During the final phase of measles elimination rigorous investigation of each individual case becomes fundamental to confirm or discard cases, particularly among vaccinated people, since they experience a milder disease, and laboratory diagnosis is more complex. Our study focused in the epidemiology of measles in vaccinated people.
MethodsLongitudinal study on measles cases in two dose vaccinated people in Spain from 2003 to 2014.
ResultsWe confirmed 138 measles cases (90 of them, laboratory confirmed) in people with two doses of vaccine. The median of time from last vaccination to rash onset showed a lineal trend (p<0.001), in parallel with the number of doses of vaccine received (0, 1, 2 doses). Among confirmed cases, the hospitalisation risk decreased inversely proportional to the number of administered vaccine doses (linear trend, p<0.001). Only in 23.9% of confirmed cases and 50% of discarded cases the guidelines about sample taking were fulfilled. 50% of samples in two dose vaccinated people were taken without fulfilling time delay criteria. 16.7% (36/215) of discarded cases with a negative IgM result did correspond to samples taken early (first 72h after rash) and could represent false negatives.
ConclusionOur results highlight the importance of fulfilling properly the guidelines for laboratory diagnosis in order to confirm or discard every measles case, especially in two dose vaccinated people. When a negative IgM result is obtained in early samples a new IgM test should be practiced, as well as a PCR test, in order to avoid infra-detection of cases.
En la fase de eliminación del sarampión, reviste especial importancia la investigación de cada caso sospechoso, especialmente en personas vacunadas, pues en ellas la clínica es más leve, y los resultados de laboratorio más difíciles de interpretar. Nuestro estudio se centró en la epidemiología del sarampión en personas vacunadas.
MétodosSe realizó un estudio longitudinal de los casos de sarampión en personas vacunadas notificados en España entre 2003 y 2014.
ResultadosSe observaron 138 casos confirmados de sarampión en personas vacunadas con 2 dosis, 90 de ellos confirmados por laboratorio. La mediana de tiempo entre la última dosis de vacuna recibida y la aparición del exantema mostró una tendencia lineal creciente (p<0,001) en función de las dosis de vacuna (0, 1, 2 dosis). El riesgo de hospitalización disminuyó de forma inversamente proporcional al número de dosis de vacuna recibidas (p<0,001). Solo en el 23,9% de los casos confirmados y en el 50% de los descartados, se cumplió el protocolo de recogida de muestras clínicas. En el 50% de los casos estudiados en vacunados con 2 dosis, las muestras se tomaron precozmente. El 16,7% de los descartados mediante IgM negativa podrían ser falsos negativos, pues procedían de muestras precoces.
ConclusiónNuestros resultados evidencian la importancia de cumplir el protocolo diagnóstico para confirmar o descartar casos de sarampión, especialmente en los vacunados con 2 dosis. Ante una IgM negativa en muestras precoces, sería necesario obtener una nueva muestra y realizar un nuevo test de IgM, así como la prueba de PCR.
In recent decades we have witnessed a dramatic reduction in the morbidity and mortality associated with measles thanks to the generalised use of the vaccine.1 Measles is an eliminable disease because its reservoir is exclusively human, it is difficult for the agent to survive in the atmosphere and in addition to good diagnostic techniques, there is an effective and economical vaccine that induces lasting immunity.2 Elimination entails interrupting the endemic transmission of the measles virus in a region for at least 12 months, under a high quality surveillance system.3 The European Region of the World Health Organisation (WHO) set the objective of eliminating measles in 2015.4,5 This study falls within the Spanish National Plan for the Elimination of Measles and Rubella,6 included in the European strategy for the elimination of measles and rubella.5,7 Despite efforts, in recent years, various outbreaks of measles have been reported in Spain and in other European countries,8–10 most between 2010 and 2012.
