The standard oesophago-gastro-duodenoscopy procedure is performed with a single endoscopist (SE). Nurse-assisted (NA) oesophago-gastro-duodenoscopies have not yet been studied. We aimed to evaluate the efficacy of an NA endoscopy compared to an SE endoscopy.
MethodsA prospective, single-center, randomized trial, in which 500 adult patients were divided into two groups. In the first group, patients underwent an endoscopy with an SE. In the second group, the endoscopy was performed with an NA. The ease of the procedure (scores 1–4; 1 difficult, 2 satisfactory, 3 easy, 4 veryeasy), evaluation of patient satisfaction (scores 1–4; 1 uncomfortable, 2 satisfactory, 3 comfortable, 4 verycomfortable), total time of the procedure and vocal cord observation were determined as quality indicators.
ResultsMean patient satisfaction scores in groups 1 and 2 were 2.98±0.79 and 3.11±0.78, respectively (p=0.043), with uncomfortable ratings in 5.2% vs 4%, satisfactory in 16.8% vs 13.2%, comfortable in 53.2% vs 50.4%, and very comfortable in 24.8% vs 32.4% of patients in groups 1 and 2, respectively. Retching rates during the procedure were 54.4% and 45.2% (p=0.040) in groups 1 and 2, respectively. No differences were seen in vocal cord observation (54.4% vs 56.0%), total procedure time (2.35±1.56 vs 2.41±1.48min) and easy score (3.26±0.603 vs 3.25±0.64) in groups 1 and 2 for the procedures. Very easy, easy, satisfactory, and difficult ratings were given by 33.6% vs 34.8%, 60.4% vs 56.4%, 4.8% vs 7.6% and 1.2% vs 1.2% of groups 1 and 2, respectively.
ConclusionsCompared with the conventional method, the assisted endoscopic technique provides more comfort and less gag reflex without increasing the processing time or difficulty of performing the procedure.
El procedimiento estándar de esofagogastroduodenoscopia se realiza con un solo endoscopista (SE). La esofagogastroduodenoscopia realizada con una enfermera asistida (NA, por sus siglas en inglés) aún no se ha estudiado. Nuestro objetivo es evaluar la eficacia de una endoscopia asistida por una enfermera en comparación con un SE.
MétodosSe trata de un ensayo prospectivo, monocéntrico y aleatorizado. Quinientos pacientes adultos fueron divididos en 2 grupos. En el primer grupo, los pacientes se sometieron a una endoscopia con un SE; en el segundo grupo, la endoscopia se realizó con una NA. Se determinaron como indicadores de calidad la facilidad del procedimiento (puntuaciones 1-4; 1 difícil, 2 satisfactorio, 3 fácil y 4 muy fácil), la evaluación de la satisfacción del paciente (puntuaciones 1-4; 1 incómodo, 2 satisfactorio, 3 cómodo y 4 muy cómodo), el tiempo total del procedimiento y la observación de las cuerdas vocales.
ResultadosLas puntuaciones medias de satisfacción del paciente en los grupos 1 y 2 fueron de 2,98±0,79 y 3,11±0,78, respectivamente (p=0,043), con puntuaciones de incómodo en el 5,2 frente al 4%, satisfactorio en el 16,8 frente al 13,2%, cómodo en el 53,2 frente al 50,4% y muy cómodo en el 24,8 frente al 32,4% de los pacientes de los grupos 1 y 2, respectivamente. Las tasas de arcadas durante el procedimiento fueron del 54,4 y el 45,2% (p=0,040) en los grupos 1 y 2, respectivamente. No se observaron diferencias en la observación de las cuerdas vocales (54,4 frente al 56,0%), el tiempo total del procedimiento (2,35±1,56 frente al 2,41 ±1,48min) y la puntuación de fácil (3,26 ±0,603 frente al 3,25 ±0,64) en los grupos 1 y 2 para los procedimientos. Muy fácil, fácil, satisfactorio y difícil fueron calificados por el 33,6 frente al 34,8%, el 60,4 frente al 56,4%, el 4,8 frente al 7,6% y el 1,2 frente al 1,2% de los grupos 1 y 2, respectivamente.
