Knowing the profile of cardiovascular morbidity, degree of control and lifestyles in type 2 diabetes.
MethodRandomised multicenter cross-sectional study conducted in 2015 in primary care with 129 diabetics. It included sociodemographic variables, microvascular and macrovascular complications, organic damage, comorbidity and lifestyles of smoking, exercise and adherence to Mediterranean diet. Metabolic control was assessed with the latest annual glycosylated haemoglobin.
Results57% were men and 43% women. Metabolic control was acceptable (HbAc1%, 7.15%) without differences by town. 74.4% had cardiovascular comorbidity and the 99.2% risk factors. 23% were smokers and 41% sedentary with a 56% adherence to Mediterranean diet.
ConclusionsThe cardiometabolic profile of diabetes includes retinopathy, peripheral arterial disease, comorbidity of hypertension and cardiovascular risk factors. Individual or group health education in self-care and healthy lifestyles can improve metabolic control.
Conocer el perfil de morbilidad cardiovascular, grado de control y estilos de vida en diabetes tipo 2.
MétodoEstudio transversal multicéntrico aleatorizado realizado en 2015 en atención primaria con 129 diabéticos. Incluyó variables sociodemográficas, complicaciones micro- y macrovasculares, daño orgánico, comorbilidad y estilos de vida de tabaquismo, ejercicio y adherencia a dieta mediterránea. El control metabólico se valoró con la última hemoglobina glucosilada anual.
ResultadosEl 57,4% eran hombres y el 42,6% mujeres. El control metabólico fue aceptable (HbAc1%, 7,15%) sin diferencias por municipio. El 74,4% tenía comorbilidad cardiovascular y el 99,2% factores de riesgo. El 23,3% era fumador y el 41,1% sedentario, con una adherencia a dieta mediterránea del 56%.
ConclusionesEl perfil cardiometabólico de diabetes incluye retinopatías, enfermedad arterial periférica, comorbilidad de HTA y múltiples factores de riesgo cardiovascular. La educación para la salud individual o grupal en autocuidados y estilos saludables puede mejorar el control metabólico.
Diabetes mellitus type 2 is a cardiovascular disease of increasing prevalence. It is usually associated with low diagnosis and undetected risk factors and microvascular complications.
What is offered?A multicentre study which provides the morbidity profile, micro and macrovascular complications, organ damage and type 2 lifestyles of diabetic patients who regularly present at primary health care centres.
Diabetes mellitus type 2 (DM2) is a worldwide problem of relevance. In 2013 the WHO declared it to be the 8th highest cause of mortality in the world.1 Given the high population load of cardiovascular risk factors (CVRF) and genetic susceptibility, predictions indicate a growing prevalence2 over upcoming years. According to a recent study, in Spain the prevalence of known, unknown and total diabetes is 7.78%, 6.01% and 13.79%.3 It has been estimated that in the Community of Madrid the figures are 6.3%, 1.8% and 8.1%,4 respectively and of those known cases, 5.4% have primary care follow-up.4 The most relevant consequences are micro- and macrovascular complications, the increase of vascular age,5 a higher risk of mortality due to coronary disease6 and a deterioration in quality of life. Multifactorial intervention in modifiable CVRF in patients with DM2 has demonstrated a reduction in complications7 and mortality associated with cardiovascular episodes. Specifically, life styles associated with CVRF play an essential role in the prevention, appearance and progress of the disease. One of the most relevant studies in diabetes highlights the importance of intervening in these lifestyles.8 Giving up smoking, a hypocalorific diet poor in fat and the increase in physical activity improves metabolic control of the disease.9,10 The aim of this research is to become aware of the cardiovascular morbidity profile, the degree of metabolic control and lifestyles of the DM2 patients within the primary care attention area.