In areas with high vaccine coverage, a new case of measles generates few secondary cases, but a major proportion of these will be people who have been vaccinated.11 In these cases, the disease might be due to primary vaccine failure (no initial response) or secondary vaccine failure (due to waning immunity, or, less commonly, due to their antibodies’ lack of neutralising capacity). Waning implies an attenuated immune response, not sufficient to prevent the disease, because the levels of measles-specific antibodies are lower in vaccinated individuals than in those exposed to the wild virus.12,13 In vaccinated persons, measles is less contagious and the symptoms are milder.14,15
The main strategies of the WHO to accelerate the elimination of measles in the European Region are to maintain the population's immunity to measles, reinforce the surveillance protocol (investigating each suspicious case in a timely and thorough manner in the laboratory), establish means for controlling transmission, establish the circulation of the virus, and verify its elimination.3,6
In vaccinated persons, it is more difficult to confirm or discard suspicious cases, since the viral load is less, and serology for IgM in the first days after onset of the rash might be negative, even in true measles cases. Some studies recommend complementing routine diagnostic methods with techniques such as the high IgG avidity test, or the IgG quantitative test.15,16 In the final phase of elimination, with very low incidence rates, suspected measles in vaccinated persons must be thoroughly investigated, especially if they have received 2 doses of the vaccine.
The principal objective of the study was to analyse the features of suspected measles in persons vaccinated with two doses, notified to the Spanish National Plan for the Elimination of Measles between 2003 and 2014, and to examine how the laboratory procedures (taking clinical samples and tests performed) adapt to the current surveillance protocol.
MethodologyFollowing the measles surveillance protocol17 of the National Epidemiological Surveillance Network (RENAVE), we used the following case definitions:
- •
Laboratory-confirmed case: meets clinical and laboratory criteria, not recently vaccinated (21 days before onset of the rash), or recently vaccinated but presenting the wild genotype of the virus. Confirmation is by positive IgM in serum (of choice) and/or positive PCR in urine/pharyngeal exudate.
- •
Epidemiological link confirmed case: meets the clinical criteria and has an epidemiological link with a laboratory-confirmed case.
- •
Clinically compatible case: meets the clinical criteria but not possible to take samples for serological confirmation, and there is no epidemiological link with a laboratory-confirmed case. In large outbreaks (2010–2012), given the difficulty of investigating all the cases in the laboratory, a large part were classified as “clinically compatible”, meaning they were highly likely to be true cases of measles. These cases were considered “confirmed” in the analysis.
- •
Discarded case: meets the clinical criteria for measles, with negative laboratory results or with epidemiological link with a laboratory-confirmed case of another exanthematous disease. A negative IgM result results in a case being discarded. A negative PCR, on its own, does not result in a case being discarded.
- •
All suspected cases of measles should be notified and investigated, taking timely samples of serum (from the fourth day after onset of the rash, but never later than the twenty-eighth day), and urine and/or pharyngeal exudate (within 7 days of onset of the rash). If the IGM is negative in serum collected in the first 72h a second sample must be taken between days 4 and 28, in the absence of another confirmatory result.17
A retrospective, cohort study was designed that included all suspected cases of measles notified to the Spanish National Plan for the Elimination of Measles between 2003 and 2014. Layers were created according to vaccination status, age group and case classification (confirmed/discarded). The incidence of measles was calculated by age group, relative risk (RR) of confirmation of measles in suspected cases according to age group and the number of vaccine doses received, as well as the RR of hospitalisation in confirmed cases. The RR with its confidence interval was calculated based on the odds ratio (OR), using Kleinbaum's method for rare diseases.18 The variables studied were: year, case classification, age, age group (<5 years, 5–19 years, 20 years or older), date of rash onset, hospitalisation, number of vaccine doses (a vaccine dose administered at least 21 days prior to onset of rash was considered valid, this is the time required for the immune response to develop), date of last vaccine dose, difference in years between the date of the rash and the date of the last vaccination, samples collected (only serum, only urine and/or exudate, both), test performed to confirm/discard (only IgM, only PCR, both), and the difference in days between the date of the firs serum sample and the date of onset of rash.
