Neurofibromatosis type 1 (NF1), or von Recklinghausen disease, is an autosomal dominant-inherited disease caused by mutations in the NF1 gene located at chromosome 17q11.2.1 Its incidence is approximately 1/3000 newborns and it occurs in all races and ethnic groups and in both genders. The mutation is “de novo” and not inherited in 50% of cases.
For diagnosis, 2 or more of the following criteria must be met: 6 or more café-au-lait spots larger than 5mm in prepubertal patients and larger than 15mm in postpubertal patients; 2 or more neurofibromas of any type or 1 plexiform neurofibroma; axillary or inguinal freckling (Crowe's sign); optic nerve gliomas; 2 or more benign iris hamartomas (Lisch nodules); distinctive osseous lesions (sphenoid dysplasia, thinning of the long bone cortex with or without pseudoarthrosis); first-degree relative (parent or sibling) with NF1.2
There is relatively common association between neurofibromatosis and gastrointestinal tumours, which may appear in 3 different ways: (a) stromal tumours (neurofibromas or leiomyomas), which is the most common form of presentation, located in the stomach or small intestine and more rarely in the colon3; (b) neuronal hyperplasia and ganglioneuromatosis; (c) endocrine tumours in the duodenum and peri-ampullary region.4–6
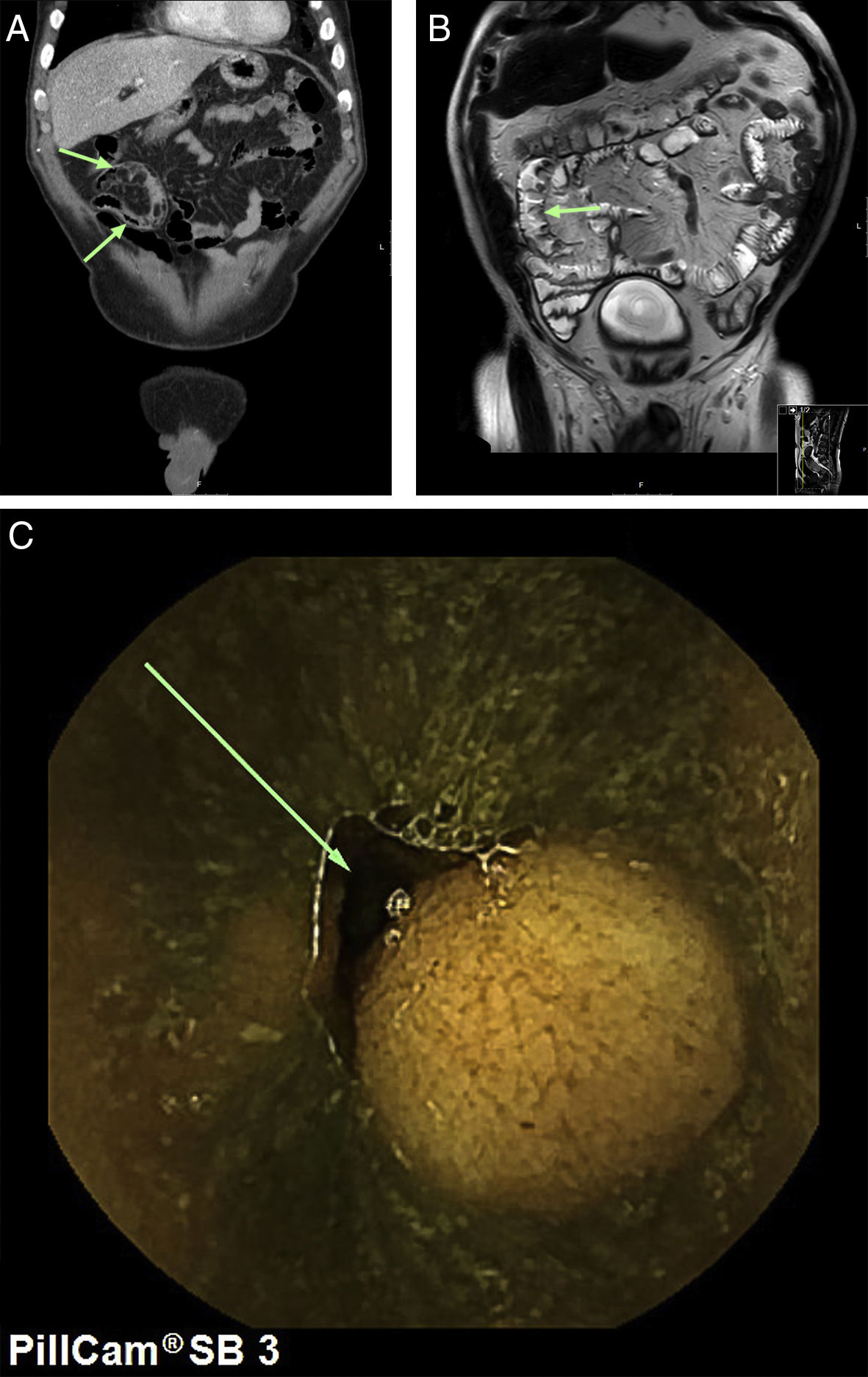
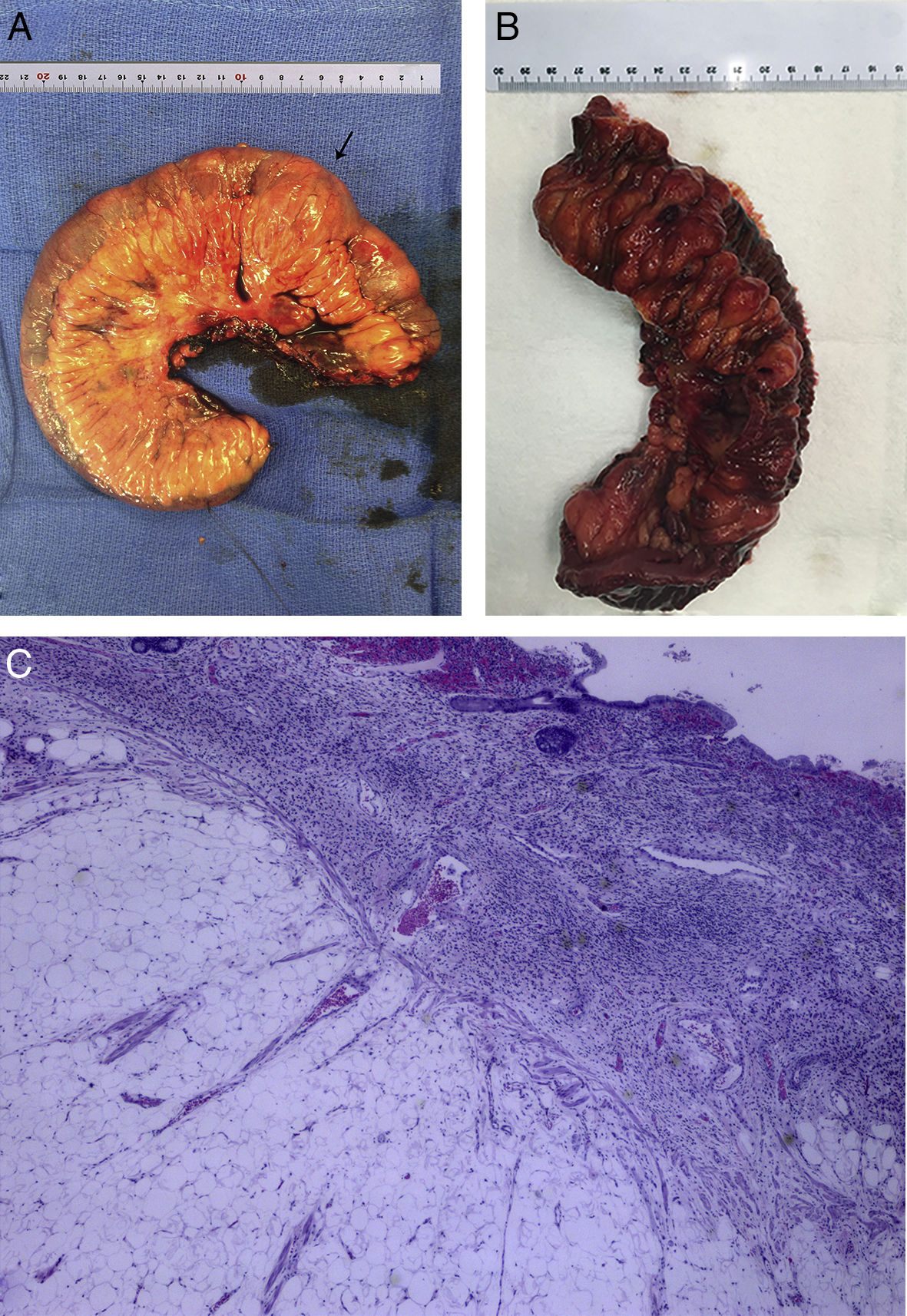
Our case study is a 69-year-old male patient diagnosed with NF1 who was admitted with asthenia and severe anaemia (haemoglobin 6.4g/dl) together with self-limiting episodes of rectorrhagia. A gastroscopy and colonoscopy was performed with no relevant findings. Computed tomography (CT) scans of the chest and abdomen, magnetic resonance imaging (MRI) scans of the intestines and a capsule endoscopy were done, showing tumours in the middle portion of the ileum consistent with his underlying disease (Fig. 1A–C). It was decided to schedule surgery (segmental resection of the ileum with end-to-end anastomosis (Fig. 2A).