MethodWe conducted a transversal, multicentre randomised study in 2015 of the Brunete, Quijorna and Villafranca del Castillo health centres which belongs to the areas of Villanueva de la Cañada (North West Healthcare Service of the Madrid Health Service). The study population were people of both genders, aged between 35 and 72. The main inclusion criteria was a diagnosis of DM211 of over one-year duration in the electronic clinical record. The study sample was provided by the primary care research committee. It was representative of the known prevalence in the whole of the basic area, with a 95% confidence level in a total population of 450 people diagnosed and a study precision of 5%. The final sample was of 129 patients, randomised from the data base of known diabetics and stratified according to municipality and gender, depending on the total population of the basic health area. Socio-demographic variables were collected with an administered study questionnaire (age, sex, marital status and educational level) and variables of the clinical record related to DM2 (years of duration, presence in other family members and current treatment), presence of microvascular, macrovasuclar complications, organic damage and known comorbidity. The CVRF collected were not modifiable (age, family history) and modifiable such as obesity (BMI≥30kg/m2), abdominal obesity in ATP-III criterion12 (abdominal perimeter in men ≥102cm and ≥88cm in women) and diagnosis of hypercholesterolemia (serum cholesterol ≥200mg/dl) and hyperglycaemia (triglycerides ≥150mg/dl). In the study questionnaire lifestyles were also included as were tobacco habits (type and number of cigarettes per day), daily physical activity (work and leisure) and programmed daily or weekly physical activity, together with the percentage of adherence to a Mediterranean diet (DietMet) measured by a 14-item questionnaire validated in Spain.13 The degree of metabolic control was measured with glycosilated haemoglobin (HbAc1%) from the previous year's analysis. Statistical analysis was carried out with the SPAA software package version 21.0. Qualitative variables were expressed with relative frequencies and the normality of quantitative variables were confirmed with the application of parametric tests. The Chi-square test was used for qualitative variables between independent groups and the Student t-test was confirmed with the ANOVA technique for variance analysis for more than 2 groups, when necessary. The level of significance used in the different contrast of hypothesis was a value of P<0.05.
