There are several retrospective studies that establish a relationship between some risk factors (cardiovascular risks mainly) and the development of COVID-19 and a severe outcome. Thus, our aim with this study is to find out the former relationship among the population within our basic health area
MethodCohort study. The study sample consisted of 372 patients aged 14 or older who had tested positive for COVID-19 in our health centre by consecutive sampling. Data collected from medical records will be analysed using Frequencies, X2 with a Confidence interval of 95% and those carrying out the study will have prior experience/training in research and will be specifically trained for the aim of this research.
ResultsA worse outcome in patients aged 76 years old on average was found versus patients aged 48.7. Regarding high blood pressure patients, X2 was <0.001 and OR between 3.975 and 21.425 with confidence interval of 95%, finding a worse outcome in these patients. With regard to Diabetes Mellitus (DM), X2 was <0.001 and OR rated between 2.766 and 12.690 with a confidence interval of 95%, also resulting in a worse outcome in these patients. No significant differences regarding a worse outcome were found in Body Mass Index, gender, or toxic habits.
ConclusionsOlder patients had a worse outcome from COVID-19, as well as patients with high blood pressure or DM. We found no differences regarding gender and neither could we find any differences regarding BMI.
La bibliografía consultada, en su mayoría estudios descriptivos, establece asociación entre factores de riesgo para la salud, en su mayoría cardiovasculares, y la mala evolución de la COVID-19. Este estudio pretende mostrar dicha asociación entre la población perteneciente al área de salud zona vi de Albacete (España)
MétodoEstudio de cohortes de carácter retrospectivo. Mediante muestreo consecutivo se ha obtenido una muestra de 372 pacientes, mayores de 14 años, con diagnóstico confirmado de COVID-19. Los grupos se han dividido entre buena y mala evolución, entendiendo esta última como ingreso en UCI y/o muerte. Los datos obtenidos mediante la explotación de historias clínicas han sido analizados obteniendo frecuencias, Chi cuadrado con intervalo de confianza al 95% y ajustando por factores de confusión.
ResultadosPor edad los pacientes con mala evolución tenían una media de 76 años, frente a los 48,7 años de los pacientes que evolucionaron favorablemente. Los pacientes con HTA presentaron peor evolución; siendo la Chi cuadrado <0,001 y la OR, para un intervalo de confianza del 95%, estuvo entre 3,97 y 21,42. En los paciente con DM también se relacionó la mala evolución de la enfermedad, siendo la Chi cuadrado <0,001 y la OR, para un intervalo de confianza del 95%, entre 2.766 y 12.690. Los pacientes que presentaban DM + HTA tenían un riesgo 5 veces superior de mala evolución respecto a los que solo presentaban una de las enfermedades. Nuestro estudio no pudo encontrar diferencias estadísticamente significativas entre el IMC, el sexo y los hábitos tóxicos (consumo de alcohol, tabaco y drogas) y la mala evolución de la COVID-19.
ConclusionesLos pacientes de mayor edad tuvieron un peor desenlace de la enfermedad, así como los hipertensos y diabéticos. No se encontró relación entre la evolución y la distribución por sexos. No se pudo establecer relación entre el IMC y hábitos tóxicos y la mala evolución.
The type 2 coronavirus that causes severe acute respiratory syndrome is a new zoonotic pathogen that has caused the largest pandemic since the emergence of the flu. Efforts have been made against the clock to establish a causal relationship in order to identify the main risk factors leading to increased mortality. Several studies consulted following a comprehensive bibliographic review have identified older age, male sex, smoking, hypertension, diabetes mellitus, obesity, and chronic renal insufficiency, among others, as some of the most relevant risk factors.
What it contributes?In Spain, we are currently facing the sixth wave of transmission of this highly infectious, deadly virus. The increase in healthcare activity, as well as the ever-changing information resulting from ongoing research on the subject, is rendering healthcare work more challenging. With this study, we have sought to design a map of contagion and evolution of COVID-19 in an area of Albacete and to determine whether the standard risk factors match our study population. With these findings we hope to be able to predict the course of the disease and ensure greater control over the population exposed to it.
Severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) is a novel zoonotic pathogen. In December 2019, a cluster of cases of pneumonia related to this new virus broke out in Wuhan City, China. The number of cases increased at a dizzying rate given the high transmissibility and infectivity of the virus responsible.
Transmission became difficult to control or prevent since the Chinese health authorities announced the possibility of person-to-person transmission, even among asymptomatic subjects.
The World Health Organisation designated this new pneumonia as coronavirus disease 2019 (COVID-19) and declared it a Public Health Emergency of International Concern (PHEIC). Likewise, on 11 March 2020, the global pandemic was declared and is currently ongoing.
