Care of chronicity is a pressing issue for health systems because of its high prevalence and the organisational challenges that it generates. Different countries solve the complexity of the care of chronicity through case management by the nursing profession, obtaining good results.
This paper analyses the status of institutionalisation of the case management nurse in Spain through the design of a reference standard to compare between the autonomous communities in their approach to chronicity. Thus, we sought to monitor the degree of progress of the institutional structure of the policies for the care of chronicity in our country through this healthcare professional. Our results showed that no autonomous community has reached the maximum standard of implementation and that the situation is very heterogeneous, confirming a weak and erratic degree of institutionalisation of the case management nurse in Spain despite the formal recognition of their role in patient care.
La atención a la cronicidad es una necesidad acuciante para los sistemas de salud por su elevada prevalencia y los retos organizativos que su atención genera. Diferentes países resuelven la complejidad de la atención a la cronicidad mediante la gestión de casos a través de la profesión enfermera, con buenos resultados.
En este trabajo se analiza el estado de institucionalización de la figura profesional de la enfermera gestora de casos en España mediante el diseño de un estándar de referencia para la comparación entre comunidades autónomas del abordaje de la cronicidad. Se pretende de esta manera monitorear el grado de avance de la estructura institucional de las políticas de atención a la cronicidad en nuestro país mediante esta figura asistencial.
Entre los resultados encontramos que ninguna comunidad autónoma ha alcanzado el estándar máximo de implantación y que la situación es muy heterogénea, en la que se constata un débil y errático grado de institucionalización de la enfermera gestora de casos en España a pesar del reconocimiento formal a su papel en la atención al paciente crónico.
“Institutions have been devised by human beings to create order and reduce uncertainty”
The main objectives of every country's health system are to maintain and improve the health of their citizens. Healthcare policies are developed to that end, which involve various strategies, lines and interventions. For policies to be developed that meet the population's health needs, first and foremost requires knowledge of all the population's demographic characteristics and health situation.
At present, the epidemiological pattern in Spain is dominated by chronic disease. According to the European Health Survey 2009, 45.6% of the population over the age of 16 have a chronic disease, and 22% of the population have 2 or more. According to the National Health Survey of 2006, people aged between 65 and 74 have an average 2.8 chronic diseases and this increases to 3.23 in those aged over 75. These diseases already comprise 80% of primary care consultations. Added to this is the marked trend for these diseases to increase in the years to come.1
Spain has one of the longest-living populations in the world, with a life expectancy of 82.3 years. And, although the mean age of the population is 42.4 years, our country's population is ageing, 18.38% are aged over 65, which is accompanied by a growing percentage of chronic health conditions. Given this situation, in 2012 the National Health System developed their Strategy for Approaching Chronic Disease, which highlighted the need to remodel the health system to tackle the issue of chronicity.1
However, the experts conclude that the current health systems are not providing an adequate response to these chronic disorders and stress the need for a turnabout in the current health policies.
This was highlighted by the WHO more than a decade ago. They presented the document “Innovative care for chronic conditions: building blocks for action” in 2002, and “Preventing chronic diseases, a vital investment” in 2005. Both documents expose the urgent need to tackle the number of chronic diseases and the obligation of all countries to ensure their health systems are targeting these diseases.2,3
The European Union, following these directives, with the same objective as the WHO, drew up their “Action plan for implementation of the European strategy for the prevention and control of non-communicable diseases 2012–2016”, which has been implemented since 2011. Likewise, the project on the Joint Action on Chronic Diseases and Promoting Healthy Ageing across the Life Cycle (JA-CHRODIS) in its section “Time to face the challenge of multimorbidity” exposes the need for the comprehensive care of the chronic patient, not merely focussing on their disease.4,5
In Spain, in 2011 the Spanish Society of Family and Community Medicine (SEMYC) together with the Spanish Society of Internal Medicine (SEMI) drew up the consensus document “Care of the patient with chronic diseases” almost at the same time that their National Health Service drafted their strategy for approaching chronic disease in 2012. Both documents highlighted the need to remodel the health system to tackle the problem of chronicity.1,6
The chronic patient who enters these documents’ area of interest requires complex care due to the confluence of high comorbidity associated with advanced age. The care response cannot be simple and focus on one health problem alone, as has been the case to date. The response, more than ever, requires a specific personalised care plan, and treatment in a social and family context which is also specific.
“Case management” is the care strategy covered within this new paradigm. This care tool was born in the U.S.A. in the 1950s due to the need for individual follow-up of people with mental health problems after the deep reform in the country that resulted in people who had been detained in psychiatric centres being returned to their homes. The care model was exported to various European countries with different situations and they adapted it to their health systems. Countries like Canada, the USA and the UK decided from the outset that nurses should manage cases with chronic disorders, since they combined the requirements to integrate all the necessary functions most efficiently.7
Our country also decided that nurse case management should provide the framework for care of the complex, chronic patient. The abovementioned “Strategy for approaching chronic disease in the National Health System” recommends enhancing the work of nurses in the care of chronic disease, targeting their responsibilities, particularly in their role as educators/trainers in self-care, in their role as case managers for patients of particular complexity and in their role of liaison nurses,1to improve the transition between care areas and units.