The quantitative variables were described by their mean and standard deviation (or median and interquartile range in non parametric variables). Normality was explored using the Shapiro–Wilk test. The qualitative variables were described by their frequency distribution. Mann–Whitney U (2 variables, non-parametric) or Kruskal–Wallis (3 or more variables, non parametric) tests were used for comparison of quantitative variables. Pearson's chi-squared test (parametric) or Fisher's exact test (non-parametric) were used in comparison of qualitative variables, and the linear tendency test for those with more than 2 categories and ordinal sequence. Logistic regression was used in the analysis.
Excel 2010 and Stata© version 13.1 were used for processing the data and the statistical analysis.
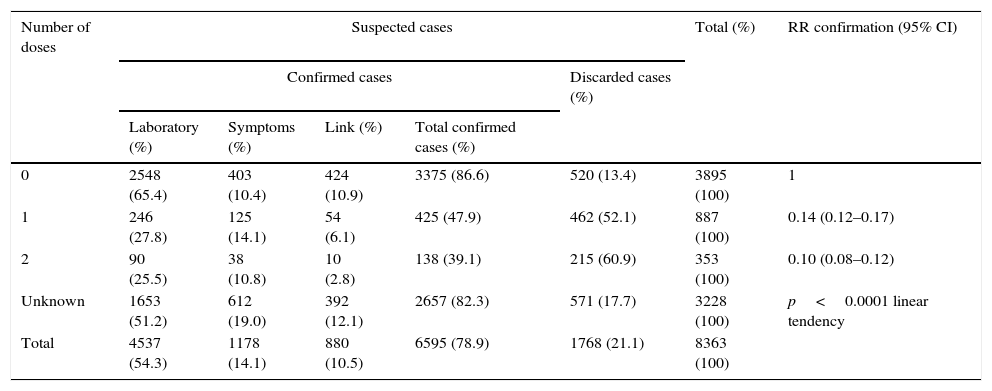
ResultsBetween 2003 and 2014, 8363 suspected cases of measles were notified. Seventy-eight point nine percent of the suspected cases were confirmed and 21.1% were discarded. In 5135 cases (61.40%) the vaccination history was known. Of these 5135 cases, 3.50% (138/3938) of those that were confirmed and 17.9% (215/1.197) of those discarded had received 2 doses of the vaccine (Table 1).
Classification of measles cases according to the number of vaccine doses received, Spain 2003–2014.
| Number of doses | Suspected cases | Total (%) | RR confirmation (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Confirmed cases | Discarded cases (%) | ||||||
| Laboratory (%) | Symptoms (%) | Link (%) | Total confirmed cases (%) | ||||
| 0 | 2548 (65.4) | 403 (10.4) | 424 (10.9) | 3375 (86.6) | 520 (13.4) | 3895 (100) | 1 |
| 1 | 246 (27.8) | 125 (14.1) | 54 (6.1) | 425 (47.9) | 462 (52.1) | 887 (100) | 0.14 (0.12–0.17) |
| 2 | 90 (25.5) | 38 (10.8) | 10 (2.8) | 138 (39.1) | 215 (60.9) | 353 (100) | 0.10 (0.08–0.12) |
| Unknown | 1653 (51.2) | 612 (19.0) | 392 (12.1) | 2657 (82.3) | 571 (17.7) | 3228 (100) | p<0.0001 linear tendency |
| Total | 4537 (54.3) | 1178 (14.1) | 880 (10.5) | 6595 (78.9) | 1768 (21.1) | 8363 (100) | |
The mean incidence of measles in Spain during this period was 1.23 (95% CI: 1.13–1.33) confirmed cases per 100,000 inhabitants and year. This incidence varied in the different age groups, there being 7.91 (6.85–9.13) cases per 100,000 inhabitants and per year in those younger than 5 years, 1.8 (1.51–2.15) cases per 100,000 inhabitants and per year aged between 5 and 19 years, and 0.32 (0.26–0.38) cases per 100,000 inhabitants and per year aged 20 or older. The proportion of confirmed suspected cases of measles reduced as the number of vaccine doses received increased. Taking the unvaccinated people as the benchmark (RR1), the RR of confirmation in people vaccinated with one dose was 0.14 (95% CI: 0.12–0.17), and in people vaccinated with 2 doses, 0.10 (95% CI: 0.08–0.12) (significant linear tendency test, p<0.001) (Table 1).
