To calculate the number of analytical tests and blood volume drawn during the first 24h of admission to the Intensive Care Unit (ICU). To analyse values of basal haemoglobin and at 24h, relate them to blood loss, weight variation, and scoring system.
MethodAn observational descriptive pilot study. Variables studied: age, sex, diagnosis on admission, analytical tests extracted, waste quantity before the extraction of samples, total volume blood extracted in 24h, weight variation, APACHE, SAPS, basal haemoglobin and at 24h. Statistical analysis with SPSS vs 20.0. Variables correlation sex, weight variation, the number of analytical tests and haemoglobin change.
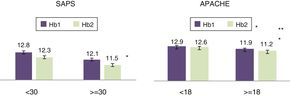
ResultsThe study included 100 patients. The average number of extractions per patient/day was 7.2 (±2.6). The average waste quantity was 32.61ml (±15.8). The blood volume used for determinations was 48.18ml/24h (±16.74). The haemoglobin value decreased in the first 24h of admission, being higher in men (P<0.05). The scoring systems were statistically significant for levels of haemoglobin (Hb1 –0.3; P=0.001; Hb2 –0.4; P=0.001).
ConclusionsOf the total volume of blood extracted in ICU, 40% belongs to a volume of waste and 60% of blood is used for analytical tests. There is a decrease in haemoglobin exists 24h after admission of the critical patient. Statistically, it has not been possible to demonstrate its relation with the number of analytical tests.
Calcular el número de analíticas y volumen de sangre extraído durante las primeras 24h de ingreso en la unidad de cuidados intensivos (UCI). Analizar valores de hemoglobina basal y a las 24h, relacionarlas con volumen de sangre extraído, balance ponderal e índices de gravedad.
MétodoEstudio descriptivo, observacional y prospectivo. Variables de estudio: edad, sexo, diagnóstico de ingreso, analítica extraída, cantidad de desecho antes de la extracción de muestras, volumen de sangre total extraída en 24h, balance ponderal, índices de gravedad, hemoglobina basal y a las 24h. Análisis estadístico realizado mediante SPSS vs.20.0. Se han calculado las correlaciones de las variables sexo, balance, número de analíticas y variación de hemoglobina.
ResultadosLa muestra estuvo formada por 100 pacientes. El número de extracciones medio por paciente/día fue de 7,2 (±2,6). La cantidad media de desecho fue de 32,61ml (±15,8). El volumen medio de sangre utilizado para determinaciones fue de 48,18ml (±16,74). El valour de la hemoglobina disminuyó las primeras 24h de ingreso, siendo mayor en los hombres (p<0,05). No se pudo demostrar que el número de analíticas estuviera relacionado con la diferencia de hemoglobina a las 24h. Los índices de gravedad tuvieron significación estadística en cuanto a los niveles de hemoglobina (Hb1: –0,3; p=0,001; Hb2: –0,4; p=0,001).
ConclusionesDel volumen total de sangre extraída en UCI, el 40% pertenece a volumen de desecho y el 60% a sangre utilizada para analíticas. Existe una disminución de la hemoglobina a las 24h de ingreso del paciente crítico, pero no se ha podido demostrar estadísticamente su relación con el número de analíticas.
Anaemia is the most frequent haematological pathology in patients admitted to an ICU. The causes are multifactorial, and the main mechanism is the increase in blood loss. The different reasons described for this include iatrogenic mechanism involved in successive extractions for analysis. During the first 24h of admission to an ICU a large amount of blood is extracted from patients, and a large fraction of the extracted blood is eliminated.
This study offers a reflective view of managing the volume of blood extracted from critical patients. It centres on analysing the volume of blood extracted from critical patients during the first hours of admission, making it possible to analyse the repercussions this has in our patients.
Implications of the studyUndertaking an analysis of the situation of medical practice will make it possible to detect the real levels of blood loss and raise the awareness of the professionals involved of the importance of rationalising extraction for analyses, to reduce blood loss and prevent iatrogenic anaemia.
The World Health Organisation (WHO) defines anaemia as a haemoglobin (Hb) level below 13g/dl in men and 12g/dl in women.1 The prevalence of anaemia in critical patients is high, and from 40% to 70% of them require blood transfusions.2 Some studies show that two thirds of the patients admitted to an intensive care unit (ICU) have a Hb concentration lower than 12g/dl on the day of their admission.3,4
Intrahospital acquired anaemia (IAA) is one of the complications of critical patients. The cause of this is complex and multifactorial; it may be due to haemodilution, alteration in iron metabolism, nutritional deficiencies, a reduction in the half-life of erythrocytes or a fall in their production, inappropriate production of erythropoietin and blood losses secondary to haemorrhage or the taking of samples.5 It is associated with negative outcomes, such as prolonged hospitalisation and increased mortality.6
Blood is extracted every day in ICUs for diagnostic and therapeutic purposes. Some authors associate IAA with the high number of blood extractions for diagnostic purposes.7–9 These analyses are fundamental for the management of critical patients; nevertheless, from 50% to 60% of these extractions are considered unnecessary.10 Rhagavan and Marik state that repeated phlebotomies may cause a loss of 25–40ml blood per patient per day.11 Vincent et al.12 state that the highest volume of blood is extracted from critical patients during the first 24–48h. As nurses we ask ourselves what repercussion blood losses due to diagnostic phlebotomies may have on our patients? The aims of this study are:
To determine the number of times blood samples are taken during the first 24h of admission to an ICU.