This recommendation, among others, was agreed in the National Health System's Inter-territorial Council of 27 June 2012 by all the health advisors of the autonomous regions. The Inter-territorial Council is the main instrument for shaping the National Health System and its functions are to establish, discuss and, where appropriate, issue, recommendations for comprehensive health plans, among others.
This recommendation to promote nurses as case managers (CMN) was adopted in 2012. Many autonomous regions have spent time designing and awarding this professional role to nurses, although others had not even considered doing so until then. A result of the aforementioned meeting was that the autonomous regions that had still not yet systematically tackled chronic disease designed their own plans including, to a greater or lesser extent, recommendations such as the one we examine in this paper.
Now is the time to start an evaluation of how these recommendations have been implemented in our autonomic health system. To that end, we made it our objective to assess the development of the CMN in Spain through an analysis of the autonomic policies on the care of chronicity. Designing an analysis tool to measure the current situation of this professional figure in our decentralised system of healthcare planning could also serve to assess and enhance their implementation.
Measuring the case management nurse model as a public policyAn institutionalisation process is, on balance, a continuous crystallisation process of various types of norms, organisations and regulatory schemes of procedures.8 But put in such a general way this generates doubt as to how to approach a detailed analysis of an aspect that to us is as crucial—although integrated within a very broad and complex social policy—as the care of chronicity. If, as we suggest in this paper, we are looking at a policy that seeks institutionalisation, in other words, maintenance through time with a defined structure, we need to resort to a more marked framework of analysis.
The answer to these questions will help us gain a general understanding of the limitations that already exist. However we need to focus the analysis framework even better, we must be rigorous and apply a precise methodology to the specific case of the CMN. And this framework exists within the evaluatory praxis in public health. Therefore, this study seeks to be placed within the field of public health policy assessment through an “analysis of the components of policies and plans”.9 The component in this study is the CMN positioned as a tool within the autonomous communities health systems’ plan to deal with chronicity, and therefore the aim is “an evaluation of the institutional structure” designed by them to approach chronicity through this professional figure.10
In order to achieve this, we focussed on the organisational institutionalisation of the Spanish autonomous communities expressed through their official publications, because this is where they set out their health policies. We reviewed the official publications of the 17 autonomous regions and the 2 autonomous cities. We revised the existing general health plans and strategies; the plans and strategies for the care of the chronic patient; the plans and strategies of social-health care and the official documents that describe or protocolise the functions, competencies and activities of the CMN in the context of the public care of the chronic patient. The entire compilation was completed between January and May 2016.
The information obtained was organised based on a gold standard11 following the items that the autonomous communities themselves had been establishing as they implemented this tool to tackle chronicity. In other words, as we analysed the texts and checked whether or not they came close to the recommendation of the national strategy that nurses should lead chronic case management, we were able to establish response patterns that could be classified, grouped and standardised. This standard enabled us to design a standard framework11 between the communities.
To approach item 7 of the standard framework “there is scientific evidence of its functionality” a complementary revision was necessary of the literature for scientific evidence of the work of the CMN in the autonomous health systems that had not undertaken pilot studies to measure their own performance. The databases used were: PubMed, Cuiden, Dialnet, Scopus, Cochrane Library, Scielo, IBECS and Google Academics. Those that, although they referred to the work of the CMN in a particular autonomous health system, did not present measurable data on the effectiveness of their interventions and did not compare these interventions with those undertaken without the participation of the CMN, were discounted.
Beyond this standard, and following its description and analysis, we will make a first attempt to answer the questions that other authors use as a script when they evaluate social policies.12 We first have to ask ourselves whether the strategy of using the CMN as a policy for approaching chronicity comes from a social and political agreement to deal with a specific problem, and then whether there is the will to establish clear objectives and goals and find the instruments to evaluate how they are achieved. The next question is whether specific obligations and rights for each of the relevant actors are being established in the process. And the final question is whether the definition of behavioural norms and rules to consolidate the model has been anticipated.
The answer to these questions is the most limited part of this paper, because it will only be possible to provide this answer when it comes through the development of the standard we designed. To reach more substantiated conclusions we would need a more complex study that covers all the interventions for chronicity and all the actors involved, both institutional and informal. But this will not prevent us from taking everything we can from a careful reading of the wishes of the administrations reflected in official documents.