ConclusionesEn comparación con el método convencional, la técnica endoscópica asistida proporciona más comodidad y menos reflejo nauseoso sin aumentar el tiempo de tratamiento ni la dificultad de realizar el procedimiento.
Esophagogastroduodenoscopy (EGD) is an essential diagnostic and therapeutic procedure for the upper gastrointestinal system, generally well-tolerated and safe, for examination of the upper GI tract. The quality of the procedure is important for endoscopy, and patient satisfaction is considered one of the quality criteria of endoscopy.1 Gastroenterology societies have been working to define the components of high-quality endoscopy.2,3 Many topical and intravenous (IV) anesthetics have been used to increase patient satisfaction,4–9 and most endoscopists prefer to use the sedatives during the procedure for their anxiolytic, amnestic, and analgesic effects.9,10 However, medications used to provide sedation have potential side effects, such as dysrhythmia, hypotension, and respiratory depression.9 In a previous study, the technical skill of the endoscopists was found to be one of the most important factors that enhance patient satisfaction.11 However, there are many studies in the literature that investigate patient satisfaction from the use of different endoscopic techniques.12–19 In some studies, the effect on patient satisfaction of the technique, comparing colonoscopic skills with a single- or double-operator method, was investigated.12–16 Although there were several studies on colonoscopy,12–16 no study on EGD using an assisted endoscopy method could be found in the literature. Although two-operator techniques are applied in some advanced upper endoscopic procedures, such as percutaneous endoscopic gastrostomy (PEG), double-balloon enteroscopy, and per-oral endoscopic myotomy (POEM),17–19 EGD is usually performed with the single operator technique.20 Endoscopy nurses do not usually interfere directly in the procedure but perform a variety of principal tasks during GI endoscopy, such as operating a forceps or a snare, injection of luminal agents, submucosal injection for lifting, injecting contrast during ERCP, and the like.21
In our study, we hypothesized that patient comfort and quality of procedure are affected by endoscopic techniques; thus, we aimed to evaluate the efficacy of endoscopy performed with the physician assisted by an endoscopy nurse (two-operator method) for the comfort of patients and to obtain conscious responses from patients who were not sedated. To the best of our knowledge, this is the first study evaluating the nurse-assisted endoscopy technique and related comfort and ease of the procedure.