To determine the total volume of blood that is extracted during the first 24h of admission: the total volume that is used for analytical determinations and the volume that is eliminated.
To analyse basal Hb values and those at 24h.
To relate Hb values at 24h with blood volume, pathology at admission, the weighted balance at 24h and severity indexes.
MethodDesign. This is a descriptive, observational and prospective study.
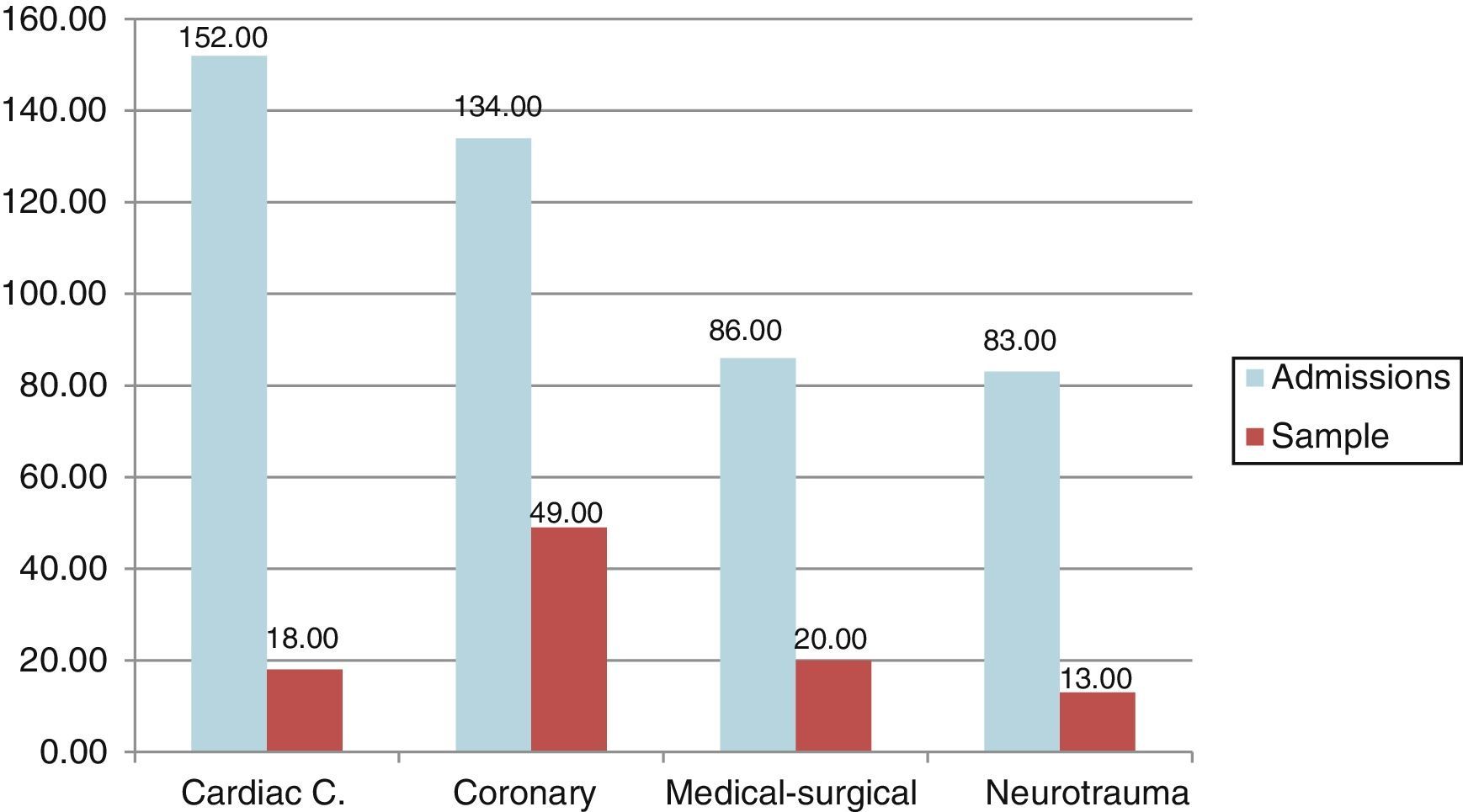
Scope. This study was performed from January to June 2016, in the Hospital Universitario Son Espases, Palma de Mallorca. This hospital ICU has 32 beds divided among 4 units: Heart Surgery, Coronary patients, Medical-surgical and Neurotrauma. Data gathering period: from February to April.
Inclusion criteria. All of the patients admitted to any of the ICU units, older than 18 years old, with a stay of at least 24h.
Exclusion criteria. Patients with active bleeding (those who presented detectable or diagnosed blood losses), after cardiac surgery with a blood loss greater than 1.5ml/kg/h during six consecutive hours within the first 24h, patients with coagulation pathologies or ones that had received haemoderivatives during the study period.