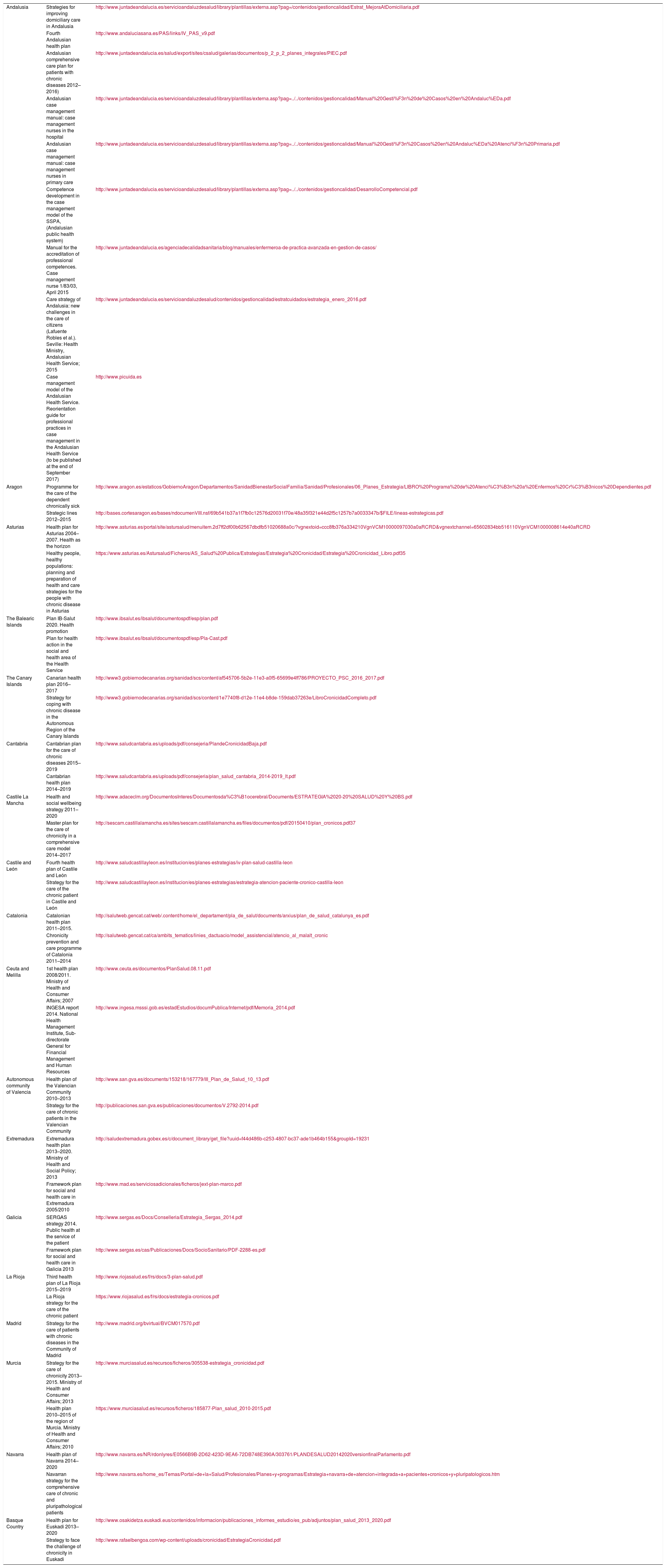
Levels of institutionalisationOur search of the official documents of the policies implemented by each autonomous region and the autonomous cities resulted in 27 official documents that encompass health plans and strategies as well as strategies for the care of the chronic patient (Table 1).
Documents analysed per autonomous region and the electronic resource used.
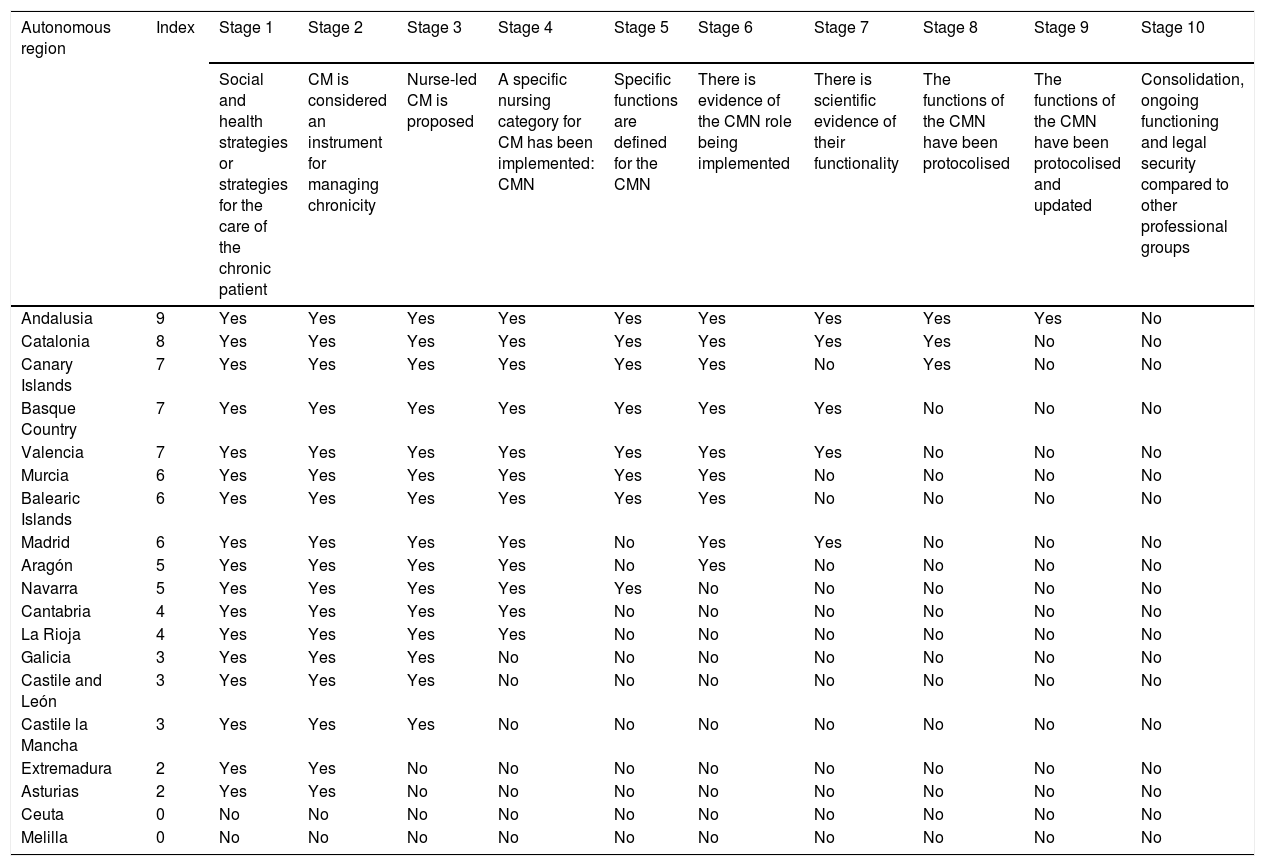
All the information was entered into standard framework (Table 2) following the aforementioned directives, which resulted in an institutionalisation gradient that enabled each autonomous health system to be placed relatively and to be compared with one another. We explain the different levels reached by the autonomous communities in the institutionalisation of the CMN below.
Case management nurse reference standard and institutionalisation index per autonomous region.
| Autonomous region | Index | Stage 1 | Stage 2 | Stage 3 | Stage 4 | Stage 5 | Stage 6 | Stage 7 | Stage 8 | Stage 9 | Stage 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Social and health strategies or strategies for the care of the chronic patient | CM is considered an instrument for managing chronicity | Nurse-led CM is proposed | A specific nursing category for CM has been implemented: CMN | Specific functions are defined for the CMN | There is evidence of the CMN role being implemented | There is scientific evidence of their functionality | The functions of the CMN have been protocolised | The functions of the CMN have been protocolised and updated | Consolidation, ongoing functioning and legal security compared to other professional groups | ||
| Andalusia | 9 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Catalonia | 8 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Canary Islands | 7 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | No |
| Basque Country | 7 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Valencia | 7 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Murcia | 6 | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No |
| Balearic Islands | 6 | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No |
| Madrid | 6 | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | No |
| Aragón | 5 | Yes | Yes | Yes | Yes | No | Yes | No | No | No | No |
| Navarra | 5 | Yes | Yes | Yes | Yes | Yes | No | No | No | No | No |