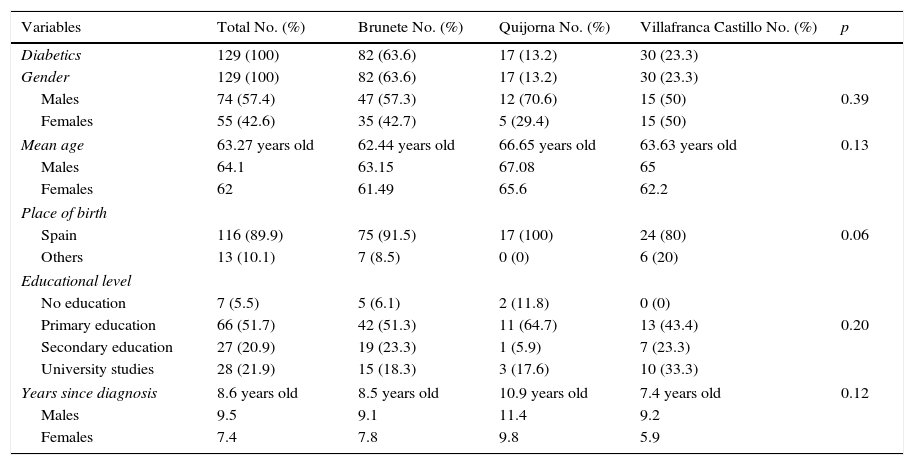
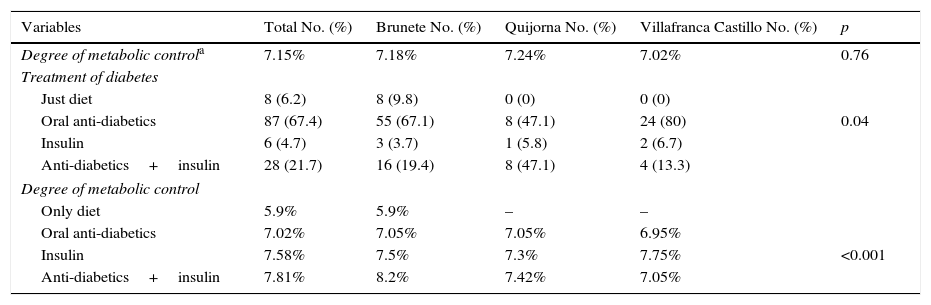
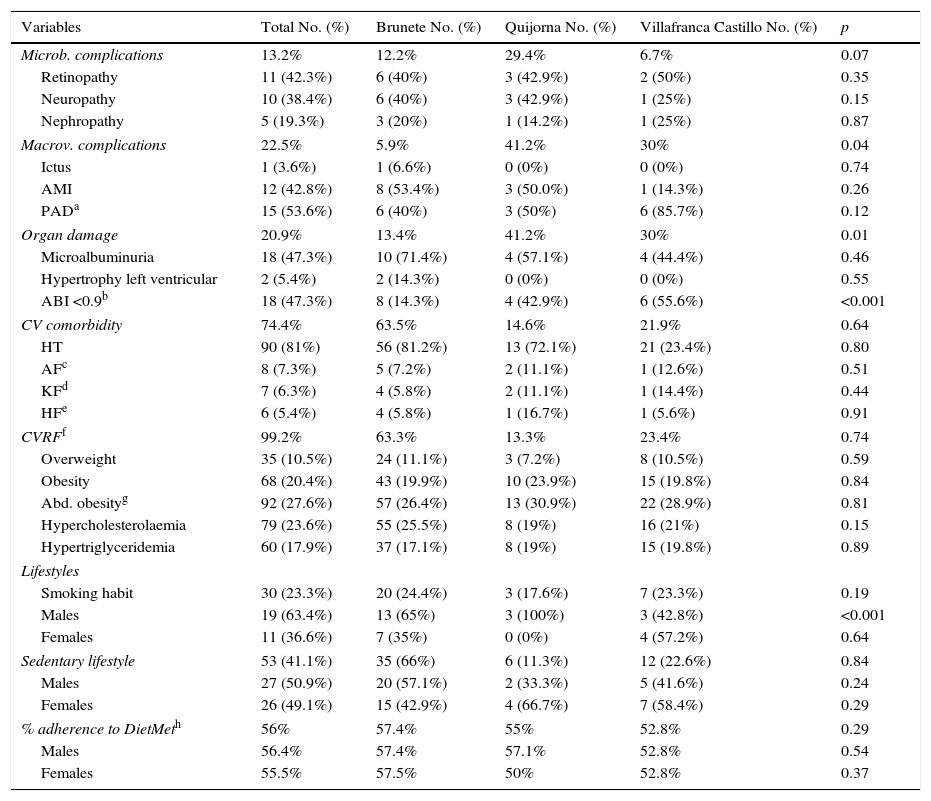
ResultsOf the 129 patients with DM2 included in the study, 63.6% belonged to the municipality of Brunete, 13.2% to Quijorna and 23.3% to Villafranca del Castillo. According to the total population of each of them, known prevalence of DM2 was at rates of 4%, 8%, 8.1% and 6.4%, respectively. With regards to the socio-demographic variables (Table 1), there was a higher sample proportion of males (57.4% vs 42.6%), with a higher mean age of 64 years±7.2 vs 62±8.6 and disease duration (9.5 vs 7.4 years) than females. According to that observed in Table 2, the degree of overall metabolic control was acceptable (HbAc1% 7.15%) with no significant differences for gender, with Quijorna as the municipality with the poorest control (7.24%). Standard treatment for DM2 was with oral antidiabetics (67.4%) with significant statistical differences existing between metabolic control and type of treatment. The combination of oral antidiabetics and insulin was that it had the poorest indicator (HbA1c 7.8%, P<0.001). Table 3 lists the complications, comorbidity, organ damage, cardiovascular profile and life style of the DM2 patients from the study sample. The prevalence of microvascular complications was 13.2% (95% CI 6.95–19.40), with retinopathy being the highest complication in all municipalities. There was a 22.5% rate of macrovascular complications (95% CI 14.88–30.07) and a 20.9% of organ damage (95% CI 13.52–28.33) with statistically significant differences per centre. In all of them microalbuminuria and peripheral arterial disease were the markers of organ damage and macrovascular complication was the most prevalent except in Brunete, which was a history of acute myocardial infarction. Comorbidity associated with diabetes was present in 74.4% (95% CI 66.50–82.33) of the population with an HT diagnosis in 8 out of 10 diabetics. Nearly all of the patients in the study (99.2%, 95% CI 95.75–99.98) had CVRF with an almost uniform distribution rate of each one of them, although with a greater presence of abdominal obesity (71.3%, 95% CI 63.12–79.51) compared with the rest. Regarding lifestyles, 23.3% were smokers (95% CI 15.57–30.93) with a much higher proportion of men smokers compared with women in each of the municipalities (P<0.001). 