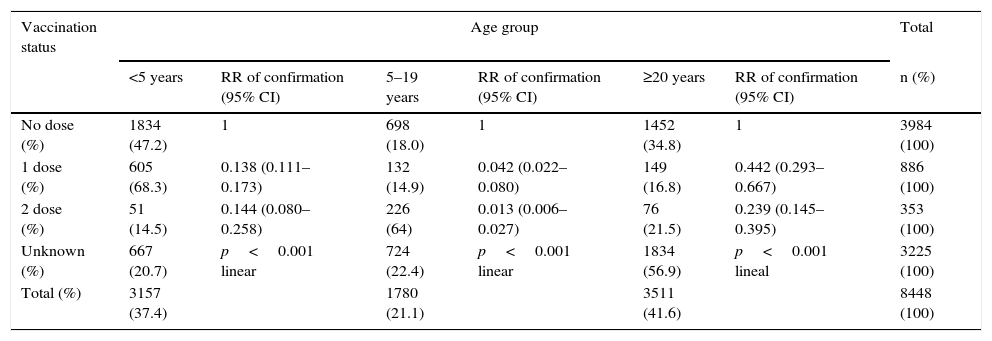
There were more suspected cases of measles in unvaccinated people among the under 5s (47.2%) and in adults aged 20 or older (34.8%). In those vaccinated with one dose, there were more suspected cases in the under 5s (68.3%), and in those vaccinated with 2 doses, there were more among those aged between 5 and 19 years (64.0%). The RR of confirmation of suspected cases showed a significant decreasing global linear tendency according to the number of doses (p<0.001). Likewise, this RR of confirmation was different in the different age groups. The risk of confirmation of a suspected case of measles, with the same vaccination status, was greater in the group aged 20 and older, followed by that aged 5 and under, and finally, in the group aged from 5 to 19 years (Table 2).
Suspected cases of measles with RR of confirmation per age group and vaccination status, Spain 2003–2014.
| Vaccination status | Age group | Total | |||||
|---|---|---|---|---|---|---|---|
| <5 years | RR of confirmation (95% CI) | 5–19 years | RR of confirmation (95% CI) | ≥20 years | RR of confirmation (95% CI) | n (%) | |
| No dose (%) | 1834 (47.2) | 1 | 698 (18.0) | 1 | 1452 (34.8) | 1 | 3984 (100) |
| 1 dose (%) | 605 (68.3) | 0.138 (0.111–0.173) | 132 (14.9) | 0.042 (0.022–0.080) | 149 (16.8) | 0.442 (0.293–0.667) | 886 (100) |
| 2 dose (%) | 51 (14.5) | 0.144 (0.080–0.258) | 226 (64) | 0.013 (0.006–0.027) | 76 (21.5) | 0.239 (0.145–0.395) | 353 (100) |
| Unknown (%) | 667 (20.7) | p<0.001 linear | 724 (22.4) | p<0.001 linear | 1834 (56.9) | p<0.001 lineal | 3225 (100) |
| Total (%) | 3157 (37.4) | 1780 (21.1) | 3511 (41.6) | 8448 (100) | |||
In the cases confirmed in vaccinated people, the median time between the last vaccine dose and the onset of the rash was 4.0 years (interquartile range [IR] 0–10.9 years) in those vaccinated with 2 doses, and 1.0 year (IR 0.1–7.1 years) in those vaccinated with one dose (Mann–Whitney U test p=0.075).