| Cantabria | 4 | Yes | Yes | Yes | Yes | No | No | No | No | No | No |
| La Rioja | 4 | Yes | Yes | Yes | Yes | No | No | No | No | No | No |
| Galicia | 3 | Yes | Yes | Yes | No | No | No | No | No | No | No |
| Castile and León | 3 | Yes | Yes | Yes | No | No | No | No | No | No | No |
| Castile la Mancha | 3 | Yes | Yes | Yes | No | No | No | No | No | No | No |
| Extremadura | 2 | Yes | Yes | No | No | No | No | No | No | No | No |
| Asturias | 2 | Yes | Yes | No | No | No | No | No | No | No | No |
| Ceuta | 0 | No | No | No | No | No | No | No | No | No | No |
| Melilla | 0 | No | No | No | No | No | No | No | No | No | No |
HC: health centre; CMN: case management nurse; CM: case management.
The standard framework (Table 2) enables the great heterogeneity of the health systems of the different autonomous regions regarding this professional role being undertaken by nurses to be graded and compared. We observe that the degree of implementation of the CMN varies substantially from one autonomous region to another.
Different cut-off points can be established on the index to establish 3 levels of institutionalisation of the CMN. Thus, stages 1 and 2 would be an incipient level of development because they suggest case management is taking place, but not via the nurse; stages 3 and 5 involve a medium level of development because case management via the nurse is referred to but has not been implemented, and stages 6 onwards are advanced development levels because there is a basic level of institutionalisation that can be analysed with evidence of nurse intervention.
Low level of institutional developmentThe existence of social and health strategies or strategies for the care of the chronic patientBecause the CMN is very involved in the care of chronic patients, it is essential first to establish that there is a care strategy in place for these patients.
This parameter is being met by all the autonomous regions except Ceuta and Melilla. These 2 autonomous cities are managed by the Public Health Service (Instituto Nacional de Gestión Sanitaria—INGESA), which is under the jurisdiction of the Ministry of Health and Social Affairs, which might be the reason for their limited planning capacity. The cities each lack the staff for these tasks and do not have political autonomy in social and health matters. It is difficult for them to start planning or even to suggest management through a CMN.
