We read with interest the article by Berzosa Sánchez et al. "Respiratory infection due to Chlamydia trachomatis, four cases report",1 published in the November issue of your journal. As the authors noted, C. trachomatis pneumonia is one of the most common causes of atypical pneumonia in the first few months of life. Accurate diagnosis is essential, given that, in some cases, symptoms of respiratory failure significant enough to require admission to intensive care (IC) can develop.2,3 However, serious C. trachomatis infection has not been studied much and is a poorly recognised disease in paediatrics.
In order to assess the severity of this disease, we retrospectively reviewed the medical records of infants diagnosed with C. trachomatis pneumonia at our centre in the last 10 years (2010–2019).
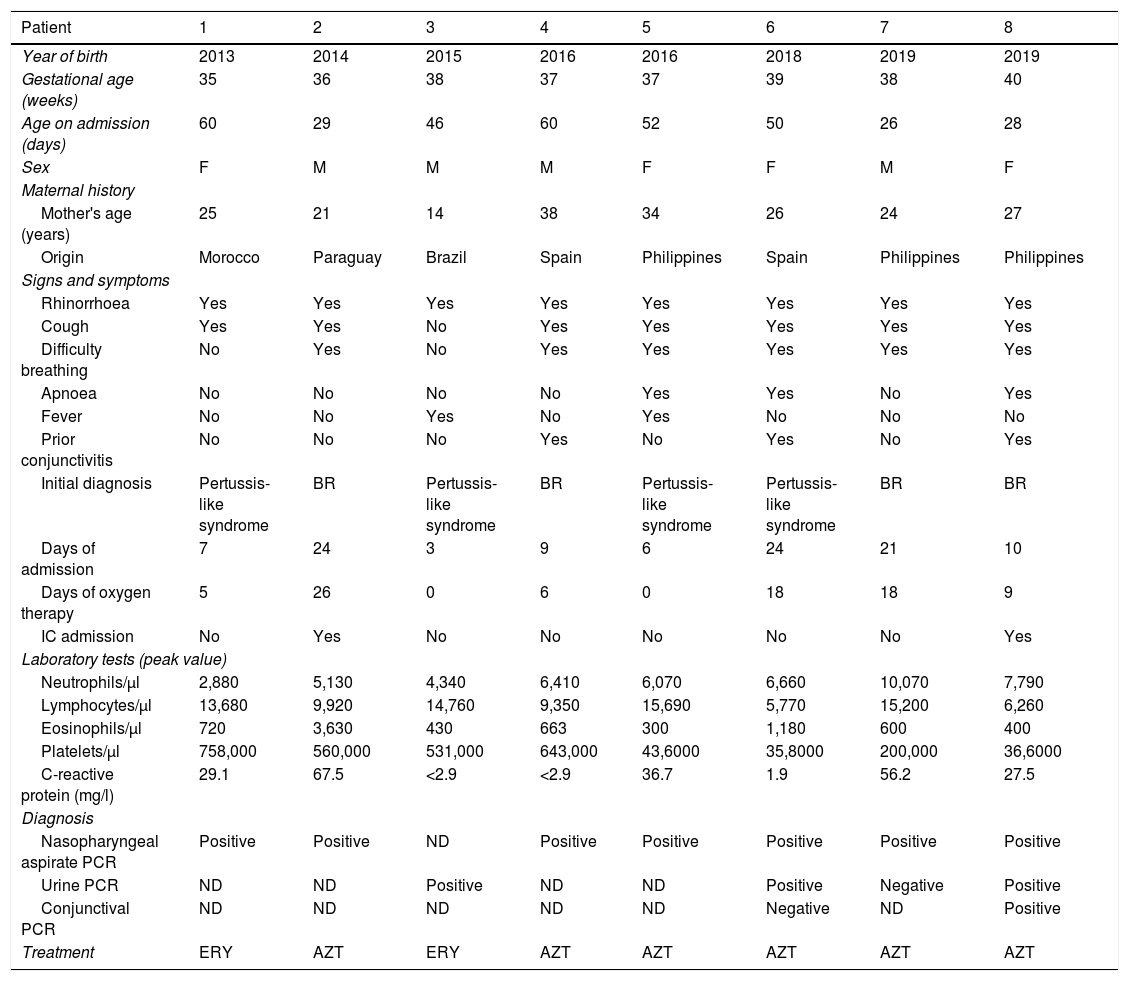
We diagnosed a total of eight infants. Their main characteristics are described in Table 1. All were full-term newborns, except for two late preterm infants (35 and 36 weeks). Median age at diagnosis was 48 days (IQR: 28-58), and all cases began between the third and sixth week of life. The mean age of the mothers was 25.5 years (IQR: 22-32), and six of them (75%) were immigrants.