Twenty point seven percent of confirmed cases required hospitalisation. The proportion of hospitalised people was different according to the vaccination status: 23.4% in unvaccinated people, 14.7% in one-dose vaccinated people, and 10.2% in 2-dose vaccinated people. Taking the unvaccinated people as the benchmark (RR 1), the one-dose vaccinated people presented a RR of hospitalisation of 0.43 (95% CI: 0.34–0.54), and those vaccinated with 2 doses, a RR of hospitalisation of 0.31 (95% CI: 0.20–0.45) (significant linear tendency test, p<0.001).
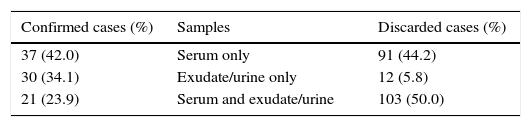
Samples had been taken from 206 (95.8%) of the 215 discarded cases of people vaccinated with 2 doses. Of these, serum and exudate and/or urine were collected from only 103 (50.0%), as recommended in the protocol. One hundred and eighty-eight (87.4%) cases were discarded through negative IgM (technique of choice). The epidemiological situation of the remaining 18 (9 with negative PCR, the others with an epidemiological link with one confirmed case of another exanthematous disease) was assessed. Although PCR alone is not sufficient to discard a case, these 9 cases were assessed individually and were eventually discarded (Table 3).
Laboratory samples and tests in confirmed and discarded cases of measles in 2-dose vaccinated people.
| Confirmed cases (%) | Samples | Discarded cases (%) |
|---|---|---|
| 37 (42.0) | Serum only | 91 (44.2) |
| 30 (34.1) | Exudate/urine only | 12 (5.8) |
| 21 (23.9) | Serum and exudate/urine | 103 (50.0) |
| Confirmed cases n (%) | Laboratory tests | No. discarded cases n (%) | |
|---|---|---|---|
| 35 (42.2) | Only IgM+ | Only IgM− | 88 (44.6) |
| 36 (43.4) | Only PCR+ | Only PCR− | 9 (5.6) |
| 12 (14.4) | IgM+ and PCR+ | IgM− and PCR− | 100 (50.8) |