Case management is taken into account in the plans and strategies analysedCase management as a care model does not necessarily mean that it must be undertaken by nurses. In fact, case management as a strategy to cope with chronic illness is claimed by diverse professionals, as we shall see later, including social workers, who consider the function vital.
We can state, however, that all the communities that have a health plan, social health strategy or strategy for the care of chronic patients (i.e., who exceed stage 1) propose case management as the model to improve the care of pluripathological, chronic patients.
Medium level of institutional developmentCase management by nurses is proposedExcept Asturias, Extremadura and the autonomous cities, the remaining autonomous regions consider that nurses should lead case management.
Although Asturias debated the possibility of including nurses, they eventually ruled it out. It is very interesting to follow the debate during the design phase of the strategy for chronicity. The debate is covered in annex IV to the “Strategies for health and the care of people with chronic disease 2014”. During the process, the participants recognised the strategic role of the liaison nurse in the care and follow-up of heart disease patients, a role it was suggested would be interesting to replicate in other areas, such as neurological disease, since ongoing contact and telephone follow-up by the liaison nurse is crucial for quality of care. But when the suggestion was transferred to the care of chronic patients, consensus fell to pieces and there was no possibility of reaching an agreement. The discussion centred on the inconsistency of generating a role for the nurse other than their existing care role. There was no agreement on where management should be based either, whether it should be in primary or hospital care. Serious doubts were raised as to whether the role should be given to family health and community nurses or whether unspecialised care nurses should be used to the full, since they do not have the opportunity to fully use their skills. Finally, this community suggested case management through social and health teams without defining who should comprise these teams, who should lead them or how they should function.
Extremadura, in their “Framework plan for social and health care 2005–2010” wanted to implement social and health commissions to manage cases formed by a professional from the social field and another from the health system. However they did not specify the professionals who should make up this team either.
Implementation of a new nursing category for case management or the development of new skills by existing care nursesThis level is different from the previous level because in these cases not only was case management by nurses considered but it was suggested that a new nursing figure should be implemented within the health framework to use her skills in case management specifically, and in a different way from other nurses. Therefore, in this section we differentiate between the communities that proposed the implementation of this new figure from those who suggested that nurses already working within the healthcare system (primary care and hospital nurses) should use their case management skills with their patients.
Castile La Mancha, Castile and Leon and Galicia did not contemplate including the CMN as a new category within the health system. The former 2 communities suggested that the primary care nurse should take on the skills and functions of case management. Galicia proposed that case management should be nurse lead, but did not elaborate further.
On the other hand, the communities that did suggest there should be a new figure for case management did so in different ways. The Canary Islands, Catalonia and Murcia incorporate the CMN from primary care and she coordinates all the resources and all the professionals involved.
The Balearic Islands incorporate the CMN, but she is included in acute as well as primary care hospitals.
Andalusia, Cantabria, La Rioja, Navarra and Valencia include 2 new CMN figures, one in hospital and the other in primary care. When the patients are admitted to hospital, the hospital CMN is in charge of case management and she coordinates with the community CMN (primary care) for continuity of care.
The Basque Country suggested including 3 figures, 2 in primary care (one for chronic patients and another for complex chronic patients) and the third in hospital care. They were to change their strategy later, as we mention below.
Aragon and Madrid stated that primary care nurses should acquire case management skills. However, Aragon added a new figure: a nurse in charge of the programme in each health sector as a coordinator. Madrid added the hospital liaison nurse in hospitals.
Defining specific functions for the case management nurseIt is not sufficient to state that the CMN is in charge of coordinating system resources; she must be given specific and clear functions that define her professional activity.
In this second step we found that Andalusia, Balearic Islands, Canary Islands, Catalonia, Murcia, Navarra, Basque Country and Valencia describe specific functions for the CMN that are included in official protocols.
Aragon is unique in this aspect since, despite having implemented 8 nurses in charge of the programme since 2006, in 2013 they decided to eliminate the figure of the CMN. This means that progress in implementing the CMN in the health systems is not linear, no medium level of institutionalisation is guaranteed and backward steps are a reality that requires constant monitoring, which indices such as this can help to achieve.
Aragon has never described the functions of the CMN in any document. This same applies to Madrid, hospital liaison nurses are working in this community.
Advanced level of institutional implementationActive case management nurse. Evidence of their activityThe Canary Islands were pioneers, since they had implemented the CMN (termed community liaison nurse) from the last decade of the 20th century in the provision of domiciliary services. However, the figure was not formalised until 2002 through the “continuous care service protocol for domiciliary care”.
Catalonia also has references for this period of time in specific hospitals within the autonomous region. Currently they have specific regional programmes for the management of chronic patients and therefore CMNs are not available throughout the autonomous region; however, the great majority opt for the CMN.
