete a structured questionnaire by face-to-face interview. The follow-up survey included 2340 baseline participants in the junior and middle classes of preschools as targeted samples (because baseline children in senior class of preschools would enter into primary school and exceed 6 years old of inclusion criteria when the follow-up survey was conducted, they were excluded at follow-up). Finally, 1595 children were effectively followed up and included in the analyses (detailed timeline of the survey and COVID-19 pandemic summarized in Figure. 1). Characteristics of the completed follow-up and lost to follow-up children were presented in Table A.1. The main characteristics were not significantly different between the completed follow-up and lost to follow-up children except for the variable of family structure, which indicated that the missing is random on the whole. The information including children's and parental sociodemographic characteristics, family factors, and the emotional and behavioral health was collected at baseline. The data including the impact of COVID-19 pandemic on family life during the past year and the emotional and behavioral health was collected at follow-up. Ethics approval was obtained from the Ethics Committee of Anhui Medical University (No. 20180402).
Timeline of the study and COVID-19 pandemic in China.
Note: The data of COVID-19 pandemic was from the State Council Information Office of the People's Republic of China (2020). Fighting Covid-19 China in Action. http://www.scio.gov.cn/zfbps/ndhf/42312/Document/1682143/1682143.htm.
Sociodemographic characteristics and family factors included child's age, gender, and body mass index (BMI); parental age, education level, marital status, occupation types, number of household children, monthly family income, and family structure (nuclear family, non-nuclear family). Child's BMI was calculated by dividing the weight (kg) by height (m) squared; and the World Health Organization BMI criteria for preschool children were applied (WHO & de Onis, 2006). The nuclear family was defined as a family consisting of parents and children, otherwise it was defined as a non-nuclear family.
The impact of COVID-19 pandemic on family lifeCaregivers were asked to report perceived overall impact of COVID-19 pandemic on family life. The single item question was asked “Did you feel the COVID-19 pandemic have affected your family life such as family income, family daily activities, family relationship, family members’ physical health, and any other impacts on families in the past year?” Then, there were four options representing four different impact degrees (1=“almost no impact”, 2=“less impact”, 3=“moderate impact”, and 4=“severe impact”) for participants to select one. Participants could directly response if any impacts occurred, which primarily depended on their overall perception. In this study, the negative of the COVID-19 pandemic on family life included three groups based on the impact degrees: the almost no impact and less impacts were combined into the less impact group as the reference group; and the moderate impact and severe impact groups were regarded as the two study groups, respectively.
Emotional and behavioral health assessmentThe Children's Sleep Habits Questionnaire (CSHQ) was used to assess sleep problems (Liu, Wang, Tang, Wen & Li, 2014). This 33-item measure includes 8 dimensions (bedtime resistance, sleep onset delay, sleep duration, anxiety around sleep, night wakings, parasomnias, sleep disordered breathing, and daytime sleepiness). Caregivers reported children's sleep behaviors during a recent week on three-point Likert scales (3=“5–7 times/week”, 2=“2–4 times/week”, 0=“0–1 time/week”). Higher total scores reflect the more sleep problems, and Cronbach's alpha value was 0.74 in this study.
The Strength and Difficulties Questionnaires (SDQ) is frequently used to measure problematic behaviors among preschool children (Goodman, 2001). In this study, we adopted four subscales (conduct problems, peer problems, emotional symptoms, and hyperactivity) of the SDQ to assess children's problematic behaviors. It is scored on a 3-point Likert scale (0=“not fit” to 2=“complete fit”). Higher total scores indicate more problematic behaviors. In this study, Cronbach's alpha value for this scale was 0.707.
The adapted Identification and Management of Feeding Difficulties scale (IMFeD) was applied to evaluate the dietary behavior of children (Deng et al., 2012). This 17-item scale contains 6 dimensions (poor appetite, food preference, poor eating habit, fear of feeding, parental misperception, and organic disease). Caregivers were asked to report children's dietary behaviors the latest week on a 4-point Likert scale (1=“7 days/week” to 5=“almost absent”). Lower total scores indicate poor dietary behavior habits. Cronbach's alpha value for the scale in this study was 0.873.