Calculation of sample size and selection. It was calculated that a sample of 100 patients would be sufficient to estimate, at 95% confidence and a precision of ±2 units, the populational average volume in millilitres of blood with values that are expected to be above 20ml/day and with a standard deviation of approx. 10ml. To make this calculation the millilitres of blood extracted from patients in a routine day and not the day of admission was taken as the standard. To evaluate the factors which influence the total volume extracted and accepting an alpha risk of 0.05 and a beta risk lower than 0.2, in a bilateral comparison, 100 subjects would be necessary to detect a difference of at least 5ml.
Variables studied. Age, sex, diagnosis at admission, type of analytical sample extracted (gasometry, biochemistry, haematology, blood culture, coagulation), number of analyses in 24h, amount eliminated before the extraction of samples and total volume of blood extracted in 24h, Hb at admission (Hb1) and at 24h (Hb2), weighted balance of the first 24h and severity indexes: Acute Physiology and Chronic Health Evaluation (APACHE) and the Simplified Acute Physiologic Score (SAPS). The severity scales are used to characterise the severity of patient disease and organic dysfunction, as well as to evaluate clinical practice. In our ICU two morbimortality scales are used for all of the patients, given that the combination of several scales may help to gain a more complete vision of patient situation.
A data sheet was prepared to record the following variables: date of admission, clinical history number, number and type of analyses, volume eliminated and extraction technique. In our ICU there is no protocol for the extraction of samples using a catheter and each professional does so according to their own criterion, knowledge or professional practice. Charts were filled out by the nurse who had extracted blood from the patient during the first 24h of admission. These charts were then stored in a folder located in each unit, and they were transferred every week to the database. Sociodemographic variables, pathology at admission, Hb and severity indexes were copied from the clinical history by the researchers, with the aim of facilitating data recording.
Data analysis. Data were filtered using range tests (detecting possible values) and crossed logical fields to detect inconsistencies between answers. A descriptive analysis was undertaken of the quantitative variables and the average±standard deviation was calculated. Spearman's correlation coefficient (Rho) was calculated for the variables of sex, weighted patient balance and the number of analytical samples together with variation in Hb (t-test) and severity indexes. Values of P<0.05 were considered significant. Statistical analysis was undertaken using the SPSS vs. 20.0 programme.