Especially in Spain, the exponential increase in the number of infections and the possibility of SARS CoV-2 leading to severe respiratory syndromes, with case fatality rates of approximately 10.42%, has meant that at the height of the epidemic in our country, health, human, material, and economic resources have been profoundly affected.1,2
Spain is currently engaged in a campaign to vaccinate the population with the four types of vaccines available; nevertheless, the disease continues to spread unchecked, albeit with less saturation of the health system.
Since the onset of the disease, first in China3–9 and subsequently in the rest of the world,10–21 many researchers have sought to develop a tool with which to estimate the risk of a poor course of the disease, with the aim of distributing resources as efficiently as possible.
The aim of this study is to report and compare the demographic, epidemiological, and clinical characteristics, as well as the complications and evolution of the disease in people diagnosed with COVID-19 from the Basic Healthcare Area VI of the city of Albacete. The possible risk factors have been analysed from the currently available literature in order to identify a scientific association that may help to predict severe cases and decrease mortality.
Our search of the literature, based primarily on systematic reviews, yielded differing results, but overall, most of them revealed an association between worse disease outcome due to COVID-19 as a function of co-morbidities. The vast majority of the studies published did find a relationship based primarily on age over 65 years as an independent risk factor,19 the presence of arterial hypertension,4,14,16 an association between arterial hypertension, active smoking, and type II DM,3,4,6,7,10–12,15,17,22,23 obesity as an independent risk factor,9,20,21,24 or male sex as a predictor of unfavourable outcomes.8,25–28 Others, however, fail to detect an association between hypertension or obesity and admission to the ICU or death.4,6,13–19,24,29
ObjectivesGeneral: To find an association between certain risk factors or comorbidities (hypertension and metabolic syndrome) and the evolution of the individual diagnosed with COVID-19.
MethodDesignThis is a retrospective cohort study.
Study population and sizeWomen and men aged 14 years and older from the Area VI Healthcare Centre of Albacete with a confirmed diagnosis of COVID-19 were identified. The variables of age, sex, diabetes mellitus (DM), obesity, arterial hypertension (AHT), and type of antihypertensive treatment were analysed, and attempts were made to predict the poor evolution of the disease (regarded as admission to the ICU or death) based on the number and/or type of risk factors associated with the patient by means of relative risk (RR).
The sample was derived from the population of the Area VI Basic Healthcare Centre of Albacete (Spain). Sample size was calculated using the EPIINFO computer application, taking into account the following considerations obtained from the bibliographic review:1,28
- -
Population size BHA VI: 25,000.
- -
Risk among the population exposed = 60% (using as a mean the percentage of those exposed to the risk factors under study in the literature review).
- -
Risk among the unexposed population = 22% (using as a mean the percentage of those exposed to the risk factors under study in the literature review).
- -
Ratio of unexposed/exposed = 1.
- -
Confidence level = 0.95.
- -
Statistical power (1-β) = 0.90.
- -
Cluster: 2.
- -
Sample size: 372.
The inclusion and exclusion criteria for participation in the study were as follows:
- -
Inclusion criteria: male or female, aged 14 years or older, with a confirmed diagnosis of COVID-19 between 1 January 2020 and 30 November 2020, and belonging to Area VI Basic Healthcare Centre of Albacete.
- -
Exclusion criteria: paediatric subject under 14 years of age, patient classified as contact/exposure to coronavirus with negative molecular biological test results and without compatible clinical findings.
Cases were obtained through the Turriano software programme of the GAI of Albacete, resulting in a list of anonymised cases ordered on the basis of the date of diagnosis since January 2020 of patients diagnosed with COVID-19 in Area VI BHA of Albacete.
Study variables- -
Independent variables: age, sex, toxic habits (alcohol, tobacco or drugs), body mass index (BMI, stratified into underweight, normal weight, overweight, or obese), hypertensive patient (classified as such in their clinical history), good HTN control (good control being defined as less than 140 systolic blood pressure and/or 90 mm Hg diastolic blood pressure and poor control as equal to or greater than 140/90 mm Hg), type of antihypertensive treatment, and subjects with DM.
- -
Dependent variable: nature of the course of COVID-19 (good course was defined as a person who did not require hospitalisation or who had to be admitted to a regular hospital ward, and poor course as an individual who had to be admitted to the ICU or who was discharged).
The statistical software Statistical Package for the Social Sciences version 26.0 (SPSS 26.0 hereinafter) was used for data entry and analysis. First, the data were coded and a descriptive study of the variables was undertaken. For quantitative variables, the mean and standard deviation were calculated, whereas, in the case of categorical variables, frequencies were determined by means of cross-tabulations, odds ratios, Pearson’s Chi-square, parametric and non-parametric tests, and frequency distributions were evaluated.
