The aim of the intervention was to describe the feasibility and cost-effectiveness of offering HIV testing in outreach interventions and subsequent consultation of the results through a secure web page.
MethodsThe HIV test was offered “in situ” to men who have sex with men (MSM), migrant sex workers and trans women recruited in places of leisure and sex. Four collaborating NGOs recruited the participants and assisted them to register on the study website (www.swab2know.eu) through a tablet or the smartphone of the same participant. The samples were sent to the reference laboratory and the results were published on the website.
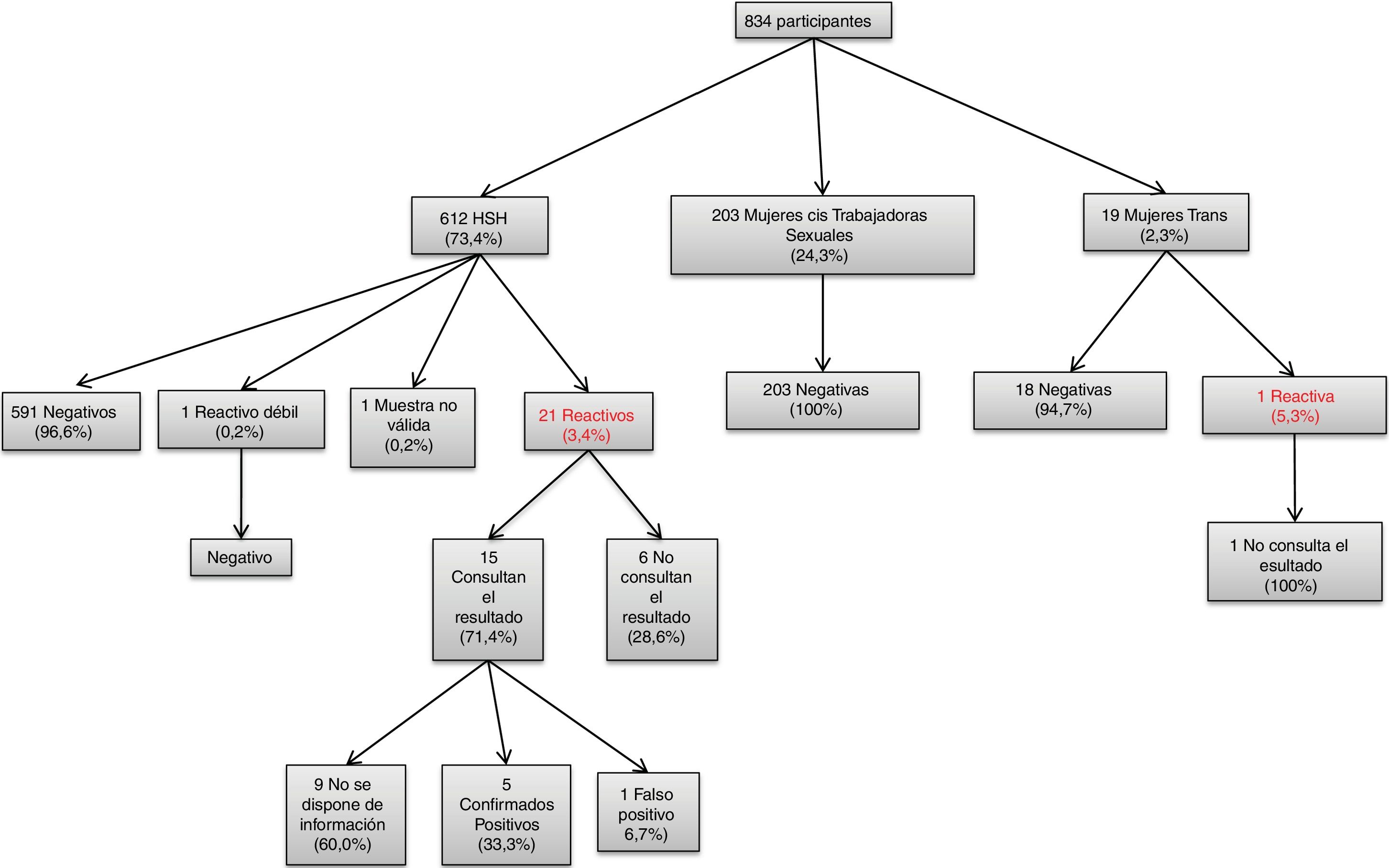
Results834 participants (612 MSMs, 203 women sex workers and 19 trans women) were recruited. In total 22 reagent results (2.6%) were detected: 21 among MSMs (3.4%) and 1 in a trans women (5.3%). While 82.6% of MSMs consulted their outcome, only 39.9% and 26.3% of women sex workers and trans women respectively consulted their outcome.