Children's anxiety symptoms were assessed using the Chinese version of the Spence Preschool Anxiety Scale (SPAS) (Wang & Zhao, 2015). The SPAS including 28 items and 5 subscales (separation anxiety disorder, physical injury fears, social phobia, obsessive-compulsive disorder, and generalized anxiety disorder) describes the presence of anxiety symptoms on a 5-point Likert scale (0=“not at all true” to 4=“very often true”). Scores of the SPAS are obtained by adding up all items. Higher total scores indicated more anxiety symptoms, and Cronbach's alpha value for the scale was 0.911 in this study.
Statistical analysisCategorical variables were presented as frequencies and percentages. First, Pearson's chi-squared (χ2) test was used to compare the distribution of different impact degrees of COVID-19 pandemic on family life among different participants. Second, the paired-sample t-test was used to analyze the difference of emotional and behavioral problems between pre-pandemic and post-pandemic periods. Third, as the primary outcome of this study interest, the univariable and multivariable linear regressions were employed to respectively explore the association of moderate/severe impact of COVID-19 pandemic on family life with preschool children's emotional and behavioral health at follow-up. Finally, the analyses were separately conducted for gender- and age-group. All analyses were performed using SPSS software (SPSS Inc., USA; version 23.0). Statistical significance was defined as the P value less than 0.05 (two-tail test).
ResultsSample characteristicsA total of 1595 preschool children (54.5% boys) with a mean age of 4.12 (standard deviation=0.66) years participated in two surveys. Children were mainly from non-nuclear families (59.1%); 31.8% families had one child; 40.9% and 16.1% families were in the medium (5000–10,000 RMB) and high monthly income categories (>10,000 RMB), respectively. The number of participants reporting the almost no impact, less impact, moderate impact, and severe impact of the COVID-19 pandemic on family life were 167, 877, 400, and 151, respectively. The 1044 (65.4%) participants reporting almost no impact and less impact were combined into the less impact group as the reference group; and 400 (25.1%) participants reporting moderate impact and 151 (9.5%) participants reporting severe impact were included in the two study groups. The other characteristics of individuals and families are presented in Table 1.
The impact of COVID-19 pandemic on family life in 1595 families of different characteristics.
As shown in Table 1, the results showed that the difference was statistically significant in baseline number of household children, monthly family income, parental education level, and parental occupation between groups of less, moderate, and severe impact of COVID-19 pandemic on family life (P<0.05).
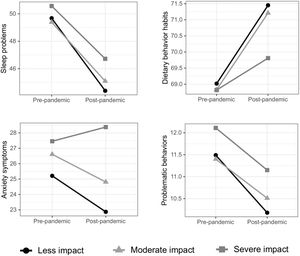
Difference of emotional and behavioral problems between pre-pandemic and post-pandemicSleep problems, problematic behaviors, dietary behavior habits, and anxiety symptoms were significantly alleviated at the post-pandemic period in groups of less and moderate impact (P<0.05). Except for sleep problems (P<0.05), changes in problematic behaviors, dietary behavior habits, and anxiety symptoms were not statistically significant between the pre-pandemic and post-pandemic period in the group of severe impact (P>0.05) (Figure A.1).
Associations of the impact of COVID-19 pandemic on family life with emotional and behavioral health at follow-upTable 2 summarizes the associations of the moderate/severe impact of COVID-19 pandemic on family life with emotional and behavioral health at follow-up. Univariable linear regression analyses showed that the moderate impact of COVID-19 pandemic on family life was positively associated with more anxiety symptoms (β=1.942, P = 0.033) compared with less impact. In addition, the severe impact of COVID-19 pandemic on family life was positively associated with more sleep problems (β=2.322, P<0.001), more anxiety symptoms (β=5.513, P<0.001), and more problematic behaviors (β=0.963, P = 0.016). In the multivariable model, the severe impact of COVID-19 pandemic on family life was significantly associated with more sleep problems (β=2.076, P = 0.001), more anxiety symptoms (β = 5.101, P<0.001), more problematic behaviors (β=0.856, P = 0.032), and poor dietary behavior habits (β=−1.801, P = 0.048).
Associations of the impact of COVID-19 pandemic on family life with preschool children's emotional and behavioral health at follow up.
Note: a Multivariable linear regression model adjusted for child's age, gender, body mass index, family structure, number of household children, monthly family income, parental marital status.