The patient's initial progress was favourable and he was discharged 5 days after surgery. However, 16 days after surgery, the patient was re-admitted due to acute abdominal pain and, as a result, an abdominal CT scan was performed, showing fluid collection near the anastomosis. The patient underwent emergency surgery and localised purulent peritonitis was found that was probably due to anastomatic leakage, which was treated with parenteral nutrition and catheter drainage of the leak. A control CT scan was performed, which showed improvement of the fluid collection, and the patient was discharged. During outpatient follow-up, the patient was asymptomatic with no recurrent bleeding.
The results of the pathology analyses performed on the surgical specimen showed multiple nodular lesions with diffuse proliferation of mesenchymal stromal (stem) cells of neural lineage and chronic inflammation of the basal lamina propria with distortion and displacement of adjacent glandular epithelium (Fig. 2B). They also showed dehiscence of the mucosal muscle fibres and overgrowth of adipose tissue into the submucosal layer with congested vessels and isolated neural structures within the overgrowth. The muscle layer showed nerve plexus hypertrophy. No evidence of nuclear atypia, mitosis or necrosis was observed. No lymph nodes were identified in mesenteric fat. Both surgical margins were free from tumour infiltration. The immunohistological study showed a strong positive reaction for S100 in the mesenchymal cell proliferation area, with a negative reaction for AE1/AE3, CD117 (c-Kit), DOG-1 and actin, and a nuclear proliferation index (Ki-67) of 10–15% (Fig. 2C). These morphological and immunophenotypical changes were compatible with multiple benign neurofibromas.
Neurofibromatosis is a disease in which affected patients are more prone to develop benign and malignant tumours compared with the rest of the population. It can be divided into 2 types: neurofibromatosis type 1 and type 2, which involve 2 different chromosomes, 17 and 22, respectively. Diagnostic criteria are different for each type of neurofibromatosis.
The association between NF1 and gastrointestinal complications affects a variable percentage of patients, ranging between 12 and 25%,3 and tends to affect middle-aged patients in relation to tumours that develop along the gastrointestinal tract, appearing most commonly in the stomach and small intestine and more rarely in the oesophagus and colon.7
In our case, the patient's condition had been latent for over a year with self-limiting rectorrhagia and a colonoscopy had showed no warning signs. However, 9 months later, all signs of rectorrhagia disappeared and he then had symptoms of asthenia and severe anaemia, resulting in thorough imaging studies (abdominal CT scan, intestinal MRI and capsule endoscopy), which revealed multiple tumours in the ileum. It was decided that surgery was the only course of treatment to correct the anaemia and it was also impossible to rule out malignancy without surgery. Chemotherapy was ruled out as the surgical specimen analysed following surgery showed no malignant potential.
These findings demonstrate the need for early diagnosis in this type of patients, who may sometimes be asymptomatic. However, in other cases, patients may develop gastrointestinal bleeding, abdominal pain, palpable mass, obstruction or even malignancy due to sarcomatous degeneration.3,8 This should promote early action to prevent major complications.
Please cite this article as: Samartín Toimil C, Gay Fernández AM, Tardío Baiges A, Primo Álvarez JC, Casal Núñez JE. Hemorragia digestiva por neurofibromas en íleon. Gastroenterol Hepatol. 2018;41:267–269.