Ethical considerations. The study was presented to and then approved by the Hospital Research Committee. No modifications were made to care or experimental procedures, according to the international norms stipulated in the Helsinki Declaration (1964). Data confidentiality was guaranteed (Data Confidentiality Law LOPD 15/99).
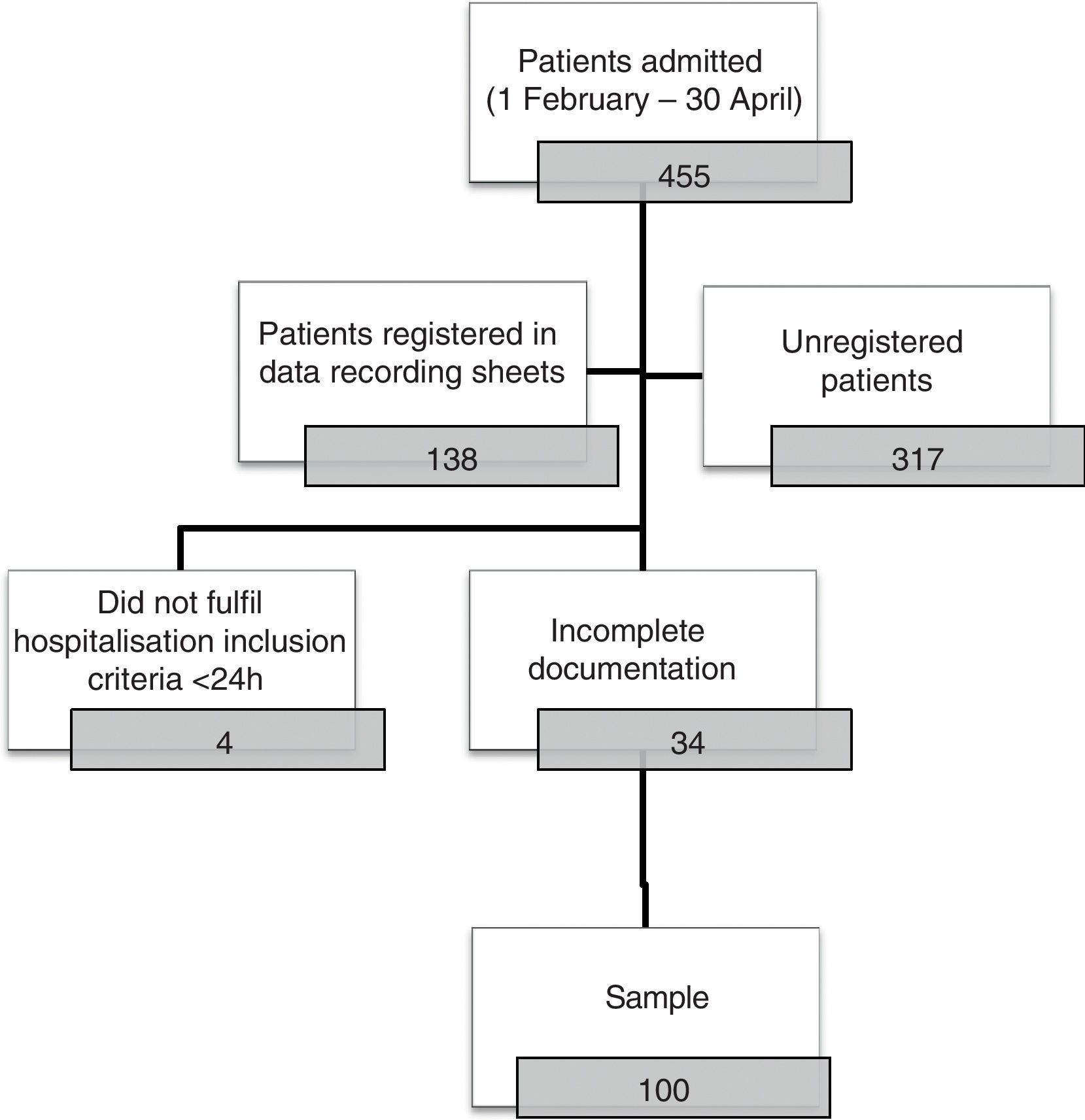
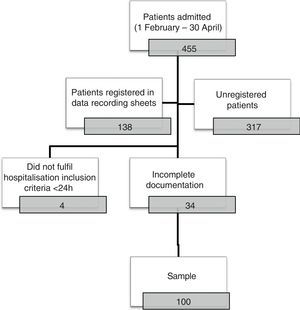
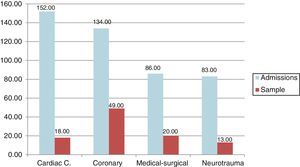
ResultsThere were 455 admissions during the data-gathering period. The final sample was composed of 100 patients; Fig. 1 shows the sample selection algorithm. Fig. 2 shows the number of admissions to the ICU grouped according to unit as well as the patients included in the study. The sample studied was representative of the 455 admissions in the ICU in terms of age, sex and number of patients, at a confidence level of 95% and a precision of 4%. 58% were men and 42% were women, with an average age of 63.7 years old (±13.6). The average APACHE and SAPS values were 18.7 (±9) and 34.8 (±13), respectively, with an overall mortality of 10–25%.
The average number of analytical samples taken per ICU patient in the first 24h after admission was 7.2 (±2.6). The medical-surgical unit was the one with the lowest number of extractions (X¯=6.7) and the one with the highest number was the coronary unit (X¯=7.6), where P=0.57.
The average amount of blood eliminated in the 24h before extraction of the sample was 31.61ml (±15.8). The units which eliminated the largest amounts of blood were cardiac surgery (X¯=36.16 ml) and the coronary unit (X¯=33.89 ml); the ones that eliminated the lowest amounts were neurotrauma (X¯=28.38 ml) and the medical-surgical unit (X¯=23.73 ml). These differences are statistically significant (P=0.048).
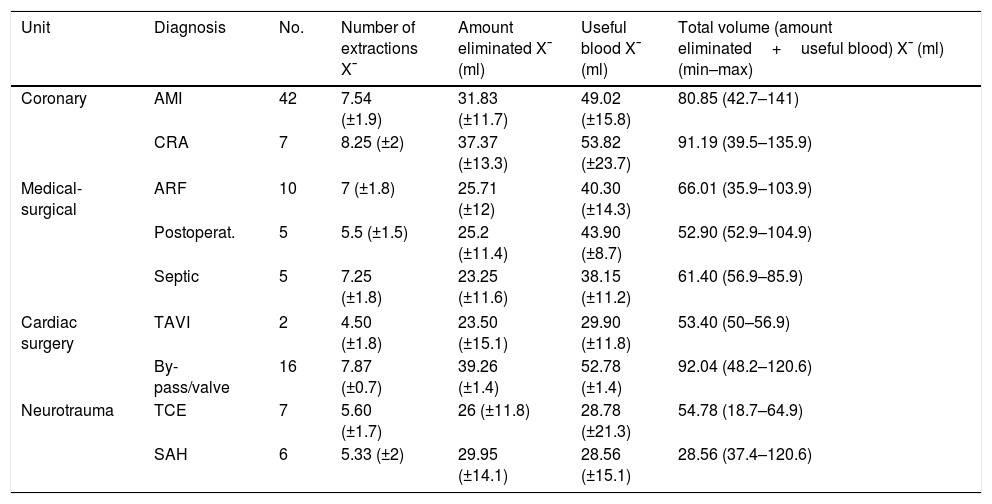
The average volume of useful blood that was extracted in samples for analysis amounted to 48.1ml (±16.7). The average total volume extracted in 24h (eliminated blood+useful volume) amounted to 80.7ml (±26.8). The patients admitted to the coronary unit had a statistically significant higher total volume of blood extracted than those in the other units (P=0.007). Table 1 shows the different volumes recorded according to unit and pathology at admission.