41.1% of the population were declared sedentary with Brunete being the municipality with the highest proportion (66%). By gender, in the other municipalities the women were more physically active (66.7% in Quijorna and 58.4% in Villafranca) compared with men. The mean adherence to the DietMet was 56% with no significant differences by gender although they did exist by municipality (Brunete 57.4% vs Villafranca 52.8%).
Socio-demographic variables.
| Variables | Total No. (%) | Brunete No. (%) | Quijorna No. (%) | Villafranca Castillo No. (%) | p |
|---|---|---|---|---|---|
| Diabetics | 129 (100) | 82 (63.6) | 17 (13.2) | 30 (23.3) | |
| Gender | 129 (100) | 82 (63.6) | 17 (13.2) | 30 (23.3) | |
| Males | 74 (57.4) | 47 (57.3) | 12 (70.6) | 15 (50) | 0.39 |
| Females | 55 (42.6) | 35 (42.7) | 5 (29.4) | 15 (50) | |
| Mean age | 63.27 years old | 62.44 years old | 66.65 years old | 63.63 years old | 0.13 |
| Males | 64.1 | 63.15 | 67.08 | 65 | |
| Females | 62 | 61.49 | 65.6 | 62.2 | |
| Place of birth | |||||
| Spain | 116 (89.9) | 75 (91.5) | 17 (100) | 24 (80) | 0.06 |
| Others | 13 (10.1) | 7 (8.5) | 0 (0) | 6 (20) | |
| Educational level | |||||
| No education | 7 (5.5) | 5 (6.1) | 2 (11.8) | 0 (0) | |
| Primary education | 66 (51.7) | 42 (51.3) | 11 (64.7) | 13 (43.4) | 0.20 |
| Secondary education | 27 (20.9) | 19 (23.3) | 1 (5.9) | 7 (23.3) | |
| University studies | 28 (21.9) | 15 (18.3) | 3 (17.6) | 10 (33.3) | |
| Years since diagnosis | 8.6 years old | 8.5 years old | 10.9 years old | 7.4 years old | 0.12 |
| Males | 9.5 | 9.1 | 11.4 | 9.2 | |
| Females | 7.4 | 7.8 | 9.8 | 5.9 | |
Degree of metabolic control and treatment of diabetes.
| Variables | Total No. (%) | Brunete No. (%) | Quijorna No. (%) | Villafranca Castillo No. (%) | p |
|---|---|---|---|---|---|
| Degree of metabolic controla | 7.15% | 7.18% | 7.24% | 7.02% | 0.76 |
| Treatment of diabetes | |||||
| Just diet | 8 (6.2) | 8 (9.8) | 0 (0) | 0 (0) | |
| Oral anti-diabetics | 87 (67.4) | 55 (67.1) | 8 (47.1) | 24 (80) | 0.04 |
| Insulin | 6 (4.7) | 3 (3.7) | 1 (5.8) | 2 (6.7) | |
| Anti-diabetics+insulin | 28 (21.7) | 16 (19.4) | 8 (47.1) | 4 (13.3) | |
| Degree of metabolic control | |||||
| Only diet | 5.9% | 5.9% | – | – | |
| Oral anti-diabetics | 7.02% | 7.05% | 7.05% | 6.95% | |
| Insulin | 7.58% | 7.5% | 7.3% | 7.75% | <0.001 |
| Anti-diabetics+insulin | 7.81% | 8.2% | 7.42% | 7.05% | |
Complications, comorbidity, cardiovascular risk factors and lifestyles.