Ethical considerationsAuthorisation was obtained from the Ethics Committee of the Albacete University Hospital. The ethical principles of beneficence were complied with, preserving confidentiality by means of the database, which assigned an identifier to each participant that was meaningless except for the study database. The study was carried out in accordance with the principles of the Declaration of Helsinki. There are no data that could be used to identify any of the participants; in any case, this research project adheres to the regulations set out in the Organic Law on Data Protection, which came into force on 25 May 2018, approved by the Council of Ministers on 10 November 2017, as well as its implementing regulations; also Regulation (EU) 2016/679 of the European Parliament and of the Council dated 27 April 2016 concerning the protection of individuals with regard to personal data processing as well as the European Commission and the FMT Council: BoaldMayor Commission guidance on the direct application of the General Data Protection Regulation dated 25 May 2018/FMT.
ResultsThe data base from the Castilla La Mancha Healthcare Service was reviewed; after applying the programme’s filters, 600 clinical histories were selected for study, of which only 372 met the inclusion criteria set.
Table 1 displays the frequencies per variable.
Distribution of frequencies by exposure variables.
| Cases | ||||||
|---|---|---|---|---|---|---|
| Valid | Lost | Total | ||||
| N | % | N | % | N | % | |
| Exposure to toxic habits * evolution code change | 372 | 100.0 | 0 | 0.0 | 372 | 100.0 |
| Blood pressure in mm Hg * evolution code change | 372 | 100.0 | 0 | 0.0 | 372 | 100.0 |
| Type of treatment to control HTN * change of code evolution | 372 | 100.0 | 0 | 0.0 | 372 | 100.0 |
| Metabolic syndrome * code change evolution code change | 372 | 100.0 | 0 | 0.0 | 372 | 100.0 |
| Sex: male or female * change of evolution code | 372 | 100.0 | 0 | 0.0 | 372 | 100.0 |
| BMI categorised * change of code evolution | 119 | 32.0 | 253 | 68.0 | 372 | 100.0 |
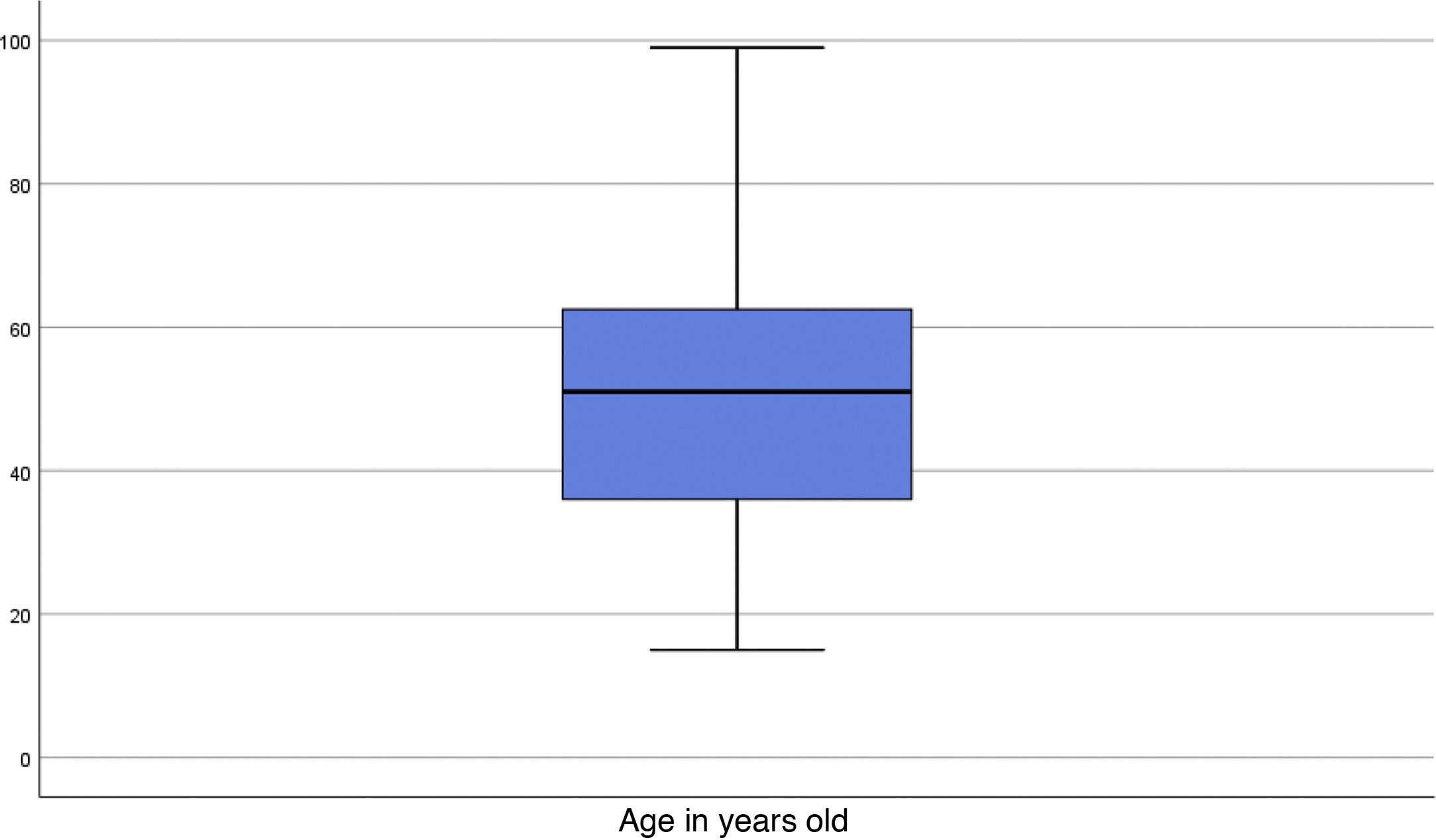
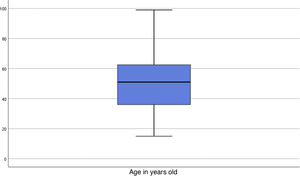
Participants’ ages ranged from 15 to 99 years, with a deviation of 18.83 (Fig. 1). Given the size of the sample, the Kolmogorov-Smirov was applied to the age variable to test for normality, revealing