In order to evaluate the timeliness of taking a sample, the “number of days between onset of rash and taking the first serum sample” variable was examined. In 2-dose vaccinated people, the median of this variable was 3 days (IR 1–5 days). In other words, 50% of samples were taken early. Of the 215 cases discarded of the 2-dose vaccinated people, in 92 cases (42.8%) the negative IgM was obtained from samples that were taken promptly. There was no other laboratory test result (PCR was not performed) to support discarding 36 (16.7% of the total discarded cases) of these 92 cases.
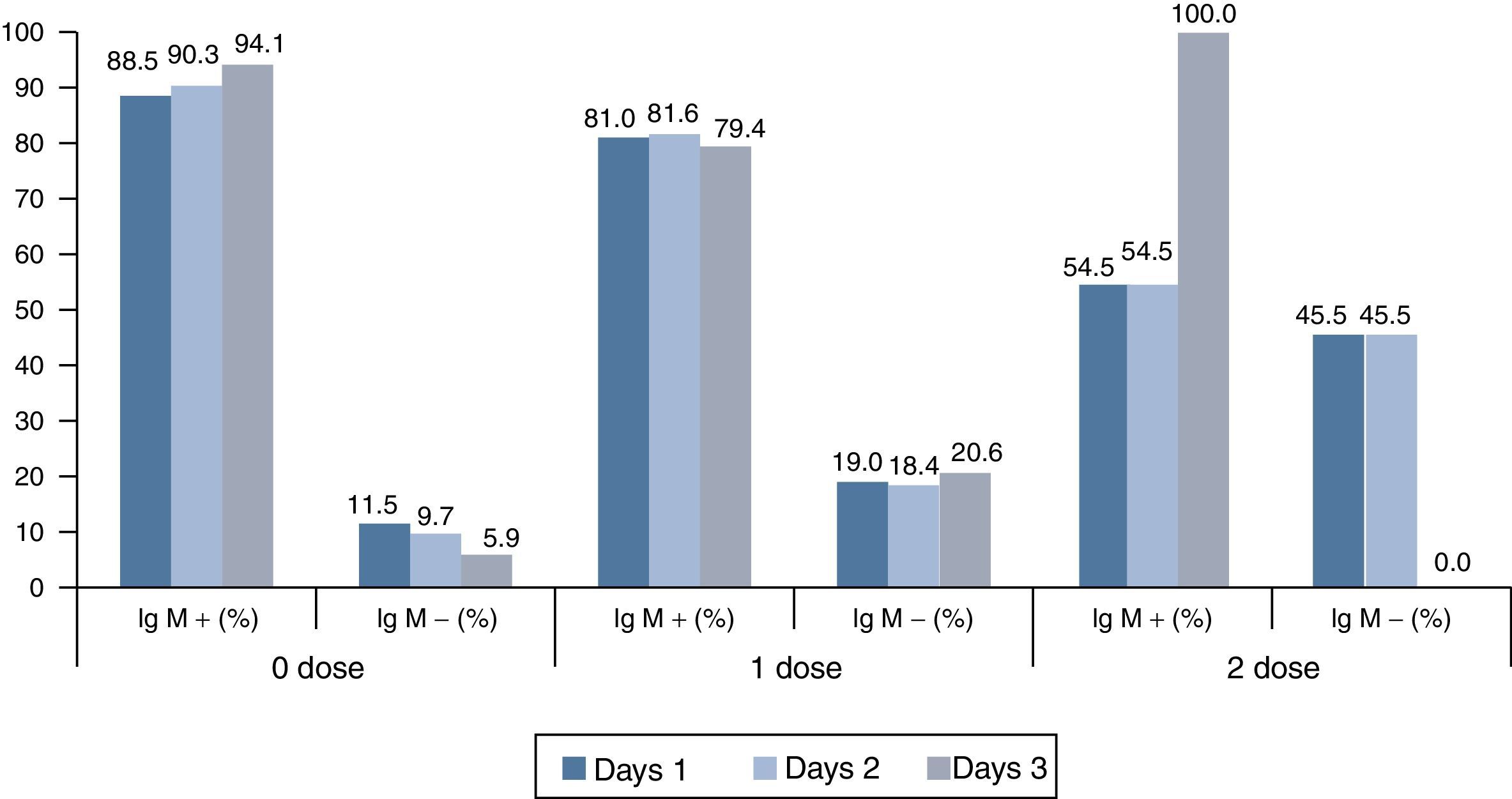
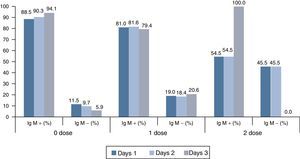
Finally, we examined the likelihood of a negative IgM in a promptly taken serum sample representing a false negative. To that end, we studied the cases that, after a first IgM negative result in an early sample, were confirmed by the laboratory after a second serum sample (with positive IgM and/or positive PCR), stratifying them according to the number of vaccine doses received (0, 1 or 2 doses). It was observed in these laboratory-confirmed cases that as the number of vaccine doses received increased, so too did the proportion of cases with early negative IgM results in serum (Fig. 1).
DiscussionAs highlighted by other studies (Van der Hoek et al. and Kutty et al.), a diagnosis of measles in vaccinated people is more complex, because the symptoms are milder, the immune response to IgM can be absent or shortened, and due to the poor replication of the virus, molecular detection by PCR is limited.13,19 All of this can lead to measles being under-detected in vaccinated people, the incorrect classification of cases (Hyde et al.),20 the consequent interruption of research into cases and outbreaks, and the pertinent control measures not being applied. Cases of measles in vaccinated people are less contagious (Rota et al.)21 and rarely cause outbreaks, although they can (Rosen et al.).22
The fact that in our study the proportion of hospitalised cases is inversely proportional to the number of vaccine doses, with significant linear tendency, is consistent with what has been noted previously about the less serious nature of measles when vaccination status improves (MMWR 198011, Damien et al.12).