| Variables | Total No. (%) | Brunete No. (%) | Quijorna No. (%) | Villafranca Castillo No. (%) | p |
|---|---|---|---|---|---|
| Microb. complications | 13.2% | 12.2% | 29.4% | 6.7% | 0.07 |
| Retinopathy | 11 (42.3%) | 6 (40%) | 3 (42.9%) | 2 (50%) | 0.35 |
| Neuropathy | 10 (38.4%) | 6 (40%) | 3 (42.9%) | 1 (25%) | 0.15 |
| Nephropathy | 5 (19.3%) | 3 (20%) | 1 (14.2%) | 1 (25%) | 0.87 |
| Macrov. complications | 22.5% | 5.9% | 41.2% | 30% | 0.04 |
| Ictus | 1 (3.6%) | 1 (6.6%) | 0 (0%) | 0 (0%) | 0.74 |
| AMI | 12 (42.8%) | 8 (53.4%) | 3 (50.0%) | 1 (14.3%) | 0.26 |
| PADa | 15 (53.6%) | 6 (40%) | 3 (50%) | 6 (85.7%) | 0.12 |
| Organ damage | 20.9% | 13.4% | 41.2% | 30% | 0.01 |
| Microalbuminuria | 18 (47.3%) | 10 (71.4%) | 4 (57.1%) | 4 (44.4%) | 0.46 |
| Hypertrophy left ventricular | 2 (5.4%) | 2 (14.3%) | 0 (0%) | 0 (0%) | 0.55 |
| ABI <0.9b | 18 (47.3%) | 8 (14.3%) | 4 (42.9%) | 6 (55.6%) | <0.001 |
| CV comorbidity | 74.4% | 63.5% | 14.6% | 21.9% | 0.64 |
| HT | 90 (81%) | 56 (81.2%) | 13 (72.1%) | 21 (23.4%) | 0.80 |
| AFc | 8 (7.3%) | 5 (7.2%) | 2 (11.1%) | 1 (12.6%) | 0.51 |
| KFd | 7 (6.3%) | 4 (5.8%) | 2 (11.1%) | 1 (14.4%) | 0.44 |
| HFe | 6 (5.4%) | 4 (5.8%) | 1 (16.7%) | 1 (5.6%) | 0.91 |
| CVRFf | 99.2% | 63.3% | 13.3% | 23.4% | 0.74 |
| Overweight | 35 (10.5%) | 24 (11.1%) | 3 (7.2%) | 8 (10.5%) | 0.59 |
| Obesity | 68 (20.4%) | 43 (19.9%) | 10 (23.9%) | 15 (19.8%) | 0.84 |
| Abd. obesityg | 92 (27.6%) | 57 (26.4%) | 13 (30.9%) | 22 (28.9%) | 0.81 |
| Hypercholesterolaemia | 79 (23.6%) | 55 (25.5%) | 8 (19%) | 16 (21%) | 0.15 |
| Hypertriglyceridemia | 60 (17.9%) | 37 (17.1%) | 8 (19%) | 15 (19.8%) | 0.89 |
| Lifestyles | |||||
| Smoking habit | 30 (23.3%) | 20 (24.4%) | 3 (17.6%) | 7 (23.3%) | 0.19 |
| Males | 19 (63.4%) | 13 (65%) | 3 (100%) | 3 (42.8%) | <0.001 |
| Females | 11 (36.6%) | 7 (35%) | 0 (0%) | 4 (57.2%) | 0.64 |
| Sedentary lifestyle | 53 (41.1%) | 35 (66%) | 6 (11.3%) | 12 (22.6%) | 0.84 |
| Males | 27 (50.9%) | 20 (57.1%) | 2 (33.3%) | 5 (41.6%) | 0.24 |
| Females | 26 (49.1%) | 15 (42.9%) | 4 (66.7%) | 7 (58.4%) | 0.29 |
| % adherence to DietMeth | 56% | 57.4% | 55% | 52.8% | 0.29 |
| Males | 56.4% | 57.4% | 57.1% | 52.8% | 0.54 |
| Females | 55.5% | 57.5% | 50% | 52.8% | 0.37 |
Percentage of adherence to Mediterranean diet measured by a 14 item questionnaire validated in Spain.
