Acute liver failure is defined as the sudden and severe deterioration of liver function, in the form of coagulopathy and encephalopathy, in patients without previous liver disease. It is a rare condition, with an incidence of fewer than 10 cases per million population per year. Causes include invasion of the liver by a malignant neoplasm, although it is very rare for acute liver failure to occur.1,2
Case reportThis was a 50-year-old woman with no relevant medical history except for 10 cigarettes and 40 g of alcohol per day. She came to the accident and emergency department with a month-long history of right mechanical low back pain, associated with slight abdominal distension. Physical examination revealed only frank mucocutaneous jaundice.
Laboratory tests showed haemoglobin 12.2 g/dl, leucocytes 14.24 thousand/mm3, platelets 86 thousand/mm3, neutrophils 10.89 thousand/mm3, INR 2.23, prothrombin activity 33%, creatinine 0.9 mg/dl, sodium 126 mEq/l, potassium 4.6 mEq/l, total bilirubin 12.8 mg/dl, GOT/AST 373 U/l, GPT/ALT 110 U/l, GGT 183 U/l, LDH 890 U/l and alkaline phosphatase 316 U/l. Ascitic fluid showed leucocytes 123 mm3, glucose 89 mg/dl, protein 1 g/dl, albumin 0.5 g/dl and a serum-ascites albumin gradient of 1.8 g/dl.
Hepatotoxins, hepatotropic viruses, spontaneous bacterial peritonitis and other infectious foci were ruled out. Autoimmunity showed IgG 2250 mg/dl, IgA 750 mg/dl and IgM 845 mg/dl, with negative ANA, AMA, anti-LKM-1 and anti-SLA.
Abdominal ultrasound showed hepatomegaly with lobulated contours and very heterogeneous echotexture, patent portal vein, recanalisation of the umbilical vein and moderate ascites.
Despite supportive treatment (albumin expansion, systemic corticosteroids and antibiotic therapy), the patient deteriorated, both clinically and analytically, with worsening of coagulopathy, acute kidney injury, hyponatraemia and grade I encephalopathy.
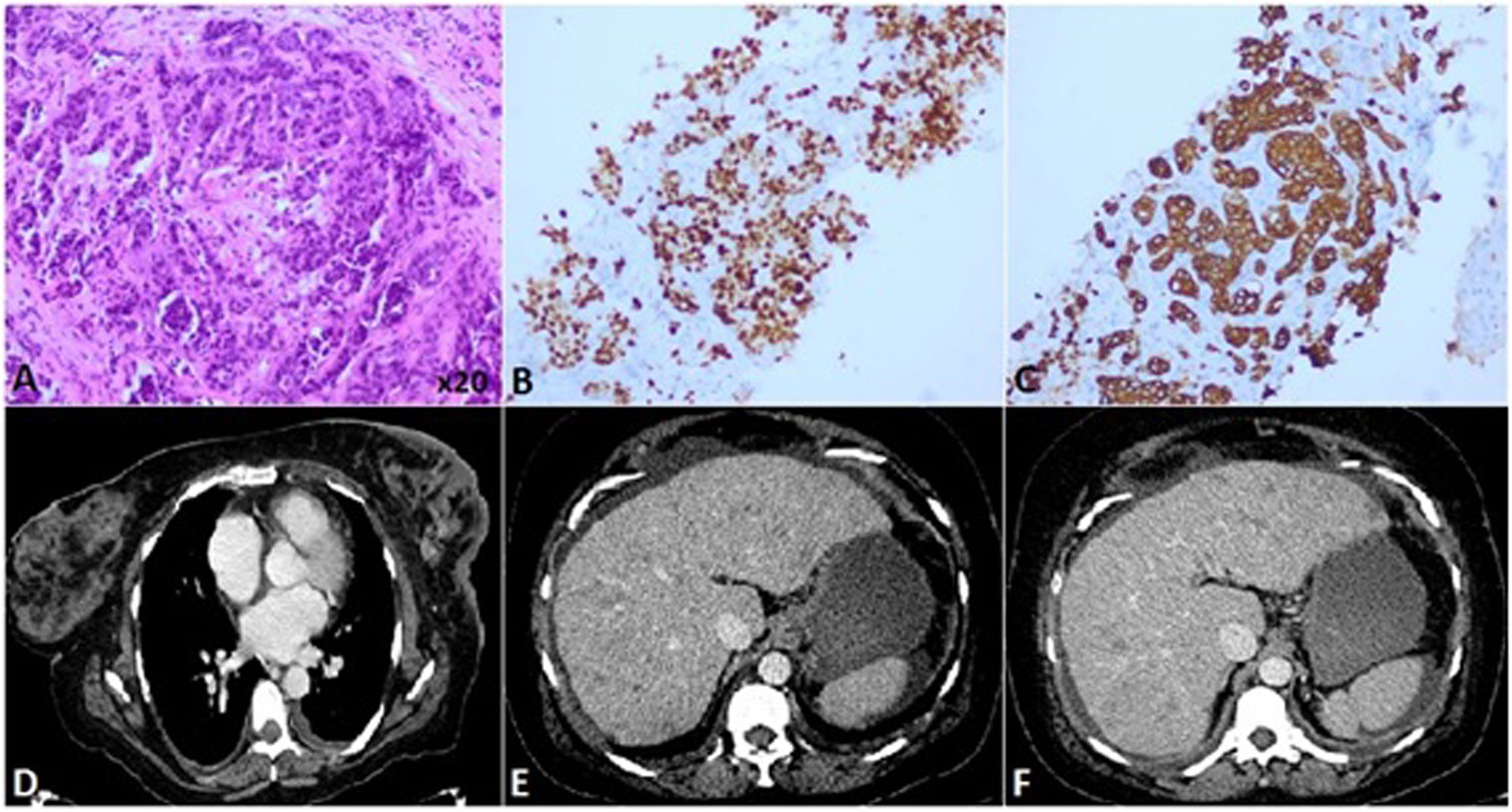
As acute on chronic liver failure was suspected, a transplant centre was contacted. Pathology examination of transjugular liver biopsy revealed “liver parenchyma invaded by malignant epithelial neoplasm. Immunohistochemistry: CK7+; CK20−; CK19+; TTF-1-; glypican 3-; arginase 1-; GATA-3+, oestrogen and progesterone receptors negative, c-erbB2 not assessable. Findings consistent with liver invasion by carcinoma of mammary origin” (Fig. 1). Ascitic fluid cytology was negative for malignancy.
A) Invasion of the liver by invasive ductal carcinoma (haematoxylin-eosin). B) Immunohistochemistry with GATA3 expression. C) Immunohistochemistry with CK19 expression. D) CT with intravenous contrast, arterial phase. Thickening of the skin and nodular lesions on the left breast. E) and F) Portal phase. Hypodense lesions distributed throughout the liver parenchyma, hepatomegaly, ascites.
