We present a case of spinal infection due to a defective strain of Streptococcus intermedius, whose diagnosis was facilitated by the use of multiplex PCR.
The patient was a 70-year-old male with type 2 diabetes mellitus admitted for 15-day low back pain with deterioration of his general condition and fever. He denied previous trauma. On examination, he presented pain on palpation in the lumbar spine with negative sacroiliac maneuvers, and in the analysis, he presented leukocytosis of 23.9×109/l (84.2% neutrophils) with C-reactive protein of 23.24mg/dl. Empirical treatment with ceftriaxone was initiated.
The MRI performed 2 days later showed images compatible with erosive septic arthritis of the left interapophysial lumbar facets at L4–L5 level and several epidural and paravertebral collections compatible with abscesses. Surgery was performed to drain the paravertebral collections, and samples were sent to microbiology.
Gram staining showed a high number of polymorphonuclear leukocytes, but no microorganisms. Cultures were made on agar-blood and agar-chocolate plates (incubated in CO2), Schaedler medium (anaerobiosis) and enriched thioglycolate broth. After 18h of incubation no medium showed growth, so a portion of the sample was diluted with physiological serum and a multiplex PCR was performed (BCID, FilmArray®, Biofire), with a positive result for Streptococcus spp., being negative for S. pyogenes, S. agalactiae and S. pneumoniae.
After 48h of incubation, all solid media remained negative and a Gram stain of the thioglycolate broth showed gram-positive cocci in chains, despite which no growth was obtained in the subcultures to solid media.
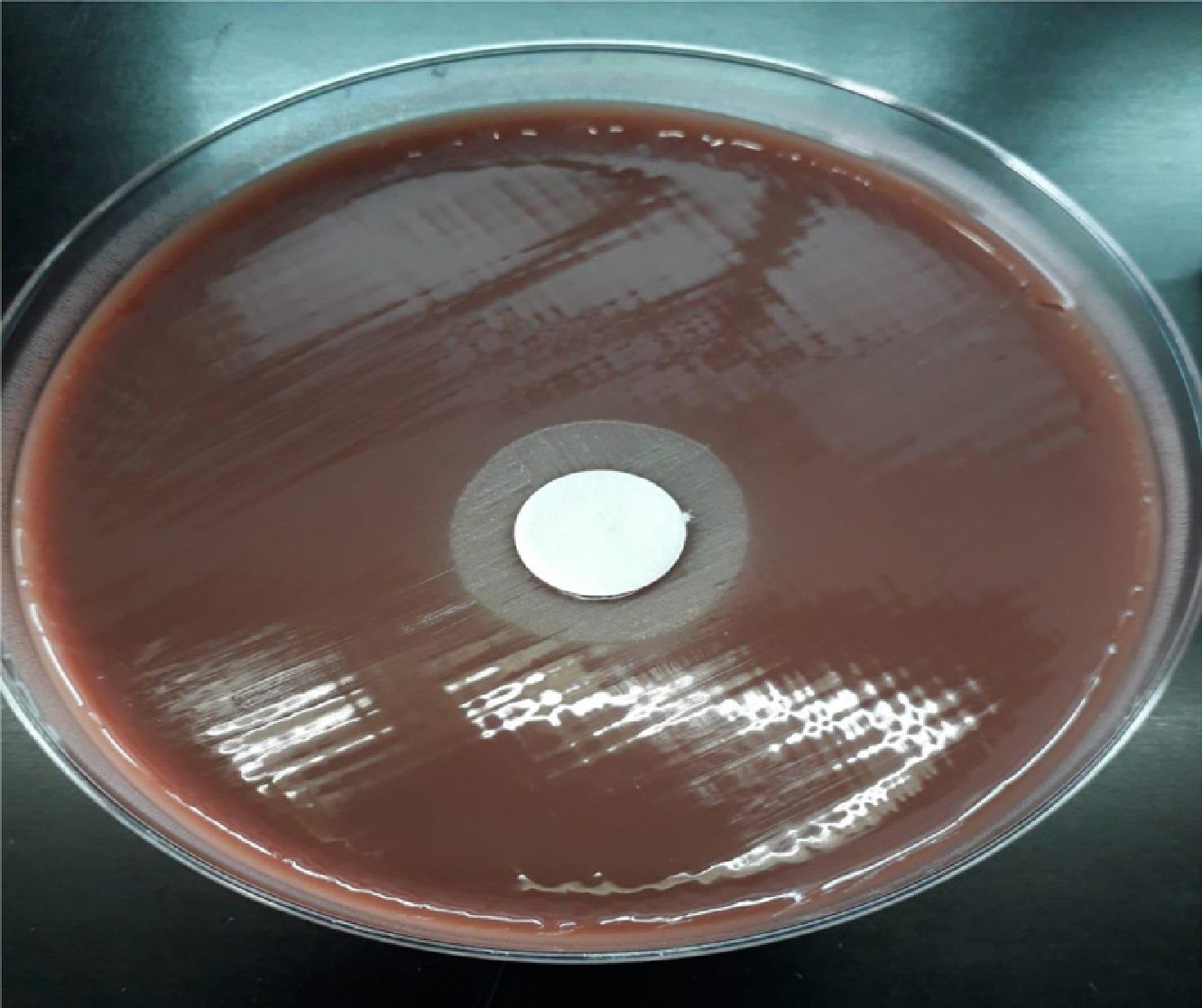
On suspicion of a nutritionally deficient strain, new subcultures of the broth were made, placing paper discs (BBLTM TaxoTM) impregnated with 0.001% pyridoxine hydrochloride on the plates. After nocturnal incubation, satellite colonies appeared around the discs (Fig. 1).
A portion of the thioglycolate broth was inoculated in a vial of anaerobic blood culture (BD BACTEC Plus Anaerobic/F), which showed growth at 33h of incubation. After subcultures of this vial, sufficient growth was achieved in the habitual media, without the need to be supplemented for the subcultures or for carrying out the identification and antibiogram tests.
Identification was made using the API® 20 Strep system (bioMerieux), with a 91.2% success rate for S. intermedius, coinciding with that obtained by MALDI-TOF (Bruker) and was confirmed at the National Centre for Microbiology.