Source: Martínez-González et al.13
Diabetes mellitus is a highly prevalent health problem which has become one of the main challenges to public health in the 21st century. In our study, the known prevalence of DM2 in the municipalities studies was slightly lower than that estimated for Spain3 and in the Community of Madrid.4 This may be explained by population differences or low diagnosis due to undiagnosed diabetes and in particular in ethnic groups who represent approximately 10% of the population. The degree of control leaves a lot to be desired (HbA1c 7.1%) but is in line with other population studies conducted in Spain14,15 and with the proportion of diabetics (54.3% of the total) with good metabolic control (HbA1c<7%).16 The outcome of our study reveals a DM2 risk profile associated with the following complications: retinopathy, microalbuminuria and peripheral arterial disease, comorbidity in HT, presence of several CVRF, including abdominal obesity and poor metabolic control associated with specific treatment with insulin and oral antidiabetics. With regards to differences in gender, there was a higher proportion of diabetic men with a longer evolution of the disease. With these results, certain primary prevention strategies could be effective, such as recruitment of patients at risk from primary healthcare centres and a better control of pre-diabetic patients.17 In secondary prevention, health education in diabetes is one of the strategies with the highest impact on control and follow-up of the disease and the essential pillar of treatment.18 Health education specifically led by nursing professionals has changed the focus of attention of the patient with DM2 in the last few years19 with programmes covering different strategies within a continuous and integral process of the disease.20 Moreover, clinical practice guides back up the claim with evidence that education in diabetes, an intervention they consider to play an active part in the self-care of patients, together with group training, improve glycaemic control.21 Within these educational interventions lifestyles play an essential role. The latest recommendations in diabetes22 insist on a healthy heart diet in keeping with Mediterranean diet guidelines, regular aerobic physical activity of moderate intensity and withdrawal from a smoking habit. In our research there were relevant differences by municipality in tobacco smoking, sedentary lifestyle and adherence to the DietMet. An optimum degree of metabolic control (HbAc1%<7%) was associated with better adherence to DietMet (58.5 compared with 53.15% in HbAc1%>7%) and regular physical activity (57.9% of non sedentary diabetics compared with 42.1% with inactivity). By municipality, Brunete had a higher proportion of micro- and macrovascular complications, smokers (66.7%) and patients with a sedentary lifestyle (66%) but a higher adherence to DietMet (57.4%). To conclude, although the indicators are still far from perfect, within the area of primary health, intensive nursing interventions for users to stop smoking, foster greater adherence to DietMet and reduce sedentary lifestyle could improve metabolic control and cardiovascular risk in patients with DM2.
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to thank all our colleagues at the health centres Brunete, Quijorna and Villafranca del Castillo and the primary care team of Villanueva de la Cañada (Madrid).
Please cite this article as: Pérez-Manchón D, Rodríguez-Álvarez ML, Alcívar-Arteaga C, Redondo-Pico M, Ramos-Quirós E. Barómetro de diabetes tipo 2 en atención primaria. Control metabólico, estilos de vida y perfil de morbilidad. Enferm Clin. 2017;27:369–374.