Andalusia has implemented the CMN since 2002, since they published their Decree 137/2002 of 30 April, in support of Andalusian families (2002) stating that nursing care will be provided in a regulated and continuous fashion, at home, for all elderly people or people with disabilities who require it and as indicated by a doctor or nurse. The community liaison nurse was the case manager to meet this requirement, who later became the community CMN and the hospital CMN.
Valencia, between 2007 and 2010, ran a pilot of a CMN model and then gradually implemented the community CMN and hospital CMN for the entire health service.
Murcia implemented a pilot programme in 2010 with 2 CMNs, with good results. They want to gradually build on this programme.
In 2011, the Basque Country implemented 8 pilot projects with three CMNs, although after analysis of the pilot projects they decided that 3 figures were not necessary and supported 2: the hospital liaison nurse and the advanced skill nurse manager.
In the Balearic Islands and Madrid the hospital liaison nurse is being incorporated in different hospitals. In the Balearic Islands the first references date back to 2002 in the Son Espases University Hospital and in Madrid, they have been functioning since 2009 in the Severo Ochoa University Hospital.
Aragon, after the 8 liaison nurses from each sector had been working for 6 years, decided in 2013 to remove them from the health system, since there were primary care professionals who could take over their functions.
There is scientific evidence for their workThe role and scope of the work undertaken by the CMN where implemented can be monitored based on published scientific evidence. The professionals themselves seek evidence of the results of their clinical practice. This is an important quality standard to establish whether or not these public policies are efficient in coping with chronicity in providing scientific evidence and objective assessment criteria as to whether or not they are resolving a social issue.
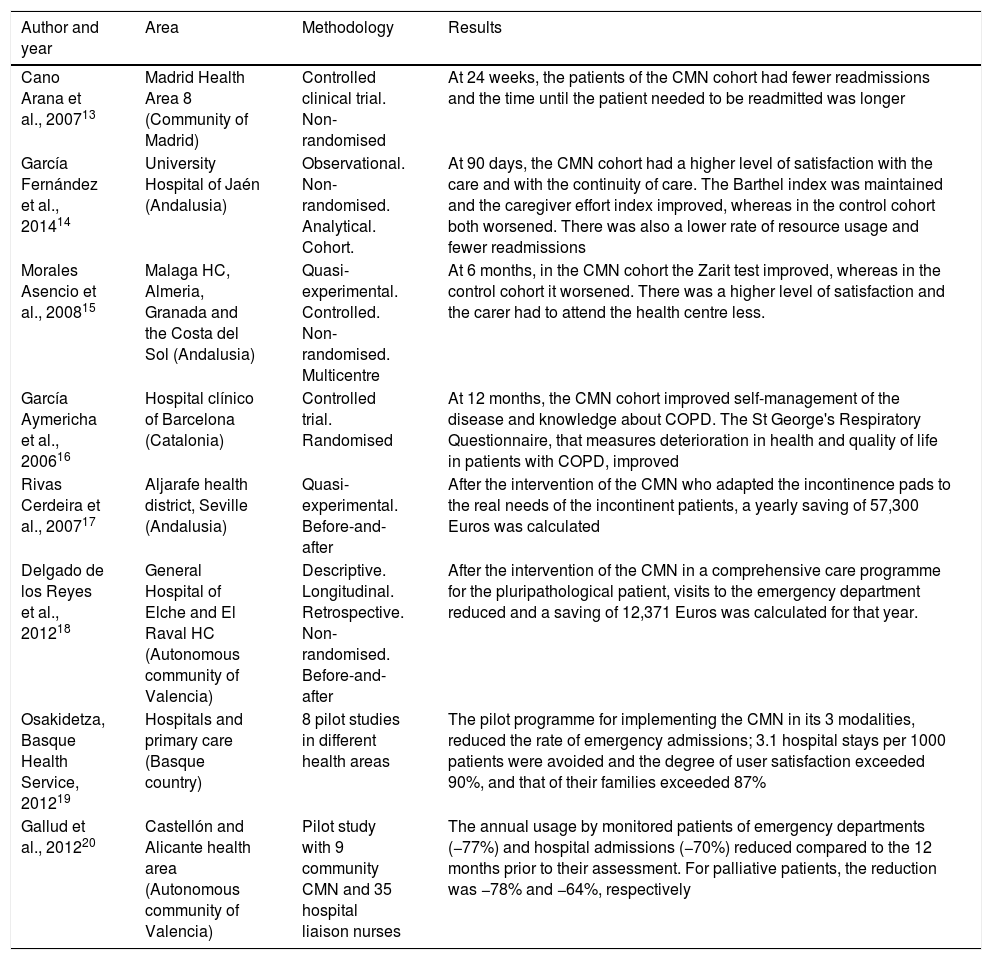
In Andalusia, Catalonia, the Basque Country, Valencia and Madrid there are publications13–20 with measurable data on the work undertaken by the CMN (Table 3) and, although there are still few published studies on the figure, there is a notable group of them that clearly indicate some very positive variables in relation to the quality of life perceived by these patients and their caregivers, their level of satisfaction with the care received, carer overload, the patients’ level of functional dependence and consumption of health resources.