Patients and methodsStudy designThis prospective, single-center, randomized controlled trial was performed in our tertiary center. Patients ≥18 years of age who were scheduled for esophagogastroduodenoscopy, at the outpatient clinics of the Gastroenterology Department between August 2015 and July 2016 were eligible to participate. Written informed consent was obtained from all patients. The study was reviewed and approved by the local institutional ethical committee (10/17–20.09.2013).
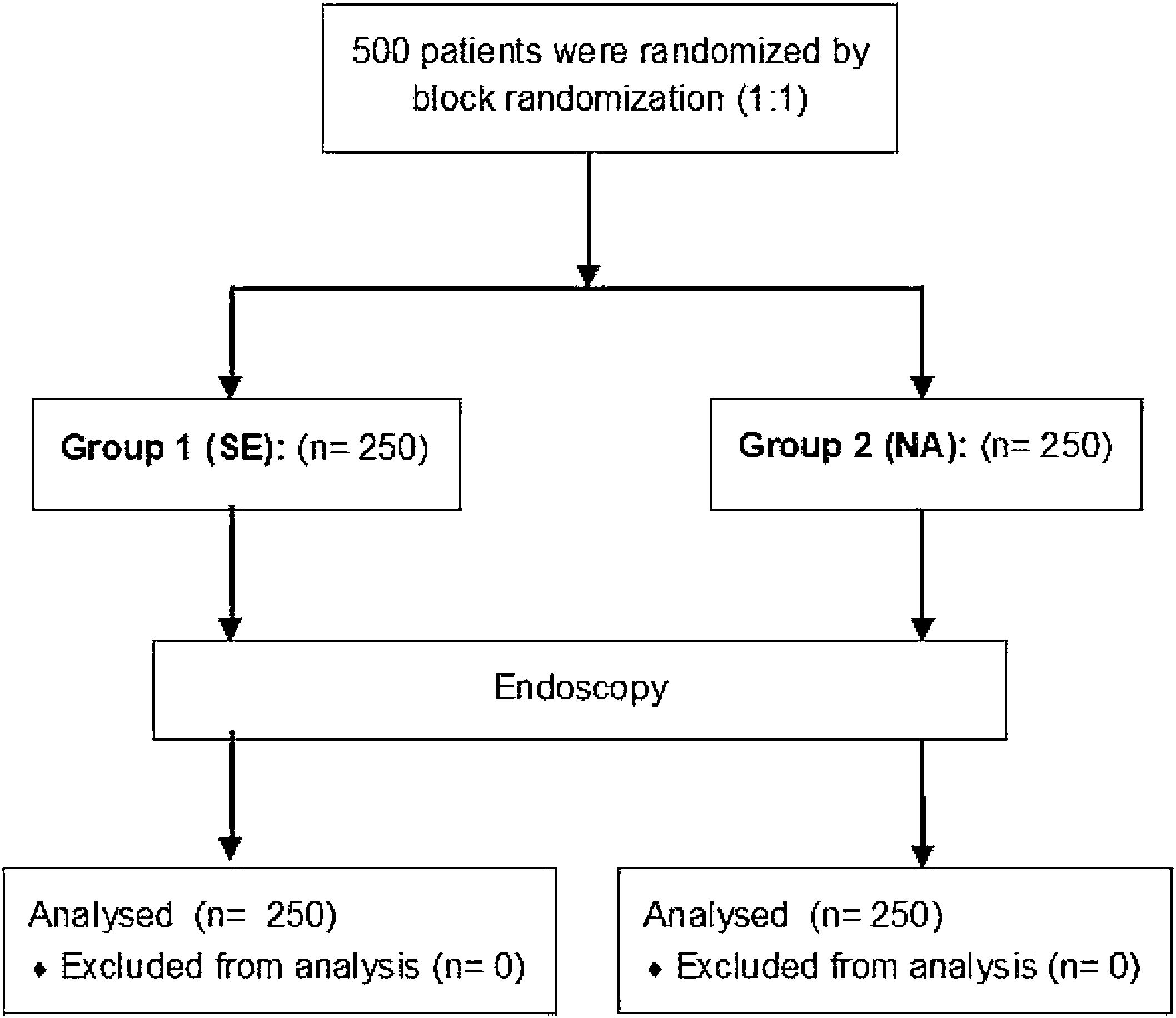
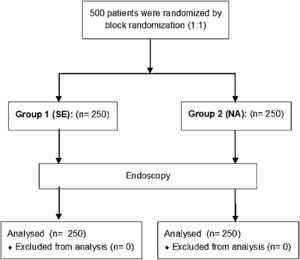
PatientsIndications for EGD and gastrointestinal symptoms were recorded for all patients. Patients identified according to the exclusion criteria—nasoenteral feeding tube, unstable clinical condition, morbid obesity, acute or chronic renal failure, decompensated heart failure, pregnancy, neurologic and psychiatric disorders, and previous abdominal operations—were excluded from randomization and from the study. Five hundred consecutive patients between ages 18 and 90 years were enrolled and randomly assigned to one of two groups: group 1, endoscopy performed with single endoscopist (SE) without assistance or group 2, nurse-assisted (NA) endoscopy, performed with nurse assistance (Fig. 1).
RandomizationPatients were randomly assigned to one of the two groups using a block randomization method (1:1, a block size of 4 and 6) by an independent physician using a computer-generated randomization list.
EndoscopyIn our department, upper endoscopy has been routinely performed without sedation due to the high number of patients, which prolongs the endoscopy appointment period and increases costs. Premedication with any sedative was not performed in this study; only topical anesthesia was administered to all patients 3min before the endoscopy in two doses at 1-min intervals in a 10% spray formulation with 100mg lidocaine, and the patients were asked to swallow lidocaine after each spraying interval. Before the study, more than 1000 endoscopic procedures had been performed with the assisted endoscopic method for 6 months for orientation purpose, by two experienced endoscopists who had performed about 4000 gastroscopies per year for 5 years (YC and IY). Two endoscopy nurses, experienced in both endoscopic methods, were assigned to the endoscopy procedure. All endoscopic procedures were performed between 8a.m. and 11a.m., using high-resolution adult video-endoscopes from Fujinon Corp., VP-4450HD processor, EG-530WR endoscope (Fujifilm Corporation, Tokyo, Japan). Successful completion of the procedure was a predetermined quality indicator. Reaching the second part of the duodenum and retro flexion in the stomach were determined as additional success indicators.