As presented in Table 3, multivariable linear regression model results revealed that the severe impact of COVID-19 pandemic on family life was significantly associated with more sleep problems (β=2.885, P = 0.001), more anxiety symptoms (β=6.452, P<0.001), and poor dietary behavior habits (β=−2.647, P = 0.032) in boys but not in girls. Regarding age, diverse effects of COVID-19 pandemic impact on family life on children's emotional and behavioral health were detected among different age groups. In the group of 3 years, the severe impact significantly predicted more anxiety symptoms (β=7.140, P = 0.001) and problematic behaviors (β=1.320, P = 0.034). In the group of 4–5 years, the severe impact was associated with increased sleep problems (β=2.510, P = 0.002) and anxiety symptoms (β=3.675, P = 0.041).
Associations of the impact of COVID-19 pandemic on family life with preschool children's emotional and behavioral health at follow up across gender and age.
Note: a Multivariable linear regression model adjusted for child's age, gender, body mass index, family structure, number of household children, monthly family income, parental marital status.
To the best of our knowledge, this study, based on a longitudinal design, was the first to explore the associations of the impact of COVID-19 pandemic on family life with emotional and behavioral health among preschool children in China. Lower monthly family income, and parents with occupation as workers, businessman/service workers and farmer/housework were more vulnerable to the impact of COVID-19 pandemic, which was supported by other studies (Feinberg et al., 2021; Qian & Fan, 2020). In China, services, businesses, and manufacturing are most affected by the pandemic (Chen & Li, 2020), in turn resulting in unemployment, irregular salaries, and lower family incomes. Indeed, recent studies have shown that individuals with lower financial sources tend to manifest more depressive symptoms and perceived stress from the COVID-19 pandemic (Ettman et al., 2020; Ruengorn, Awiphan, Wongpakaran, Wongpakaran & Nochaiwong, 2021). According to intergenerational transmission theory, in both pandemic and non-pandemic period, parental mental distress is associated with children's emotional and behavioral health (Aktar, Majdandžić, de Vente & Bögels, 2014; Liu et al., 2021a). This highlights that children's emotional and behavioral health are required adequate attention especially in these vulnerable families during the COVID-19 pandemic and post-pandemic.
With regard to children's behavioral problems, this study indicated that the severe impact of COVID-19 pandemic on family life was associated with more sleep problems, and the effect was more significant in boys and older children. In accordance with this, one study has confirmed that preschool children within household chaos due to the COVID-19 pandemic are susceptible to sleep problems (Kracht, Katzmarzyk & Staiano, 2021). Additionally, several studies have indicated that sleep quality of preschool children decreases in the COVID-19 lockdown (Dellagiulia et al., 2020; Markovic, Mühlematter, Beaugrand, Camos & Kurth, 2021). Furthermore, Markovic et al. (2021) also detect a significant age difference. However, some inconsistent results have emerged. Some studies indicate that children in prolonged home confinement of COVID-19 pandemic have fewer sleep problems or other studies failing to detect a significant impact on preschool children and gender differences (Lim et al., 2021; Liu et al., 2021b). A possible explanation was that most studies merely described sleep problems during the period or its differences versus the pre-pandemic period, which could not specify the impact stemming from the COVID-19 pandemic. Regarding dietary behaviors, one study has shown that higher parental COVID-19-specific stress increase children's intake frequency of sweet and savory snacks (Jansen et al., 2021). During the lockdown, with parental feeding practices and food shopping motivations changing, children's dietary behaviors changed (Philippe, Chabanet, Issanchou & Monnery-Patris, 2021). In addition, one study has suggested that the appetite augmentation during lockdown is significantly associated with age and gender (Galali, 2021). In the same vein, the present study indicated that the severe impact of COVID-19 pandemic on family life was associated with poor dietary behavior habits, particularly in boys. However, evidence on dietary behavior problems is scarce among preschool children, which is needed to further focus on this population.