that it did not conform to normal distribution. In order to come to a clinical interpretation of the difference of means, the Mann-Whitney U test and the “t” test were used, by means of which two independent groups were established (poor and good course of COVID-19). The results evidenced that patients with a mean age of 76 years had a worse outcome compared to those with a good outcome, whose mean age was 48.7 years. In order to perform the suitable comparison of means, given that the variance of both age groups according to Levene’s test was F = 1.745 (there is homogeneity of variances between the samples); similarly, Student’s t-test was performed, yielding a t-test result of <0.001, and the 95% CI with respect to the difference between the means was in the range of 20.928 and 33.671.
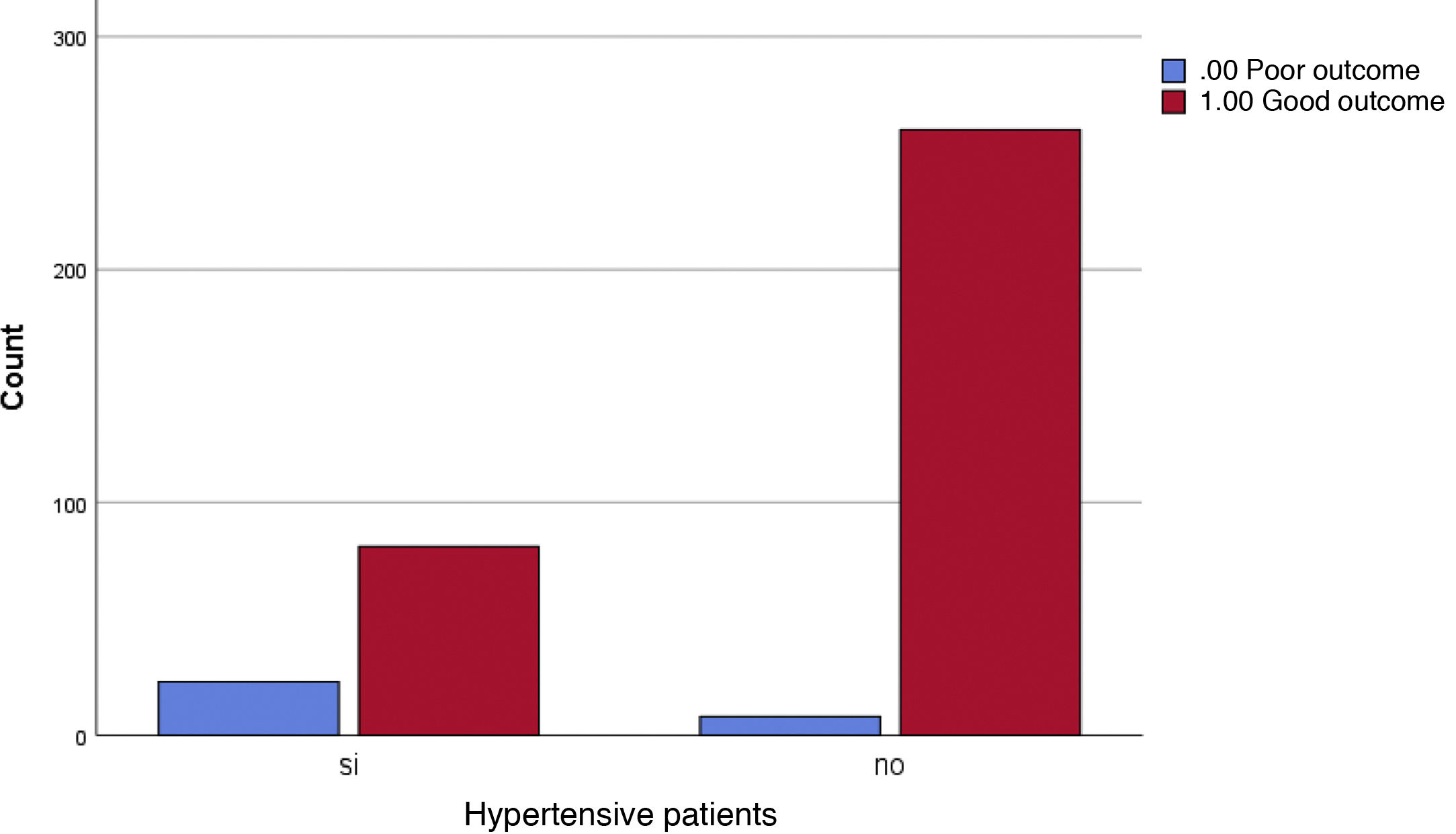
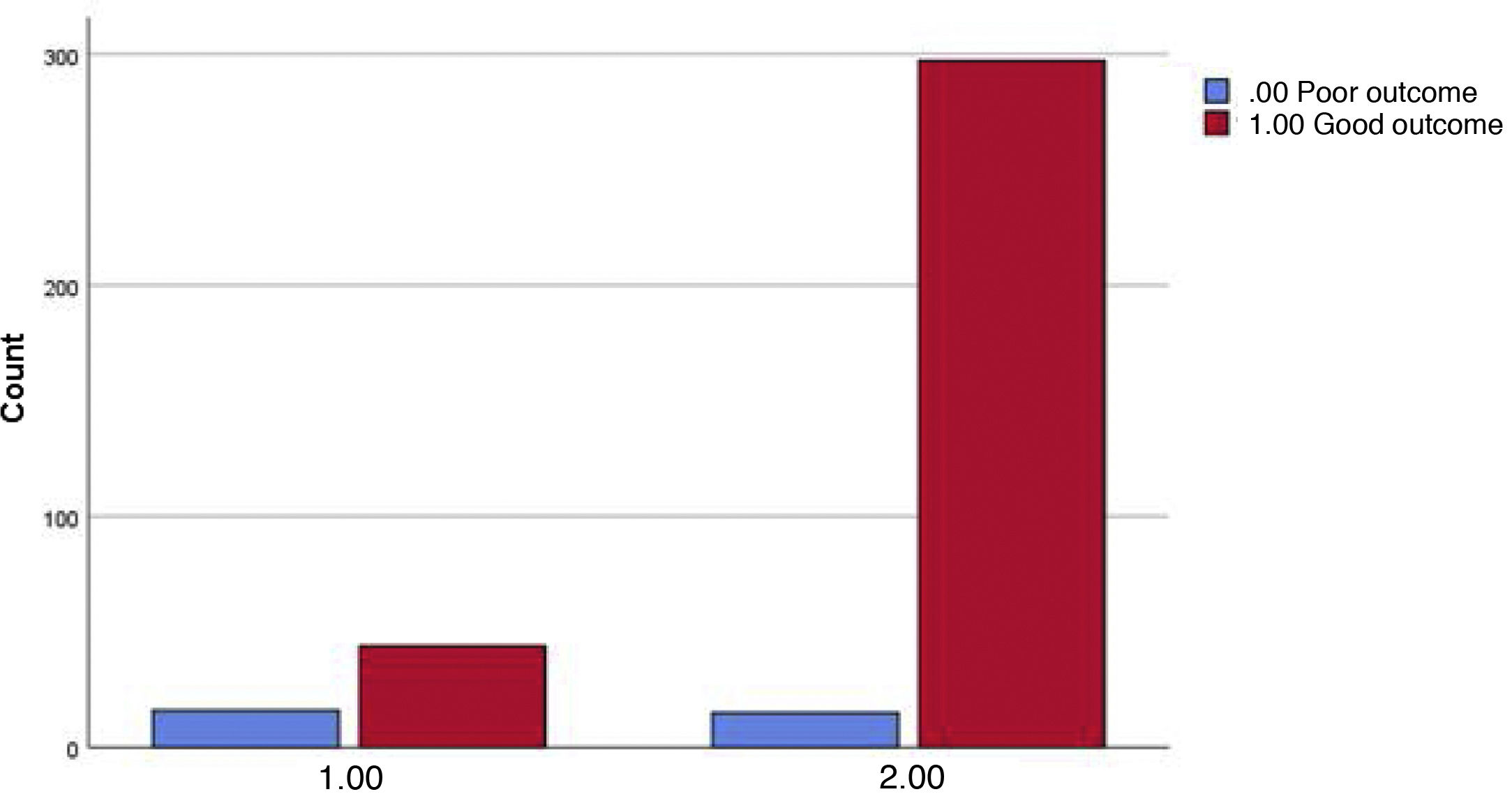
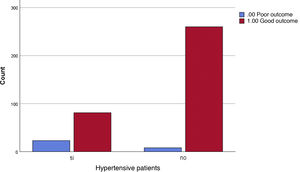
The percentage of hypertensive individuals presenting a poor COVID-19 outcome was 22.1% in comparison to 3% with the same outcome in non-hypertensive patients. Chi-square was <0.001 and OR for 95% confidence interval was between 3.975 and 21.425 (Fig. 2).