Endoscopy techniqueIn the first group, with a single endoscopist (SE), the control section of the endoscope was kept in the palm of the left hand. While the wheels and buttons were controlled with the left-hand, the insertion tube was grasped approximately 30cm from the distal tip and advanced into the mouth with the right hand. The tip of the endoscope is moved up or down with the left-hand thumb using the up/down deflection wheel, and to the right or left with the index and middle finger using the left/right deflection wheel. In the second group, nurse-assisted (NA) endoscopy, the control section of the endoscope was kept in the palm of the left hand by the endoscopist. While the air insufflation, water, and suction buttons were controlled with the left-hand index and middle fingers, up/down and right/left angulation wheels were controlled with the righthand. The insertion tube was kept approximately 30cm from the distal tip and advanced into the mouth by the endoscopy nurse during the insertion and withdrawal phases of the endoscopy. The advancing, withdrawal, and axial rotation of the endoscope were the responsibility of the nurse. In both groups, the tip of the gastroscope was pushed downward gently until the vocal cords and epiglottis become visible. The role of the second endoscopy nurse was to perform a variety of principal tasks in all procedures in each group during GI endoscopy, such as operating a forceps or a snare, injection of luminal agents, and so on.
End pointsThe primary endpoint of the study was to evaluate the patients’ satisfaction, and the secondary endpoint was to compare the ease of procedure of two endoscopic methods.
Evaluation of endoscopist's assessmentsFour parameters were considered in this study for evaluation of procedures by the endoscopist: 1. Observation of the vocal cords, 2. Retching during the procedure, 3. Total time of the procedure, 4. Ease of the procedure. Although not included in the European Society of Gastrointestinal Endoscopy (ESGE) guidelines, the gag reflex and visualization of the vocal cords were taken as variable criteria.22,23 The laryngeal assessment was performed as quickly as possible to avoid triggering the gag reflex. During the transition to hypopharynx, if vocal cords are visible, it was scored as 1; if not visible, it was scored as 0. The presence of the gag reflex was evaluated from the insertion of the endoscope into the hypopharynx to withdrawal of the endoscope; the absence of gagging was scored as 0 and the presence as 1. Total procedure time was defined as the total time from insertion of the endoscope into the mouth until the removal of the endoscope. The endoscopist evaluated the total time and the ease of performing the procedure at the end of endoscopy. The ease of performing the procedure was scored 1 to 4 (1 difficult, 2 satisfactory, 3 easy, 4 very easy) by the endoscopist and identified as one of the quality indicators.
Assessment of the patient's satisfactionPatient satisfaction was determined as a quality indicator. All patients were administered a questionnaire dealing with satisfaction and quality of the procedure after the end of endoscopy, and they were asked to score 1–4 (1 uncomfortable, 2 satisfactory, 3 comfortable, 4 very comfortable).
StatisticsStatistical power for the patient satisfaction rate variable was calculated before starting the study. We assumed there would be no difference in patient satisfaction rates between the two techniques. In a previous study evaluating patient satisfaction, the patient satisfaction rate of upper GIS endoscopy was reported as 86%, and the satisfaction rate in this study was taken as reference.24 Consequently, the sample size of 247 patients per group was calculated to determine the 10% difference between the two groups when the alpha level was set to 0.05 and 90% statistical power was assumed.
Data were statistically analyzed using SPSS for Microsoft Windows 17.0 (SPSS Inc., an IBM Company, Chicago, IL). The Mann–Whitney U test was used for comparison of the two independent groups and chi-square tests for categorical measures. p values below 0.05 were considered significant in all analyses.