Number of blood extractions, volume eliminated, useful volume and total volume.
| Unit | Diagnosis | No. | Number of extractions X¯ | Amount eliminated X¯ (ml) | Useful blood X¯ (ml) | Total volume (amount eliminated+useful blood) X¯ (ml) (min–max) |
|---|---|---|---|---|---|---|
| Coronary | AMI | 42 | 7.54 (±1.9) | 31.83 (±11.7) | 49.02 (±15.8) | 80.85 (42.7–141) |
| CRA | 7 | 8.25 (±2) | 37.37 (±13.3) | 53.82 (±23.7) | 91.19 (39.5–135.9) | |
| Medical-surgical | ARF | 10 | 7 (±1.8) | 25.71 (±12) | 40.30 (±14.3) | 66.01 (35.9–103.9) |
| Postoperat. | 5 | 5.5 (±1.5) | 25.2 (±11.4) | 43.90 (±8.7) | 52.90 (52.9–104.9) | |
| Septic | 5 | 7.25 (±1.8) | 23.25 (±11.6) | 38.15 (±11.2) | 61.40 (56.9–85.9) | |
| Cardiac surgery | TAVI | 2 | 4.50 (±1.8) | 23.50 (±15.1) | 29.90 (±11.8) | 53.40 (50–56.9) |
| By-pass/valve | 16 | 7.87 (±0.7) | 39.26 (±1.4) | 52.78 (±1.4) | 92.04 (48.2–120.6) | |
| Neurotrauma | TCE | 7 | 5.60 (±1.7) | 26 (±11.8) | 28.78 (±21.3) | 54.78 (18.7–64.9) |
| SAH | 6 | 5.33 (±2) | 29.95 (±14.1) | 28.56 (±15.1) | 28.56 (37.4–120.6) | |
SAH: subarachnoid haemorrhage; AMI: acute myocardial infarction; ARF: acute respiratory failure; CRA: cardiorespiratory arrest; Postop: after abdominal surgery; TAVI: transcatheter aortic valve implant; CET: craneoencephalic trauma.
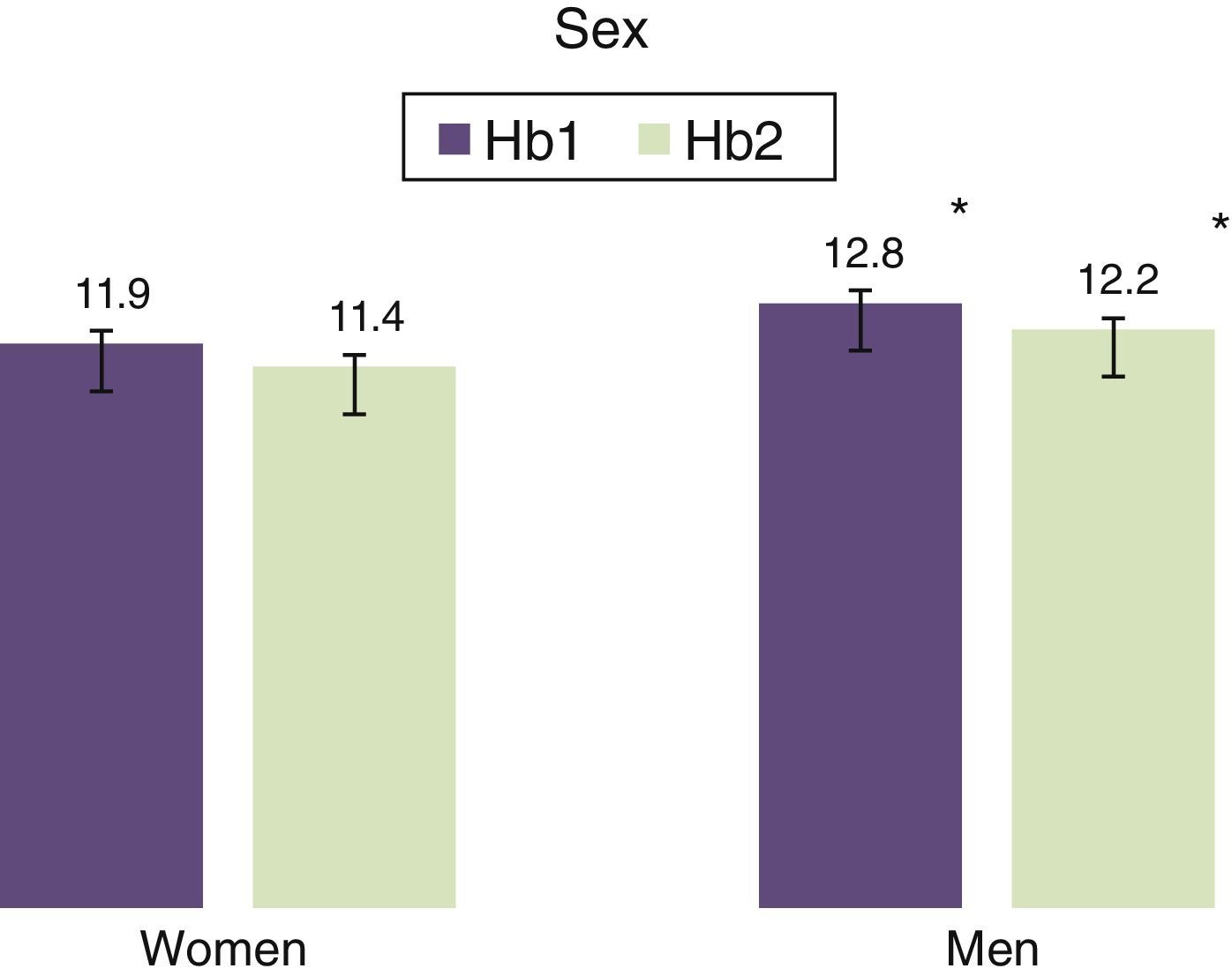
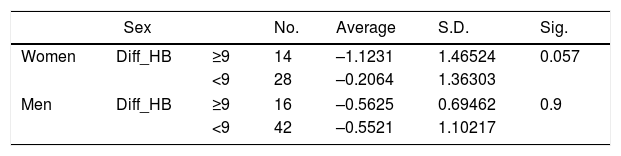
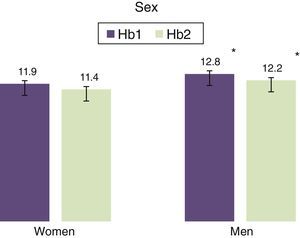
Statistically significant differences exist between men and women in terms of basal Hb and Hb at 24h, as it is higher in men (Fig. 3).