Evidence of the rate of case management nurse interventions in the autonomous regions.
| Author and year | Area | Methodology | Results |
|---|---|---|---|
| Cano Arana et al., 200713 | Madrid Health Area 8 (Community of Madrid) | Controlled clinical trial. Non-randomised | At 24 weeks, the patients of the CMN cohort had fewer readmissions and the time until the patient needed to be readmitted was longer |
| García Fernández et al., 201414 | University Hospital of Jaén (Andalusia) | Observational. Non-randomised. Analytical. Cohort. | At 90 days, the CMN cohort had a higher level of satisfaction with the care and with the continuity of care. The Barthel index was maintained and the caregiver effort index improved, whereas in the control cohort both worsened. There was also a lower rate of resource usage and fewer readmissions |
| Morales Asencio et al., 200815 | Malaga HC, Almeria, Granada and the Costa del Sol (Andalusia) | Quasi-experimental. Controlled. Non-randomised. Multicentre | At 6 months, in the CMN cohort the Zarit test improved, whereas in the control cohort it worsened. There was a higher level of satisfaction and the carer had to attend the health centre less. |
| García Aymericha et al., 200616 | Hospital clínico of Barcelona (Catalonia) | Controlled trial. Randomised | At 12 months, the CMN cohort improved self-management of the disease and knowledge about COPD. The St George's Respiratory Questionnaire, that measures deterioration in health and quality of life in patients with COPD, improved |
| Rivas Cerdeira et al., 200717 | Aljarafe health district, Seville (Andalusia) | Quasi-experimental. Before-and-after | After the intervention of the CMN who adapted the incontinence pads to the real needs of the incontinent patients, a yearly saving of 57,300 Euros was calculated |
| Delgado de los Reyes et al., 201218 | General Hospital of Elche and El Raval HC (Autonomous community of Valencia) | Descriptive. Longitudinal. Retrospective. Non-randomised. Before-and-after | After the intervention of the CMN in a comprehensive care programme for the pluripathological patient, visits to the emergency department reduced and a saving of 12,371 Euros was calculated for that year. |
| Osakidetza, Basque Health Service, 201219 | Hospitals and primary care (Basque country) | 8 pilot studies in different health areas | The pilot programme for implementing the CMN in its 3 modalities, reduced the rate of emergency admissions; 3.1 hospital stays per 1000 patients were avoided and the degree of user satisfaction exceeded 90%, and that of their families exceeded 87% |
| Gallud et al., 201220 | Castellón and Alicante health area (Autonomous community of Valencia) | Pilot study with 9 community CMN and 35 hospital liaison nurses | The annual usage by monitored patients of emergency departments (−77%) and hospital admissions (−70%) reduced compared to the 12 months prior to their assessment. For palliative patients, the reduction was −78% and −64%, respectively |
CMN: case management nurse; COPD: chronic obstructive pulmonary disease.
All the studies, with the exception of the first, confirm that including the CMN – either in a multidisciplinary team or independently – is positive for both patients and the health system alike.
These studies show favourable results for the CMN, as do the pilot programmes undertaken in the different communities.
In their article “New nursing profiles for the comprehensive management of complex chronic and palliative patients in the Community of Valencia”, Valencia set out the results of a pilot study on CMN and hospital liaison nurses and confirmed that they were able to reduce the annual urgent care usage by 77% and hospital admissions by 70% compared to the 12 preceding months.
The Basque Country's pilot programmes together show significantly lower urgent readmission and lower hospital stay rates compared to previous rates. Patient satisfaction and that of their caregivers with the care provided was also over 85% for all the questions posed. However, despite the good results being achieved by the CMN, the professionals viewed this pilot programme differently. Between 35% and 40% of the professionals viewed the intervention of new roles as positive, whereas between 45% and 50% were neutral on the subject, and 13% to 17% negative. There is also a lack of information on the care functions performed by the CMN, since in this pilot programme 29% of the professionals considered that the information they were given was not useful and 39% were neutral on the subject.
Protocolised functionsHaving reached this point, the question is: what are the specific functions that justify the professional profile of the CMN? There is no legal framework that establishes their role in any of the proposals of the autonomous regions. Despite Andalusia constantly alluding to their Decree 137/2002 of 30 April, in support of Andalusian families, the function of the CMN is not regulated. This means that, formally, the CMN role is being constructed in practice without yet having achieved legal or administrative crystallisation. Therefore, the protocols of these 3 autonomous regions are the only framework that we can cling to in an attempt to find acknowledgement for the CMN profile which remains vague and is still struggling to differentiate itself from others, even among the care professionals themselves, as we saw in the previous point.
If we had to summarise and define the functions of the CMN, we would have to start with the protocols and manuals of Andalusia, the Canary Islands and Catalonia, which include the allocated functions. Thus we would find a professional practitioner whose mission is to ensure complex care for chronic patients preventing interruptions between care levels and between the different practitioners, who must, in addition, coordinate with social workers, negotiate with families and informal carers and ensure personalised care through individualised assessment and planning. In the case of Catalonia, the CMN are also in charge of promoting personal and family self care (which is reminiscent of the Dororea Orem model) and preventing the duplication of clinical tests by coordinating between care levels.