In addition, the findings demonstrated that the severe impact of COVID-19 pandemic on family life increased anxiety symptoms and problematic behaviors. Furthermore, anxiety symptoms and problematic behaviors significantly alleviated at follow-up in groups of less and moderate impact, but changes in anxiety symptoms and problematic behaviors were not statistically significant in the group of severe impact. During the COVID-19 pandemic, many families have experienced hardships including unemployment, income loss, caregiving burden, and illness. In families which have suffered from multiple hardships, preschool children have worse mental health (Gassman-Pines et al., 2020). Indeed, research from other countries has shown that the pandemic substantially affects preschool children's emotional and behavioral health especially during school lockdown (Cantiani et al., 2021; Vasileva, Alisic & De Young, 2021). Gassman-Pines et al. (2020) report that preschool children in families with more severe hardships manifested more worries. Preschool children often worry about getting sick and infecting others, and permanent changes in daily life due to the COVID-19 pandemic (Vasileva et al., 2021). Vasileva et al. (2021) propose that preschool children seem to experience the threat of the pandemic but struggle to understand causality and risk, thus appropriate parent-child communications are crucial to support them in realizing the situation and relevant risk during hard times. However, most studies have only examined the difference in children's emotional and behavioral health compared to the pre-pandemic period (Cantiani et al., 2021; Ma et al., 2021; Vasileva et al., 2021). Few studies have evaluated the associations of the direct impact of COVID-19 pandemic on family life with children's emotional and behavioral health (Gassman-Pines et al., 2020). This study highlighted that the COVID-19 pandemic might affect children's emotional and behavioral health by directly assessing the impact of COVID-19 pandemic on family life, which prompted effective intervention for mitigating emotional and behavioral problems among vulnerable preschool children to be warranted.
This study has several strengths. First, based on a longitudinal design, baseline family characteristics were collected before the COVID-19 outbreak and emotional and behavioral health of children at baseline and one-year follow-up. Thus, we could fully investigate associations of the impact of COVID-19 on family life with emotional and behavioral health. Second, although other longitudinal studies repeatedly collected and compared mental health between pre-pandemic and post-pandemic, they were not able to specifically attribute any impacts to the COVID-19 pandemic based on incomparable conditions. This study could overcome this problem by directly assessing impact degrees of COVID-19 pandemic on family life. Nevertheless, some limitations of this study should be noticed. First, as information on the impact of COVID-19 pandemic on family life was an additional assessment at that time of the COVID-19 pandemic occurrence in this longitudinal study, despite efforts to reduce participants’ burden of filling out the questionnaire, one limitation was that a single item evaluation was applied to generally assess COVID-19 impact on family life. When the survey was conducted, the single item was detailedly explained as any impacts on families due to the pandemic. Additionally, several previous studies on COVID-19 pandemic and mental health also applied single item measure to assess these variables (eg. personal impact of COVID-19, change in their mental health status during pandemic, family distress, family quality of life, and family happiness) (Haliwa, Spalding, Smith, Chappell & Strough, 2021; Jenkins et al., 2021; Meral, 2022). To some extent, although the single item evaluation may be less reliable than multi-item, a scale which is user-friendly and time-efficient is as well as reliable and valid. Furthermore, evidence has demonstrated that single item measure is commonly used in epidemiological surveys, and it is associated with the multi-item measure (Ahmad, Jhajj, Stewart, Burghardt & Bierman, 2014). Meanwhile, it should not be ignored that the results give us a meaningful study direction. Future studies need to subdivide the effects of different aspects of impacts on children's health. Second, when the different study groups (eg. the moderate/severe impact group) were defined, the group sizes were small especially in the severe impact group. Although the number in the severe impact group may be relatively small, the impact on preschool children's emotional and behavioral health was not too optimistic. Hence, children's emotional and behavioral health in this group needs more attention. Third, information on the impact of COVID-19 pandemic on family life was retrospectively collected, which might raise the recall bias. Finally, the assessment of emotional and behavioral health among children via caregiver reports were prone to subjectivity and reporting bias.
ConclusionThe severe impact of COVID-19 pandemic on family life increased the risk for sleep problems, poor dietary behavior habits, anxiety symptoms, and problematic behaviors among preschool children. It is considered vital to identify risk factors for vulnerable families and then to implement precise interventions when necessary for emotional and behavioral health of children in these families.
FundingThis work was supported by National Natural Science Foundation of China [grant number 81872704].
We acknowledge the efforts of the research team, the local Center for Disease Control and Prevention and all preschools, and all the children and families who participated in this research.
Characteristics of completed follow-up and lost to follow-up preschool children.