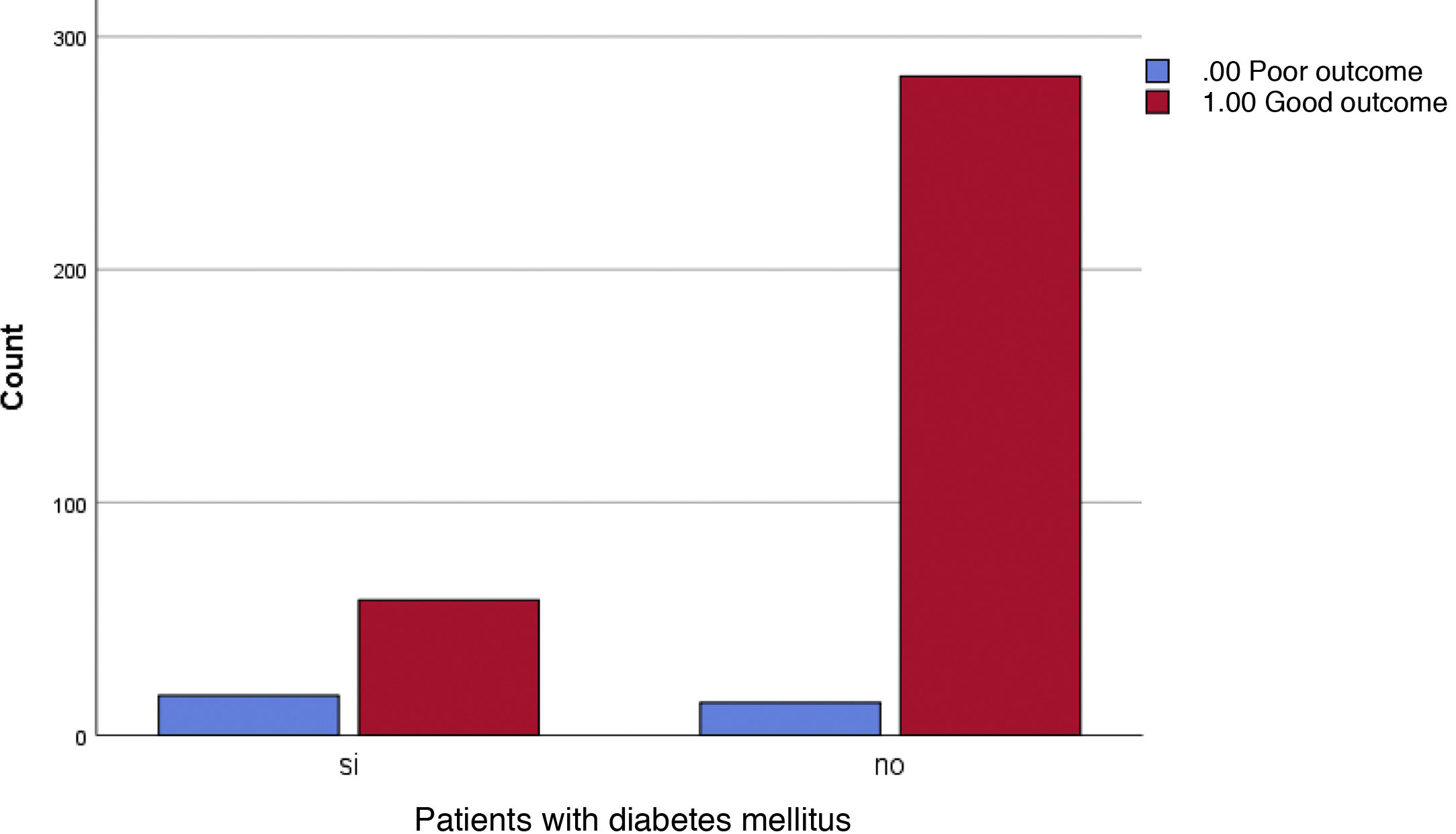
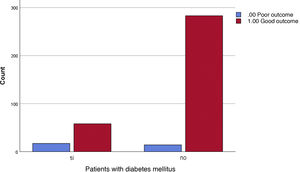
The percentage of subjects diagnosed with DM who had a poor course of COVID-19 was 22.7% versus 4.7% among non-diabetic participants who had the same course. The Chi-square was <0.001 and the OR for a 95% confidence interval was between 2.766 and 12.690 (Fig. 3).