The competencies of these professionals are expected to include the capacity to work in multiprofessional teams, the capacity to provide advanced care, manage conflicts and have the skills to communicate and motivate patients and their families, as well as a critical capacity and a desire to innovate and research.
If we had to define a trend among the 3 communities, we could highlight that we found that the importance of this nurse's role in the Canary Islands is to act as a liaison officer to help ensure continuity of care for the patient between the different clinical care levels. In addition to the above Andalusia places the emphasis on integrating the social and health areas, and Catalonia's mission is to ensure self care and the independence of patients and their families, and to prevent repeated diagnostic tests.
Stage 9: Updated protocolised functionsWe included this section because on completion of the standard we had already found greater activity in the community of Andalusia, which differentiates it from the other regions. Every political project runs the risk of becoming exhausted and lost without being definitively implemented. Andalusia has continually reviewed the process, and reviewed and committed to “the model”. In fact, once we had finished our review and confirmed that the community had the most recent protocol of functions (from 2014), we added to the previous information and found that in January 2017 the protocol was further updated to improve and strengthen the case management system. This is why we have placed this community at the apex of the institutionalisation process above the others.
Stage 10: Consolidation, ongoing functioning and legal security compared to other professional groupsNone of the autonomous regions reached this stage. The title of this article already indicates this from the outset. Despite advances made, the model is far from being consolidated and even further from being institutionalised.
The case management model is not, a priori, defining of or exclusive to any specific profession: it is a work methodology that the CMN use to personalise and individualise care. However, there are professions, like social work, that claim this model as their own and, by extension, as part of the functions of the CMN. At one point, these claims on the part of social work generated conflicts in the implementation of the figure of the CMN in some autonomous communities.21,22 At present, other professionals, such as some internal medicine specialists are starting to make these competencies exclusive as references in complex chronic disorders or pluripathology.23 For all of these reasons, the commitment of these autonomous communities to implementing nurse-lead case management with good results in professional practice and patient health should be accompanied by a defined legal framework that ensures the professional security and survival of the CMN.
Where is the model headed? A conclusion left openThe most recent institutional document of the autonomous region of Andalusia (2016) shows the threat to the model posed by a failure to institutionalise the figure of the CMN and the risk of regression, even 15 years after its implementation: the progress of case management over these years has been heterogeneous among the diverse institutions that constitute our system (the Andalusian system), driven more by the developed professional competencies, by the varying support from management teams, and by local resources than by changes in the needs and strategies of the system. For example, a lack of institutionalisation influenced the removal of the CMN figure in the community of Aragon.
It is true, as the Nobel Laureate in Economics, Douglass C. North states, that all processes of institutionalisation require a mix of formal and informal procedures, the latter being equally or more important than the former. Acknowledging the specific profile of the CMN requires a knowledge and understanding of the differentiated nature of the role by the nursing profession itself. Once this informal acknowledgement has been achieved, it is the responsibility of the nursing profession to promote this case management nurse profile and to fight for its institutional recognition.
Another element to be taken into account is that policies only enter and, in particular, stay on institutions’ agendas if they clearly answer socially identified issues. It is then that policies are forced to direct governments towards resolving these issues. The key question is, if there are obvious results from the actions of the CMN on problems arising from chronicity and complex chronicity: why has their profile not been consolidated on the institutional agendas?
There is political and social agreement in the health systems of all the autonomous regions to provide a social and health care response to the problem of chronic disorders. This is a first step, but it is not enough if what is agreed is not reflected in policies and strategic planning. And the regions that, more than 5 years after signing up to the National Strategy for the Care of Chronicity, are still not achieving an advanced level in implementing the figure of the CMN are increasingly lagging behind those that are leading the way forward.
There is also a willingness to establish clear objectives and goals, but this only applies to the professionals who are concerned and busy promoting the role of the CMN, and not the regional governments that, to date, have agreed “recommendations” and nothing else. Even the most advanced administrations acknowledge that the efforts of professionals will have been in vain if the formal institutions fail to drive the issue in the same way.
Furthermore, we can state that we have tools to evaluate attainment of the model, but they have still failed to definitively cross the barrier put up by the public agendas. We must continue to assess the work of the CMN to demonstrate to the profession that the figure has a true and necessary profile that provides answers to citizen's health needs, specifically in the case of complex, chronic disorders.
No specific obligations or rights have been established for the relevant players, either. Significant legal aspects are missing, such as specific recognition of the CMN beyond the health plans, which create administrative practice but fail to ensure either continuity or a formal institutional framework.
Authorship/collaborationsMLP contributed to the choice of study subject, the literature search, processing the information and drafting the initial paper.
JPA contributed to the methodology and the reference standard design, and to editing the version for publication.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: López Vallejo M, Puente Alcaraz J. El proceso de institucionalización de la enfermera gestora de casos en España. Análisis comparativo entre los sistemas autonómicos de salud. Enferm Clin. 2019;29:107–118.