In the antibiogram with discs and gradient strips, the strain showed sensitivity to penicillin G, amoxicillin, cefotaxime, erythromycin and clindamycin.
This microbiological finding led to the suspicion of an odontogenic origin of the infection, consulting with the maxillofacial surgery department, which proceeded to extract 7 affected teeth. A transesophageal echocardiogram ruled out the existence of vegetation. The patient evolved favorably, with resolution of the condition after treatment with ceftriaxone IV for 20 days and subsequently oral amoxicillin, until 6 weeks were completed.
S. intermedius is part of the oropharyngeal microbiota, the gastrointestinal tract and the genitourinary tract.1 More than 40% of clinical isolates come from dental plaque, with haematogenous spread having been reported in both surgical and conservative procedures,2 and is a major cause of serious infections, including brain and liver abscesses,3 particularly in diabetic patients, with cancer or cirrhosis.2–5 Epidural spinal abscess can be fatal in more than 16% of cases. Patients typically present with fever and acute pain located in the neck or back.2
Cases with negative culture have been described when antibiotic therapy is established prior to sample collection,4,6 but the novelty of our case is that growth was only obtained after supplementation with pyridoxine hydrochloride. The Streptococcus strains, known as nutritionally deficient variants, were transferred to other genera in 1995,7 therefore, our case is the first in which a defective S. intermedius strain has been isolated. It is known that commercial media for blood cultures contain pyridoxal and allow the growth of these strains, while the habitual media do not do so unless they are supplemented.
Molecular techniques offer a fast, effective alternative for the detection of pathogens in clinical samples, especially when the culture is negative.6,8 In our case, the use of FilmArray® equipment allowed us to make the microbiological diagnosis, confirming the usefulness of the BCID panel in samples other than blood, as other authors had suggested.9
Please cite this article as: Ortiz de la Tabla V, Infante A, Jover F. Infección espinal por una cepa defectiva de Streptococcus intermedius diagnosticada mediante PCR multiplex. Enferm Infecc Microbiol Clin. 2020;38:245–246.