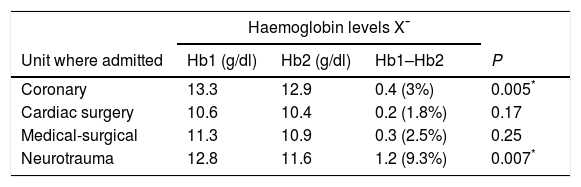
The patients admitted to the coronary and neurotrauma units had a statistically significant greater fall in Hb in comparison with basal values (Table 2).
Average haemoglobin levels according to unit where admitted.
| Haemoglobin levels X¯ | ||||
|---|---|---|---|---|
| Unit where admitted | Hb1 (g/dl) | Hb2 (g/dl) | Hb1–Hb2 | P |
| Coronary | 13.3 | 12.9 | 0.4 (3%) | 0.005* |
| Cardiac surgery | 10.6 | 10.4 | 0.2 (1.8%) | 0.17 |
| Medical-surgical | 11.3 | 10.9 | 0.3 (2.5%) | 0.25 |
| Neurotrauma | 12.8 | 11.6 | 1.2 (9.3%) | 0.007* |
Hb1: haemoglobin at admission; Hb2: haemoglobin after 24h; Hb1–Hb2: difference between haemoglobin levels at admission and after 24h.
The number of analytical determinations and the volume of blood extracted in 24h were not statistically significant respecting the difference between basal Hb and Hb at 24h. The women who underwent more than nine extractions showed a greater fall in Hb than the men (Table 3).
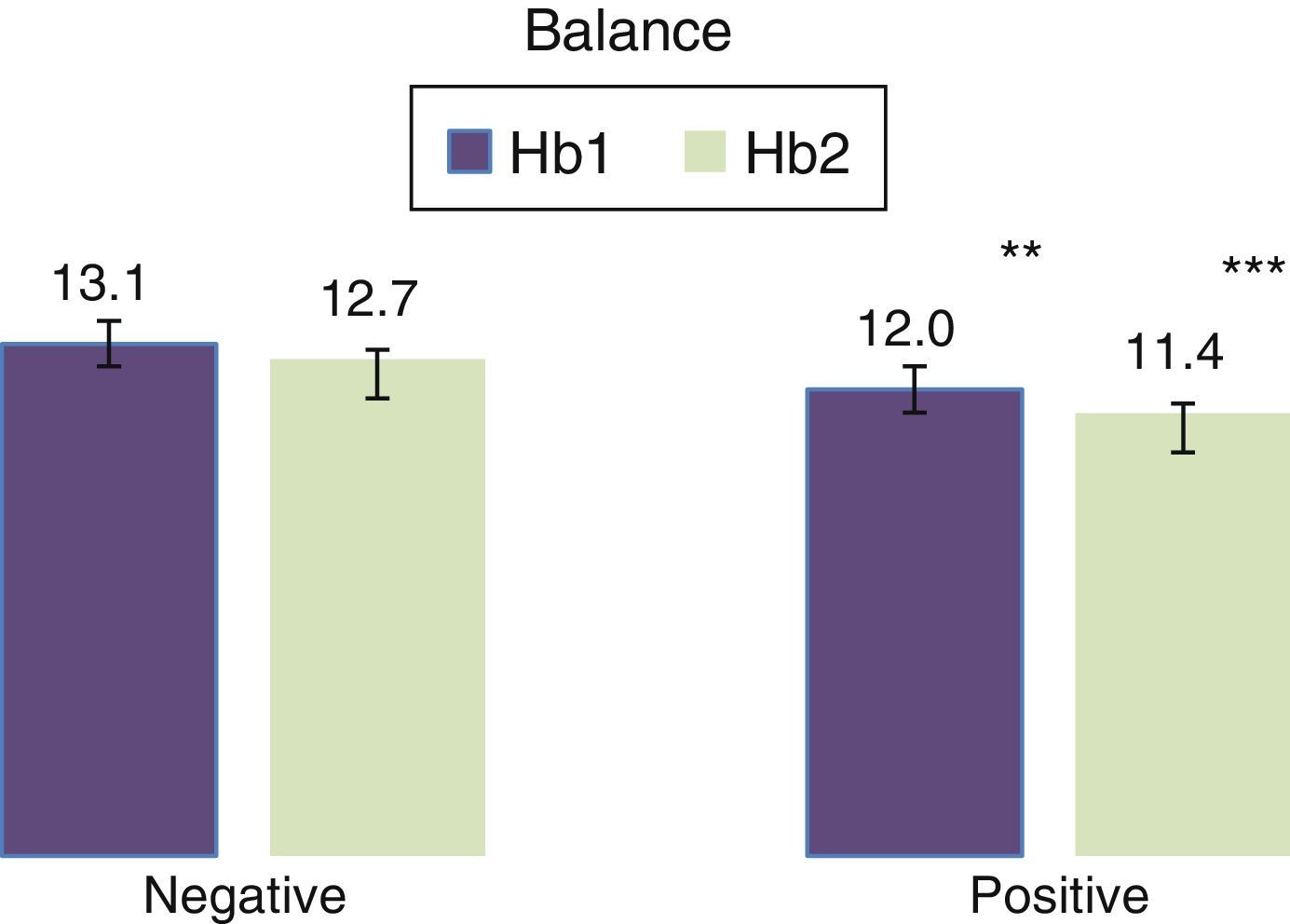
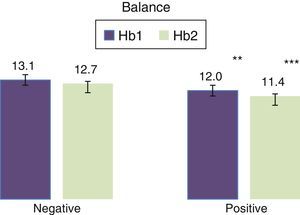
The patients with a positive balance had lower Hb values at 24h than their basal Hb value. This was statistically significant with a weak negative correlation (Fig. 4).