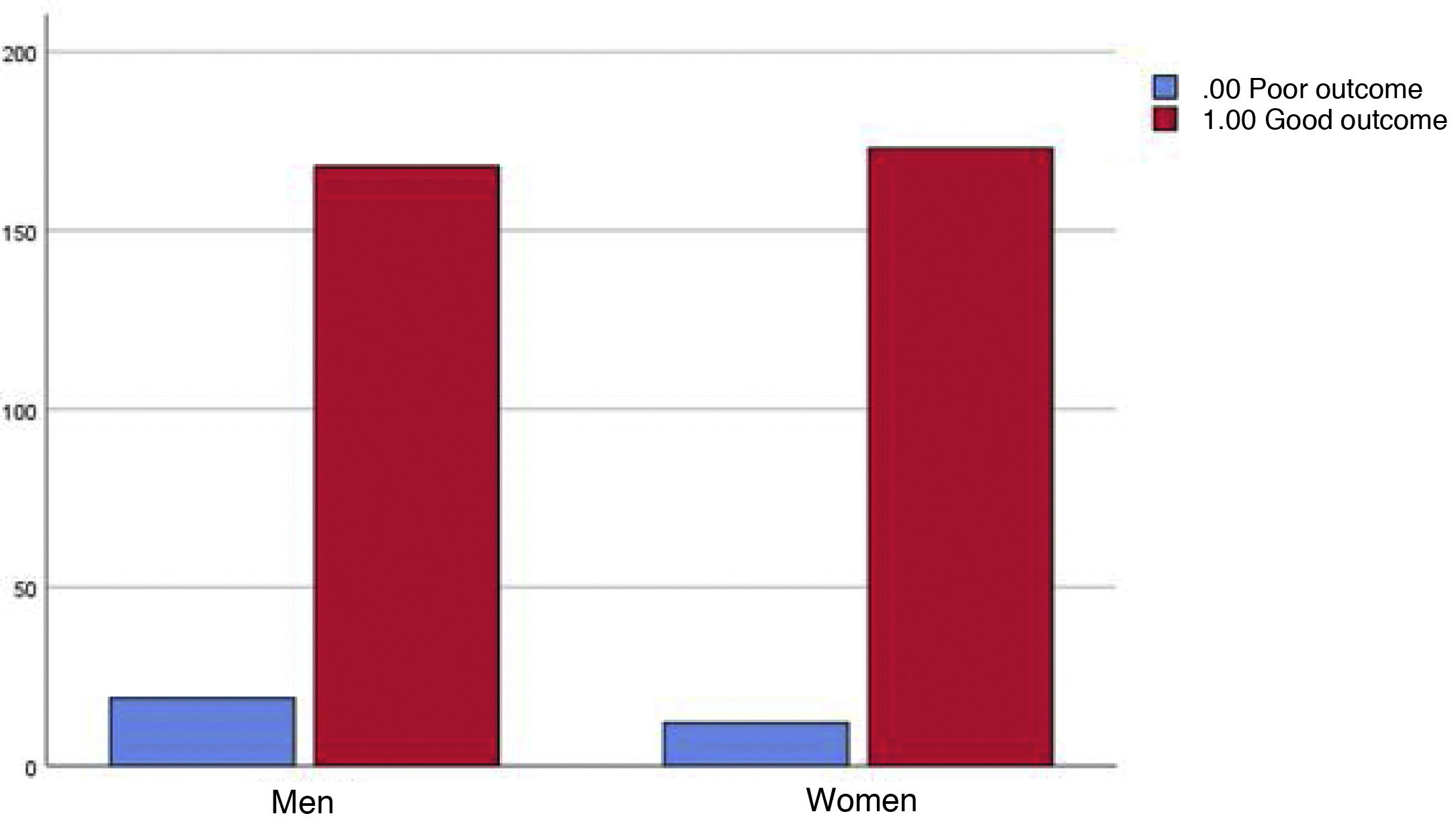
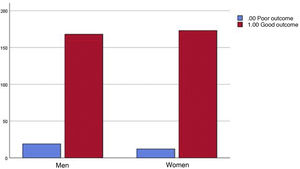
No statistically significant differences were detected between BMI and poor outcome, sex and poor outcome, or toxic habits and adverse COVID-19 outcome (Fig. 4).
