Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis complex,1 the target organs of which are the lungs. It primarily affects the populations of developing areas, causing 2,000,000 deaths per year.1,2 Extrapulmonary tuberculosis is derived from the pulmonary disease and primarily affects immunosuppressed individuals, particularly HIV patients.1,3 The most commonly affected extrapulmonary tissues are the pleura, the lymph nodes and the urinary system.1 The rarity of liver involvement coupled with its nonspecific symptoms make it difficult to diagnose, meaning that histological confirmation is often required.1,2,4 As in our case, it can be confused with primary or metastatic liver tumours.
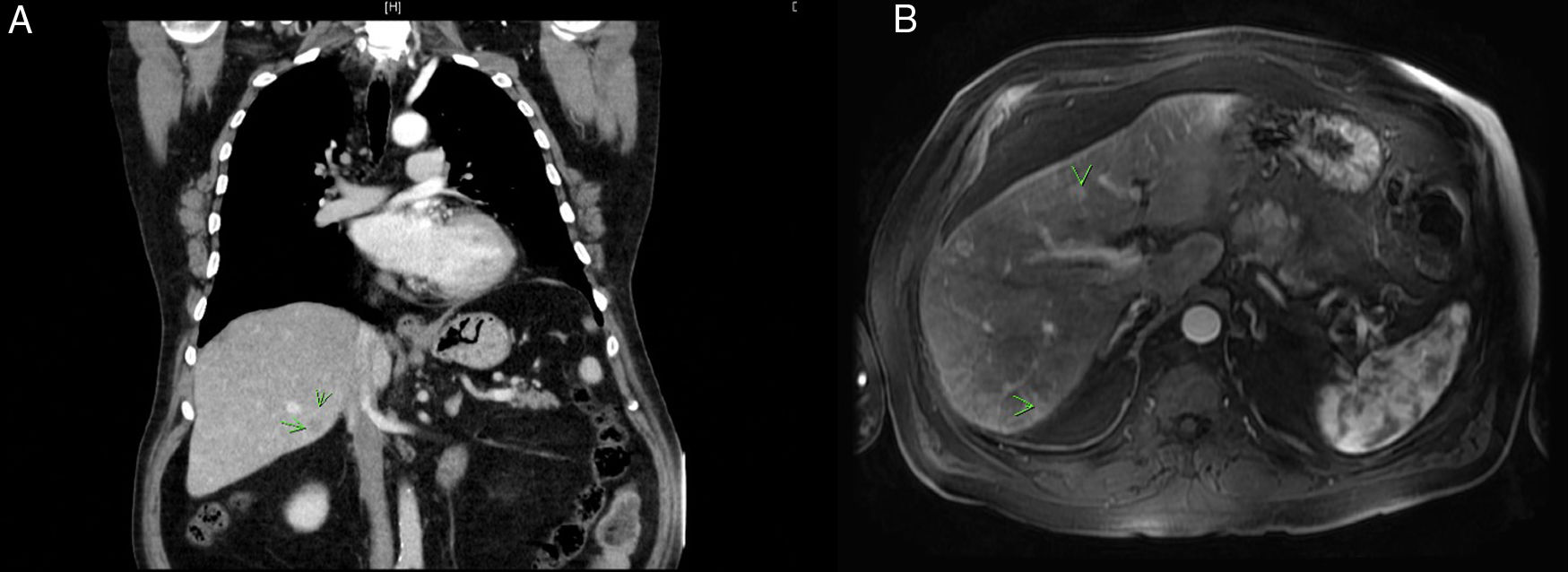
We present the case of a 69-year-old male with a history of smoking and alcoholism, diabetes mellitus, hypertension, dyslipidaemia and a rectal adenocarcinoma in 2013 who received neoadjuvant chemotherapy and radiotherapy, followed by surgery with a pathological finding of T3N0M0, receiving adjuvant therapy with six cycles of Xeloda®. The patient subsequently remained free of clinical and radiological disease and, at the fourth year of follow-up, exhibited a hypodense low attenuation lesion on the CT scan (Fig. 1A) in segment VI of the liver. Given his oncological history, liver metastasis of colorectal origin was the first possibility to be considered. The study was extended with an abdominal ultrasound, which revealed multiple nodular lesions measuring up to 2 cm in diameter, and an MRI (Fig. 1B), which showed hyperintense, non-calcified bilobar lesions in T1 Fat-Sat with contrast in arterial phase, in segments II, ivA, ivB, VIII and VI, all suggestive of liver metastases, and CEA at the upper limit of normal. The case was submitted to the digestive tumour committee, and it was decided to start systemic chemotherapy with six cycles of FOLFIRI plus cetuximab. New CT and MRI scans at four months showed partial response to chemotherapy with a reduction in the size of the hepatic space-occupying lesions (SOLs), except for one in segment II and one in segment VI. It was decided to perform rescue surgery on the liver, finding five subcapsular lesions suggestive of subcentimetric metastases in segments ivA, ivB, V, VI and VIII, as well as two intraparenchymatous lesions in segments II and ivB. Metastasectomy of the subcapsular lesions was performed and microwaves were applied to the intraparenchymatous lesions. The histological result of all the samples showed granulomatous nodular lesions centred by necrosis of a caseous appearance surrounded by epithelioid histiocytes, some multinucleated giant cells and, peripherally, fibrosis with Ziehl-Neelsen staining; no acid-alcohol-resistant bacilli were detected. Neoplastic cells were not found in any of the samples. The patient was assessed by the Infectious Diseases department and started treatment with isoniazid, rifampicin and pyrazinamide for nine months with good drug tolerance. At the end of treatment, a CT scan and MRI showed complete resolution of the described lesions.
Hepatic tuberculosis is an uncommon form of tuberculosis, accounting for 1% of all cases of abdominal tuberculosis.1,2 It can present as disseminated tuberculosis with synchronous pulmonary involvement, diffuse liver involvement without pulmonary disease, or in the form of a solitary liver abscess or tuberculoma.1,2 The low incidence of primary hepatic tuberculosis is related to low oxygen levels in hepatocytes, meaning that this tissue does not provide a favourable environment for Mycobacterium tuberculosis.4 The first reference in the literature to hepatic tuberculosis was made by Bristowe in 1858.2 It can clinically manifest with nonspecific symptoms such as fever, abdominal pain, weight loss, hepatomegaly or even abnormal liver function tests1,2 or, as in our patient, an incidental finding in a histological study expected to show metastasis of colorectal origin. Its diagnosis is complex and highly specific but it is uncommon to find Koch's bacillus in histological material.2 Given the nonspecificity of the characteristics of imaging tests, it can be mistaken radiologically for primary or secondary liver tumours, as in our case.2,5 Once diagnosed, the objective is to start tuberculosis treatment as soon as possible, achieving resolution of the lesions in 6–12 months.2,3
In conclusion, although tuberculosis is now uncommon in our setting, and extrapulmonary tuberculosis even more so, it should be considered in the differential diagnosis of primary or secondary liver tumours in patients with a history of cancer.
FundingThis study was conducted without a grant.
Please cite this article as: Soto-Darias IC, Morales-Hernández A, García-Romera Á, Bravo-Gutiérrez A, Alarcó-Hernández A. Tuberculosis hepática simulando metástasis de cáncer colorrectal. Gastroenterol Hepatol. 2020;43:90–91.