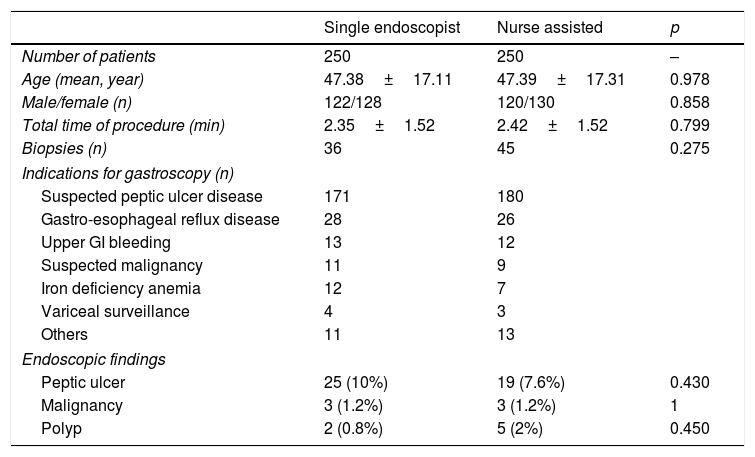
ResultsBaseline characteristicsThe study population consisted of 500 patients. The mean age and sex distributions in groups 1 and 2 were 47.38±17.11 vs 47.39±17.31 years, and 48.8% vs 48% males, respectively (p>0.05). Eighty-one biopsies were performed during endoscopy, and the mean time of procedure was 2.35±1.52 and 2.42±1.52min, respectively. The characteristics of the patients are presented in Table 1.
Characteristics of the patients.
| Single endoscopist | Nurse assisted | p | |
|---|---|---|---|
| Number of patients | 250 | 250 | – |
| Age (mean, year) | 47.38±17.11 | 47.39±17.31 | 0.978 |
| Male/female (n) | 122/128 | 120/130 | 0.858 |
| Total time of procedure (min) | 2.35±1.52 | 2.42±1.52 | 0.799 |
| Biopsies (n) | 36 | 45 | 0.275 |
| Indications for gastroscopy (n) | |||
| Suspected peptic ulcer disease | 171 | 180 | |
| Gastro-esophageal reflux disease | 28 | 26 | |
| Upper GI bleeding | 13 | 12 | |
| Suspected malignancy | 11 | 9 | |
| Iron deficiency anemia | 12 | 7 | |
| Variceal surveillance | 4 | 3 | |
| Others | 11 | 13 | |
| Endoscopic findings | |||
| Peptic ulcer | 25 (10%) | 19 (7.6%) | 0.430 |
| Malignancy | 3 (1.2%) | 3 (1.2%) | 1 |
| Polyp | 2 (0.8%) | 5 (2%) | 0.450 |
n: number.
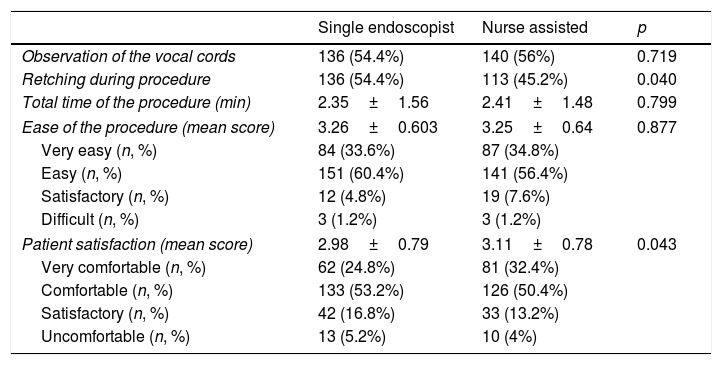
The rate of observation of the vocal cords was 54.4% in group 1 and 56% in group 2. The ranking of ease of performing the procedure was similar between the two groups. While 94% of the procedures in group 1 and 91.2% of the procedures in group 2 were classified as easy and very easy, 4.8% of the procedures in group 1 and 7.6% of the procedures in group 2 were classified as satisfactory. The percentage of those who stated difficult was the same in both groups (1.2%). There was no significant difference between the two groups in the rate of observation of the vocal cords or in the rates of ease of performing the procedure (p>0.05) (Table 2).