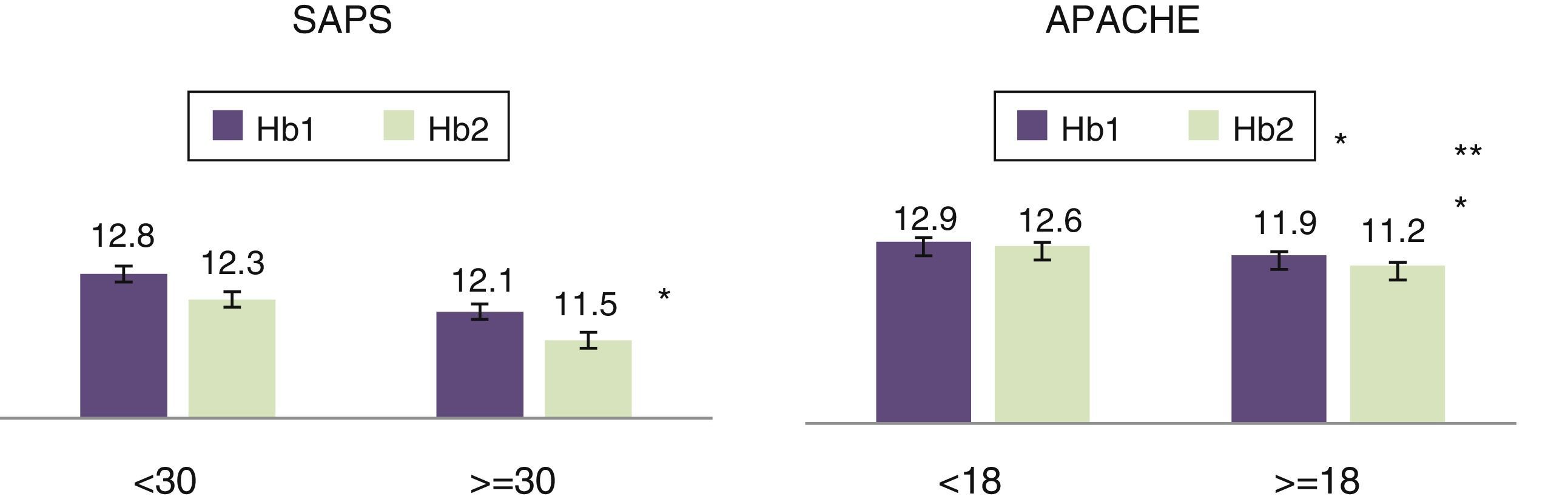
The APACHE and SAPS severity indexes were statistically significant too, with a weak negative correlation; the highest values of Hb corresponded to lower scores on the severity scales or less severe patients (SAPS: rS=–0.210; P=0.036. APACHE: rS=–0.256; P=0.004) (Fig. 5).
DiscussionLoss of blood due to diagnostic and therapeutic tests is associated with a fall in Hb.7–9 In our study the average number of analyses per patient was 7. Vincent et al., with a data gathering period of the same length as ours, state that 46% of patients undergo an average of 4.6 analyses in 24h.12 On the other hand, Mendoza et al.13 conclude that approximately 50% of patients undergo an average of 8±5 extractions per day. According to Carrillo et al.14 the number of extractions varies from 5 to 12 per day.
We observed that the volume of blood extracted varied, depending on patient pathology; the units where the greatest number of extractions took place during the first hours after admission were Cardiac Surgery and the Coronary Unit. These created enzyme curves to monitor patients after cardiac surgery, or to monitor cardiac enzymes in patients with acute cardiovascular pathology. We agree with the bibliography that these patients have greater blood losses.15 Carrillo et al.14 describe blood volumes of from 41.5 to 377ml in cardio-thoracic intensive care units, 240ml/day in medical–surgical units and 41.5ml/day in mixed units. Nevertheless, Wisser et al.16 describe lower losses: 40ml in vascular surgery and 26ml in general surgery.