Epidemiological characteristics, clinical signs, supplementary tests and treatment.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| Year of birth | 2013 | 2014 | 2015 | 2016 | 2016 | 2018 | 2019 | 2019 |
| Gestational age (weeks) | 35 | 36 | 38 | 37 | 37 | 39 | 38 | 40 |
| Age on admission (days) | 60 | 29 | 46 | 60 | 52 | 50 | 26 | 28 |
| Sex | F | M | M | M | F | F | M | F |
| Maternal history | ||||||||
| Mother's age (years) | 25 | 21 | 14 | 38 | 34 | 26 | 24 | 27 |
| Origin | Morocco | Paraguay | Brazil | Spain | Philippines | Spain | Philippines | Philippines |
| Signs and symptoms | ||||||||
| Rhinorrhoea | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Cough | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Difficulty breathing | No | Yes | No | Yes | Yes | Yes | Yes | Yes |
| Apnoea | No | No | No | No | Yes | Yes | No | Yes |
| Fever | No | No | Yes | No | Yes | No | No | No |
| Prior conjunctivitis | No | No | No | Yes | No | Yes | No | Yes |
| Initial diagnosis | Pertussis-like syndrome | BR | Pertussis-like syndrome | BR | Pertussis-like syndrome | Pertussis-like syndrome | BR | BR |
| Days of admission | 7 | 24 | 3 | 9 | 6 | 24 | 21 | 10 |
| Days of oxygen therapy | 5 | 26 | 0 | 6 | 0 | 18 | 18 | 9 |
| IC admission | No | Yes | No | No | No | No | No | Yes |
| Laboratory tests (peak value) | ||||||||
| Neutrophils/μl | 2,880 | 5,130 | 4,340 | 6,410 | 6,070 | 6,660 | 10,070 | 7,790 |
| Lymphocytes/μl | 13,680 | 9,920 | 14,760 | 9,350 | 15,690 | 5,770 | 15,200 | 6,260 |
| Eosinophils/μl | 720 | 3,630 | 430 | 663 | 300 | 1,180 | 600 | 400 |
| Platelets/μl | 758,000 | 560,000 | 531,000 | 643,000 | 43,6000 | 35,8000 | 200,000 | 36,6000 |
| C-reactive protein (mg/l) | 29.1 | 67.5 | <2.9 | <2.9 | 36.7 | 1.9 | 56.2 | 27.5 |
| Diagnosis | ||||||||
| Nasopharyngeal aspirate PCR | Positive | Positive | ND | Positive | Positive | Positive | Positive | Positive |
| Urine PCR | ND | ND | Positive | ND | ND | Positive | Negative | Positive |
| Conjunctival PCR | ND | ND | ND | ND | ND | Negative | ND | Positive |
| Treatment | ERY | AZT | ERY | AZT | AZT | AZT | AZT | AZT |
AZT: azithromycin; BR: bronchiolitis; IC: intensive care; ERY: erythromycin; F: female; M: male; ND: not done; PCR: polymerase chain reaction.
All infants were brought in due to respiratory symptoms; only two had fever. Three had a history of conjunctivitis in the second week of life, although C. trachomatis infection was not suspected, and therefore they did not receive suitable treatment. In all cases, a chest X-ray was pathological, with hyperinflation and interstitial infiltrates. Notably, there were high percentages of eosinophilia (5/8) and hypergammaglobulinaemia (4/4).
All patients were admitted, and the median duration of hospitalisation was 9.5 days (IQR: 6-23). Six patients required oxygen therapy for a mean of 7.5 days (IQR: 1-18). High-flow systems were used in three patients. Two infants required IC admission for respiratory failure: one needed non-invasive ventilation and the other needed invasive mechanical ventilation for two days.
The microbiological diagnosis was made by polymerase chain reaction (BD max™ multiplex PCR) in nasopharyngeal aspirate (positive in seven cases) and in urine (positive in three of the four cases for which it was ordered). In two cases with associated conjunctivitis, conjunctival PCR was performed, and was positive in one case.
All patients received treatment with an oral macrolide, following a favourable course. The mothers and their partners were referred to the gynaecology clinic for evaluation.
In developed countries, C. trachomatis infection is the most prevalent sexually transmitted disease.4 It is an underdiagnosed disease in pregnant women because it usually follows an asymptomatic course,1,2 which can lead to a delay in diagnosis for the child and a need for hospital admission.
Perinatal infection causes colonisation of the pharynx, rectum and genital tract of newborns. In 30%–50% of colonised neonates, it causes conjunctivitis in the first two weeks of life.5 It is important to be attentive to this first sign, which is usually self-limiting, to make a correct diagnosis by PCR in conjunctival discharge.
Without suitable treatment, these patients can develop a nasopharyngeal infection, which in 30% of cases can progress to pneumonia.6 This usually presents with prolonged hypoxaemia and, in some cases, a need for respiratory support and IC admission.3,7,8 In our series, two patients were transferred to IC for severe respiratory failure. In 1985, Attenburrow and Barker reported five cases of severe neonatal pneumonia due to C. trachomatis in premature infants (25–32 weeks); all required mechanical ventilation, and one died.8
We agree with Piñeiro et al.9 on the need to implement screening programmes for C. trachomatis in pregnant women 15–25 years of age and in women with risk factors for infection. In our series, 75% of the mothers were under 30 years of age and many were immigrants from areas with a high prevalence of the disease. In areas where screening is not implemented, it should be suspected in infants under 2 months of age with slowly progressing bronchiolitis or cough with pertussis-like features, a history of previous conjunctivitis, eosinophilia and hypergammaglobulinaemia. Early diagnosis and treatment in the infant can prevent hospital admission and associated complications.
FundingThis work received no specific funding from public, private or non-profit organisations.
Please cite this article as: Dorado-Criado M, Fabra-Garrido C, Buitrago Gil C, Baquero-Artigao F. Neumonitis por Chlamydia trachomatis: una enfermedad infradiagnosticada y potencialmente grave. Enferm Infecc Microbiol Clin. 2021;39:265–266.