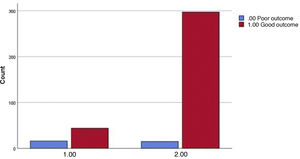
Finally, the sum of patients with DM + HTA diagnoses was analysed with respect to the evolution of COVID-19, revealing a 26.7% rate of poor evolution among patients with both diagnostic entities compared with a 4.8% poor evolution in individuals who did not have these two diagnoses; the Chi-square <0.001 and the OR for a 95% CI was between 3.326 and 15.586 (Fig. 5).
In the first columns, patients with AHT + DM and poor outcome are shown in blue and patients with the same conditions and good outcome are shown in red. The second columns display subjects without HTA + DM and poor evolution and those in the same conditions with good outcome are shown in red.
The analysis of the results evinces a significant association between patients with HTN and poor outcome. Several studies among those consulted also detected such an association.4,6,11,12,14,16,17
The relationship between diabetes and ICU admission and/or death was statistically significant. This is in line with earlier studies,3,4,6,7,11,12,17 which established that the strength of the association had varying degrees.
Longevity has been identified as a prognostic factor for worse course of disease. Some authors have demonstrated this relationship above the age of 50 or 65 years.11,14,19,28 However, in our study, the mean age of subjects exhibiting an adverse outcome was 76 years.
With our data, we were unable to establish any difference in mortality as a function of sex. Nevertheless, some authors did find one,8,25–28 making further research necessary to ascertain whether or not there is excess mortality depending on gender.
As regards BMI, several studies have found a relationship between higher weight and worse outcome.3,9,9,11,12,17,20,21,24 In our study, weight and height parameters were not recorded in many of the clinical histories and could not be calculated. The recorded data appeared to suggest such a correlation, albeit there were no records to prove that the relationship was statistically significant. The same was true for the toxic habits variable (alcohol, tobacco, and drugs). This enables us see how important it is to record events related to health and illness properly, so that health behaviours can be analysed. Thus, we can ascertain the risk factors on which we can exert the greatest impact for prevention and control.
As a final conclusion, the epidemiological characteristics of the population of the Zone VI Health Centre in Albacete (Spain) were as follows:
- -
Mortality was approximately 9%, with no differences by sex. Older patients had a worse outcome, as did hypertensive and diabetic individuals, with a substantial increase in risk among subjects presenting both conditions.
- -
It was not possible to establish a relationship between BMI and the toxic habits because the records lacked the necessary information.
- -
It would be interesting to repeat this same study in the future, in the same BHA, to assess how vaccination impacts the analysis of the same variables.
Our study presents a number of limitations:
Limitations due to its being a cohort study. Its most notable limitation is that systematic errors are easily introduced, both with respect to group selection and data collection, and that it examines the relationship between study event and exposure to only a relatively small number of factors measured at the start of the study.
Specific limitations of this study. First, its sample size is ideal for making inferences about the geographical area in which the health centre is located, but it involved only a single healthcare centre in a city of 160,000 inhabitants and might not be susceptible to inference to a universal population. Second, the retrospective design led to a considerable amount of missing data, due to lack of computerised records, in particular as regards the BMI variable, which should be taken into account as a constructive criticism to all health professionals, since a complete record of our health care work is essential. Finally, the data collected for the most part concern a period during which the disease evolved very poorly in general. In Spain at present, a high percentage of cases are asymptomatic or have milder symptoms, despite having the same risk factors; therefore, one might deduce that there are more specific factors that may not have been contemplated.
It is difficult to control for such biases, and the only way to minimise these limitations is to take them into account when interpreting the results.
Conflict of interestThe authors have no conflict of interests to declare with respect to the present project.
Manuel Gutiérrez Pérez, Pilar Córcoles Jiménez, Antonio Cifuentes Verdú, Juan Ríos Laorden, Marcelino Requena Gallego, Sebastía Sabater Martí, Milagros Alfaro Moya, and Otilia Gómez López.
Please cite this article as: Cantero-Quintero S, Sáez-Martínez M, Castellanos-Garrido AB. Evolución del paciente diagnosticado de sindrome respiratorio agudo severo por coronavirus tipo 2 en función de la comorbilidad de la población adscrita al Centro de Salud Zona VI de Albacete. Enferm Clin. 2022;32:217–224.