Details of physician's assessment of the procedure, patients’ satisfaction and procedural quality assessment.
| Single endoscopist | Nurse assisted | p | |
|---|---|---|---|
| Observation of the vocal cords | 136 (54.4%) | 140 (56%) | 0.719 |
| Retching during procedure | 136 (54.4%) | 113 (45.2%) | 0.040 |
| Total time of the procedure (min) | 2.35±1.56 | 2.41±1.48 | 0.799 |
| Ease of the procedure (mean score) | 3.26±0.603 | 3.25±0.64 | 0.877 |
| Very easy (n, %) | 84 (33.6%) | 87 (34.8%) | |
| Easy (n, %) | 151 (60.4%) | 141 (56.4%) | |
| Satisfactory (n, %) | 12 (4.8%) | 19 (7.6%) | |
| Difficult (n, %) | 3 (1.2%) | 3 (1.2%) | |
| Patient satisfaction (mean score) | 2.98±0.79 | 3.11±0.78 | 0.043 |
| Very comfortable (n, %) | 62 (24.8%) | 81 (32.4%) | |
| Comfortable (n, %) | 133 (53.2%) | 126 (50.4%) | |
| Satisfactory (n, %) | 42 (16.8%) | 33 (13.2%) | |
| Uncomfortable (n, %) | 13 (5.2%) | 10 (4%) | |
The rates of retching during procedure were 54.4% in group 1 and 45.2% in group 2 patients (p=0.040). Mean patient satisfaction scores in groups 1 and 2 were 2.98±0.79 and 3.11±0.78, respectively (p=0.043). An uncomfortable procedure was experienced by 5.2% of group 1 and 4% of group 2 patients. Satisfactory scores given in groups 1 and 2 were 16.8% and 13.2%, comfortable scores were 53.2% and 50.4%, and very comfortable scores were 24.8% and 32.4%, respectively (Table 2).
Adverse eventsNo infection, perforation, or pulmonary or cardiac adverse events were observed in this study. Minor incidents, such as self-limited bleeding of the hypopharynx due to mucosal laceration, were observed in only six patients (two in group 1 and four in group 2). This difference was not statistically significant (p=0.451).
DiscussionThis study was conducted to examine whether nurse-assisted endoscopy is as safe and effective as the single-endoscopist method. In this study, we evaluated the efficacy of endoscopy performed with nurse assistance as an alternate technique for patient comfort, and we found that the assisted endoscopic technique provides more comfort and less gag reflex, without increasing the processing time or difficulty in performing the procedure.
A high-quality endoscopic procedure should provide an accurate diagnosis while ensuring the satisfaction of the patient. One of the measures of a high-quality endoscopy is considered patient satisfaction.1 In recent studies, it has been found that the use of local anesthesia or intravenous (IV) sedation during the procedure may affect the patient's satisfaction score and ease of the procedure and reduce the risk of discomfort during the procedure.4–8 Although sedation was established as a quality criterion in the ESGE guidelines,22,23 sedatives were not used in our study because this is not the routine practice in our hospital. Although this preference may seem to be a shortcoming of the study, it provided us with very important information in terms of determining the comfort and discomfort of patients who were not sedated during the endoscopy procedure. While the implementation of sedation during the procedure may enhance patient satisfaction, technical skill is also associated with patient satisfaction. The technical skills of the endoscopist and nurse as well as the patient's perception of the technical skill of the endoscopist were determined as factors related to patient satisfaction.25 Yacavone et al. found that the endoscopist's technical skill was the most important factor influencing patient satisfaction.11
Although there are many studies on patient satisfaction, no studies were encountered in the literature review of the nurse-assisted method for the EGD procedure. The two-operator technique can be applied in colonoscopic and advanced upper endoscopic procedures, but EGD is usually performed with a single-operator technique. There are many studies on colonoscopy procedures with one-person and two-person techniques investigating the effect of technical skill and technical method. In a survey study with 75 endoscopists, 9368 colonoscopy procedures were performed, and the rate of polyp detection was slightly higher in the one-person technique, while the cecal intubation rate was found to be higher in the two-person technique. Pain score rates were found to be similar for both techniques.13 In addition, Paggi et al.12 found no difference between the methods in terms of procedure duration, cecal intubation rate, and patient satisfaction, while Lee et al.16 found better patient comfort in the one-person method. In pediatric patients, Chen et al. concluded that the one-person method was safer than the two-person method.26
In our study, we focused on three parameters that affect the quality of the procedure and patient comfort, total procedure time, physician's assessment of ease of the procedure, and patient comfort. In addition, the gag reflex, which was not included in the ESGE guidelines, was taken as a variable criterion. Although most endoscopists are not generally interested in laryngeal evaluation during upper gastrointestinal endoscopic examinations, to avoid triggering the gag reflex, the laryngeal assessment was performed as quickly as possible in our study, vocal cords were observed in approximately 55% of patients, and no significant difference was found between the two groups. In the physician's evaluation, the ease of the procedure was satisfactory in both groups (98.8%), and the mean scores (3.26±0.603 and 3.25±0.64, p>0.05) were almost the same. The total time of the procedure was lower in the first group; thus, for coordinating the movements, the nurse-assisted method required more time than the one-person method, but this difference was not statistically significant. Therefore, according to physician-dependent evaluation criteria, the assisted method does not prolong the duration of the procedure and does not increase the difficulty of the procedure.