With regard to the phenomenon of waning, Mercader et al. indicated a progressive descent in the levels of antibodies to measles over the passage of time since vaccination.15 In line with this waning immunity that the group of LeBaron et al.23 also highlight, in our study we observed that the risk of confirmation of suspected measles in vaccinated individuals (with 1 or 2 doses) was considerably higher in adults aged 20 and over than in children and young people between the ages of 5 and 19. However, when interpreting this result we should consider that febrile rashes caused by other infectious agents are more common at these ages. This could be an explanation, therefore, in part for the fewer confirmed suspected cases of measles in the 5–19 year age group.
In populations with high vaccine coverage like ours (above 95% for the first dose since 1999, and above 90% for the second dose since 2006), there will be increasingly more suspected cases of measles in vaccinated people. The most probable scenario at the end of the elimination phase will be that most notified suspected cases that are investigated will be discarded. In our study, we found that the risk of a suspected case of measles being discarded after investigation was greater in vaccinated individuals than in unvaccinated individuals, and also showed a significant linear tendency inversely proportional to the number of doses of vaccine received (p<0.001).
The great difficulty in confirming or discarding cases of measles in 2-dose vaccinated people, especially in the elimination phase, motivated us to make a detailed analysis of the adaptation to the current investigation protocol in the laboratory (clinical samples and tests performed) of the suspected cases in this group, paying particular attention to discarded cases. In a suspected case of measles it is essential to take the 3 clinical samples promptly (serum/exudate/urine).
In our study, in 50% of the cases studied of 2-dose vaccinated people, the first serum sample had been taken promptly. In 16.7% of the discarded cases an early negative IgM was obtained, and PCR was not performed; these could be false negatives. A negative IgM result in early samples, as indicated by Atkinson et al.24 or Hyde et al.,20 does not mean a suspected case can be discarded. For this reason, it is particularly important to follow the protocol for taking samples and perform laboratory tests on 2-dose vaccinated people, repeating serum samples early for a second IgM test and always performing the PCR test on exudate and urine as well. Likewise, the inclusion of additional diagnostic tests in the measles surveillance protocol could also be assessed, such as the quantitative IgG test or the IgG avidity test, since these tests show differential characteristics in previously immunised people, as mentioned by Mercader et al.,15 or Hickman et al.16
In conclusion, after analysing the cases of measles notified to the Spanish National Plan for the Elimination of Measles and Rubella, in the past 12 years we have found that there are differences according to an individual's previous vaccination status in terms of developing an immune response and the clinical presentation of the disease. Cases of measles in vaccinated people, particularly those who have received 2 vaccine doses, are associated with less hospitalisation and are milder. Likewise, fewer suspected cases of measles are confirmed in vaccinated people. Finally, diagnosis is more difficult in vaccinated people, because IgM takes longer to result positive and false negatives are more frequent when samples are taken early. Therefore, we consider it particularly appropriate to follow the current surveillance correctly for these people, ensuring that samples are taken promptly and always performing a PCR test, especially in this final phase of the measles elimination process.
FundingNo funding has been received for this study.
Conflicts of interestThe authors have no conflicts of interests to declare.
We would like to thank the measles epidemiological surveillance and laboratory managers of the Spanish National Epidemiological Surveillance Network.
And Andrés Aragón, Head of the Area Epidemiological Section of the Community of Madrid, for his comments and suggestions regarding the content and drafting of the article.
Please cite this article as: Risco-Risco C, Masa-Calles J, López-Perea N, Echevarría JE, Rodríguez-Caravaca G. Epidemiología del sarampión en personas vacunadas, España 2003–2014. Enferm Infecc Microbiol Clin. 2017;35:569–573.