Computerised axial tomography showed multiple focal liver lesions in both lobes, consistent with metastasis, as well as alterations in the left breast suggestive of malignancy (Fig. 1). Mammography showed a left breast nodule suspicious for malignancy with skin thickening in relation to oedema and/or inflammatory carcinoma, without suspicious lymph nodes (BI-RADS 5).
Progress continued to be poor, and as liver transplantation was impossible due to massive metastatic invasion, the patient died 10 days after admission.
DiscussionWe have presented a case of fulminant hepatic failure, most commonly caused worldwide by hepatotropic virus infections, and by drug toxicity specifically in the West. Less common are ischaemic hepatitis, autoimmune hepatitis, Wilson’s disease or massive tumour invasion.1,2
After lymphatic involvement, the liver is the organ most frequently affected by haematogenous spread of solid malignancies, sometimes causing massive intrasinusoidal invasion. The main primary tumours which metastasise to the liver are colorectal carcinoma, breast carcinoma, melanoma, neuroendocrine tumours, lung carcinoma and gastric carcinoma.3,4
In cases of liver involvement due to breast carcinoma, the metastatic pattern usually consists of discrete nodules, with diffuse metastatic invasion and acute liver failure being rare. However, diffuse metastatic invasion is the form most commonly associated with acute liver failure.5
This clinical case reminds us that tumour invasion can be a cause of acute liver failure and, although uncommon, it should be considered in the differential diagnosis in patients without evidence of viral hepatitis or consumption of hepatotoxic drugs and with non-specific findings in imaging tests, particularly if there is a history of cancer. In addition, it can behave as a “pseudocirrhosis”, in which the desmoplastic reaction induced by the invasive cancer leads to collagenisation of the liver parenchyma, resulting in hepatocyte atrophy, which induces acute liver failure and signs of portal hypertension.2
It is therefore necessary to maintain a high index of suspicion, and in these cases a pathology study is required to reach a definitive diagnosis,3 although in patients with heterogeneous livers on ultrasound it is important to perform other imaging tests beforehand, preferably with contrast.
Ethical considerationsThis work did not involve the use of human subjects, as the information has simply been obtained in a completely anonymous manner from a patient’s medical records following the protocols of our work centre on the publication of patient data.
FundingNo funding was received for this study.
Conflicts of interestThe authors declare that they have no conflicts of interest.