Evaluation of patient satisfaction is an important issue in healthcare services and one of the quality criteria, so patient satisfaction scores should be at an acceptable level.1 In a few studies, discomfort during the procedure was identified as the main cause of patient dissatisfaction.24,25 In previous studies, the patient satisfaction rate was found to be approximately 95%.27,28 The procedure was described as uncomfortable by 4.6% of the patients in our study, and the patient satisfaction rate (95.4%) was found to be consistent with the literature. More gag reflex was observed in our study compared to those reported in the literature29 due to IV sedation not being performed. The gag reflex is an important factor in terms of patient comfort, which was less observed in the nurse-assisted method. Even if there are similar rates of patient satisfaction (94.8% vs 96%, p>0.05), compared to the single endoscopist method, the nurse-assisted technique provides less gag reflex (54.4% vs 45.2%, p=0.04) and higher satisfaction score (2.98±0.79 vs. 3.11±0.78, p=0.043), hence the alternative nurse-assisted technique improves the quality of the endoscopic procedure. The risk of adverse events is low in upper GI endoscopy; adverse event rates were reported as 0.5% to 0.01% in previous studies.30 Our study has a low rate of adverse events similar to the literature; only mucosal lacerations of the hypopharynx were observed in six patients, and no major adverse events were observed.
In the single endoscopist technique, the left hand controls the up/down wheel, left/right angulation wheel, insufflation, water, and suction buttons, while the right hand is responsible for advancing and withdrawing the endoscope and its axial rotation. Therefore, when using the distal tip of the endoscope with the right-hand, control section of the endoscope remains under the control of only the left hand; this condition may reduce maneuverability. In the nurse-assisted technique, because the nurse is responsible for advancing and withdrawing the endoscope and its axial rotation, the maneuverability of the endoscopist increases. Thus, the left hand holds the control section and controls the up/down deflection wheel, while endoscopist's right hand easily controls the left/right deflection wheel. We think that the increase of maneuverability with this method causes the difference between the two methods.
This study has several potential limitations. The most important are that the study design was open labeled, the two methods were not compared in terms of adenoma or dysplasia detection rates, and subgroup analyses were not performed between different physicians. Other limitations of the study were as follows: this was a single-center study, and waiting time (pre-procedural in-hospital) before the endoscopy, the patients’ educational and socio-cultural levels were not evaluated. The procedure time determined in our study was found to be shorter than the time specified in the ESGE guidelines.22 We think this reflects that the endoscopists are very experienced and that the procedure is performed serially to avoid patient intolerance from performing the procedure without sedation.
In conclusion, we found that the assisted endoscopic technique provides more comfort and less gag reflex, without prolonging processing time or making the procedure more difficulty. Thus, this alternative technique provides superior patient comfort compared to the standard technique. Nurse-assisted endoscopy is a safe and effective method for routine esophagogastroduodenoscopy. The advantage of working with an experienced nurse as the endoscopist's assistant is that it provides increased organizational flexibility for performing the procedure. To the best of our knowledge, this is the first study evaluating assisted endoscopy technique-related comfort and the ease of the procedure.
FundingNone.
Conflict of interestThe authors declare that they have no conflict of interest.