When the average amount of blood eliminated before the extraction of samples is analysed, the Surgery and Coronary Units were once again the ones that eliminated the largest amounts. The higher the number of extractions, the larger the volume of blood that was extracted. Tineo17 states in his doctoral thesis that the amount eliminated in an ICU varies from 28.5% to 33.1%. These are smaller percentages than the one calculated in our study, which amounted to 40%. The bibliography recommends the use of blood-conserving devices to reduce losses due to phlebotomies.18,19
When we talk about the volume extracted we refer to the amount eliminated plus the useful volume that is necessary for sample analysis. Some studies talk about the daily extraction of blood, although they do not specify whether they have also studied the amount eliminated. The average total volume of blood extracted in 24h from our patients was 80.7ml. If we compare this with similar studies, the results are variable. Vicent et al.12 state that in European ICUs the daily extraction of blood for diagnostic purposes amounts to from 40ml to 70ml, with an average of 41.1ml±39.7ml. Carrillo et al.20 analyse the extraction of blood in different ways, and the average stands at 94.26ml (±21.02ml) in the first 24h. Smoller and Kruskall21 found that more than 40ml/day of blood is extracted for analysis from ICU patients, compared with the 12ml/day that is extracted from hospitalised patients. In the study by Mendoza et al.13 in an ICU, the average total volume extracted is 23ml (±10ml). These results differ widely from those obtained by Henry et al.22 (85.3ml) and Rawal et al.23 (70ml). In this study we find no relationship between the volume of blood extracted and the fall in Hb, as is also the case in the study by Tosiri et al.24
Some studies state that the basal Hb of critical patients is lower than the level recommended by the WHO.12,20 The average values of Hb in our patients at admission were slightly lower: 11.9g/dl in women and 12.8g/dl in men. Although the aetiology of this anaemia was not the objective of this study, Woodman et al. state that in patients older than 64 years old 11% of men and 10.2% of women have anaemia before admission to an ICU; 33% is due to an unknown cause, 33% is due to nutritional deficits and 33% is due to chronic diseases.25
It has been observed that patients with neurotraumatic and cardiovascular pathologies have greater falls in their Hb level. Meroño et al.26 state that anaemia during the hospitalisation of coronary patients may be due to the associated risk of bleeding, invasive procedures, anticoagulation, thrombolysis and antiplatelet treatment. They conclude that nosocomial anaemia without evident bleeding is a long-term morbimortality predictor. Moscote et al.27 state that 50% of patients admitted with craneoencephalic trauma (CET) have anaemia. Haemodilution and the increase in blood losses suffered by patients of this type favour the appearance of anaemia. The difference between the total volume of blood extracted in these two groups of patients and its repercussion on Hb at 24h is striking. According to the European Journal of Anaesthesiology, the most frequent causes of blood loss are procedures carried out on cardiovascular patients, trauma patients and craniofacial ones, among others.28
Another cause of anaemia may be haemodilution or the increase in volemia.29 In this study we observed that patients with a positive balance had lower values of Hb, and this was statistically significant. Our findings disagree with Mendoza et al.,13 as they conclude that there was no statistical significance between the accumulated balance and Hb level.
We agree with some authors that there is a significant correlation between disease severity and the fall in Hb, as this exposes the most severe patients to a higher risk of anaemia and therefore more needs for transfusions.12,16 Other studies conclude that anaemia increases mortality in critically ill patients.30,31
Developing anaemia in critical patients may go unnoticed. Critical patients should be identified as at a high risk of developing anaemia. It is necessary to make the healthcare professionals involved aware of this so that they avoid unnecessary, excessive or arbitrary extractions. One of the strategies which we as nurses can use is to employ conservative extraction techniques, reducing the volume of eliminated blood and minimising iatrogenic blood loss in critical patients.
Limitations. It has not been possible to prove that the extraction of samples for analysis is associated with the reduction in Hb, perhaps because of the short data-gathering period. Future studies should prolong the duration of the research. Nursing professionals took part voluntarily: those in the Coronary unit recorded the most data, so that homogeneity in terms of the unit patients were admitted to was not achieved, and the sample was mainly composed of coronary patients. Postoperative surgical patients were included, and although losses through other drainages were not recorded, their Hb levels remained stable.
ConclusionsThe number of analytical samples extracted during the first 24h of admission in our study amounted to 7, which is similar to other studies.
Of the total volume of blood extracted, 40% was eliminated and 60% was used in analyses.
There is a fall in Hb during the first 24h of admission of critical patients; it has not been possible to prove any statistical relationship between the number of analytical samples extracted and the fall in Hb at 24h.
The patients with neurotraumatic and cardiovascular pathologies are the ones with the greatest fall in Hb levels at 24h after admission.
The patients with the highest severity indexes and positive balance tended to have lower Hb levels than their basal level.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that the procedures followed conform to the ethical norms of the relevant human experimentation committee, the World Medical Association and the Helsinki Declaration.
Data confidentialityThe authors declare that this paper contains no patient data.
Right to privacy and informed consentThe authors declare that this paper contains no patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all of our colleagues in the ICU of Hospital Universitario Son Espases for their help and participation in data gathering, together with Pilar Sanchís and Aina Yañez for their help in the statistical analysis.
Please cite this article as: Maqueda-Palau M, Pérez-Juan E. Volumen de sangre extraído al paciente crítico las primeras 24h de ingreso. Enferm Intensiva. 2018;29:14–20.