ConclusionsProviding self-sampling in outreach activities, dispatch and analysis in a reference laboratory as well as online communication of test results is feasible. A high proportion of participants with a HIV reactive result were detected among MSMs and trans women.
El objetivo de la intervención fue describir la viabilidad y la rentabilidad de la oferta de la prueba del VIH en intervenciones de acercamiento (outreach) y posterior consulta de los resultados a través de una página web segura.
MétodosSe ofreció la auto-toma de muestra “in situ” para detección del VIH en fluido oral a hombres que tienen sexo con hombres (HSH), trabajadores/as sexuales migrantes y mujeres trans reclutados en lugares de ocio y sexo. Cuatro ONGs colaboradoras reclutaron a las personas participantes y les asistieron para que se dieran de alta en la web del estudio (www.swab2know.eu) a través de una tablet o el smartphone del mismo participante. Las muestras se enviaron al laboratorio de referencia y los resultados se publicaron en la página web.
ResultadosSe reclutaron 834 participantes (612 HSH, 203 mujeres trabajadoras sexuales y 19 mujeres trans). En total se detectaron 22 resultados reactivos (2,6%): 21 entre los HSH (3,4%) y 1 en una mujer trans (5,3%). Mientras que el 82,6% de los HSH consultó su resultado, solamente el 39,9% y el 26,3% de las mujeres trabajadoras sexuales y las mujeres trans respectivamente consultaron su resultado.
ConclusionesOfrecer la auto toma de muestra en actividades de acercamiento, el envío y análisis en un laboratorio de referencia y la posterior consulta de los resultados online es viable. Se detectó un elevado porcentaje de usuarios con un resultado reactivo para el VIH entre los HSH y las mujeres trans.
In 2017, 578 new HIV diagnoses were reported in Catalonia. This represents a ratio of 8.1 cases per 100,000 inhabitants,1 higher than the average in the European Union (6.4 cases per 100,000 inhabitants).2 Half of the diagnoses reported were in men who have sex with men (MSM) (54%), 47% were in people born outside of Spain and 44% had a late diagnosis (CD4 count <350 cells/μl). Even though the percentage of late diagnosis among MSM is lower (39%), they account for 48% of all late diagnoses1. A delay in diagnosis is associated with higher rates of morbidity and mortality, higher economic costs and a longer period of transmissibility and, therefore, a higher contribution to incidence.3–6
In Spain and other countries where the HIV epidemic is concentrated in the MSM population, it has been reported that the sustained incidence of HIV within this group could be explained by a growing percentage of recent undiagnosed HIV infections in MSM (period of high transmissibility), coupled with an increase in risky behaviours, such as unprotected anal sex and a larger number of sexual partners, particularly among HIV+MSM who risk transmitting the disease.7,8 Reducing the number of undiagnosed infections and treating these individuals early is a priority that would have an impact on the incidence of HIV, as different models have demonstrated.9,10 Both national and international guidelines recommend that MSM undergo annual testing and at-risk MSM, specifically those with a medical history of sexually transmitted infections and those taking anti-HIV pre-exposure prophylaxis (PrEP), be tested every 3 months.11–13 With the objective of increasing access to and frequency of testing in this key population, different strategies for screening outside of the healthcare setting have been developed. Interventions at both gay entertainment venues and community centres offering anonymous screening14–16 have demonstrated their effectiveness in providing easy access to HIV testing in this population. However, despite these interventions, it has been reported that 12.3% of MSM in Spain have never had an HIV test and 45.7% have not been tested in the last 12 months.17
Sex workers, for their part, constitute a population of women, men and trans women who are particularly vulnerable to HIV. In Spain, the prevalence of HIV in female sex workers has remained constant over the years (approximately 2%).18 Among male sex workers, increases in proportions of HIV seropositive cases by 1.1% in 2010 and 13.6% in 2015 have been reported.19 Among sex workers who are trans women, a prevalence of HIV of 24.5%20 has been reported. It should be noted that a high percentage of sex workers in Spain are immigrants. Aside from the stigma and marginalisation linked to sex work, sex workers constitute a mixed group whose access to social and healthcare services is limited by cultural and language barriers, stigma and discrimination, and lack of awareness of the system, among other reasons.21
Finally, the World Health Organization has deemed transsexual women a highly vulnerable group with specific health needs requiring a different and separate status in the global response to HIV.22 The prevalence of HIV in trans women tested for the first time at 20 community screening centres in Spain's major cities was 24.5%23
Therefore, innovative approaches must be developed that promote better access to HIV testing and reach at-risk, difficult-to-access populations for whom current outreach strategies have not been successful. These innovative approaches include self-testing, for which good results and widespread acceptance among MSM have been reported.24,25 In Belgium, the Swab2know project25 demonstrated the acceptability and viability among MSM and sub-Saharan migrants of the use of oral fluid samples collected during outreach activities or through online orders for self-testing kits. Once the samples had been analysed, the results were made available to the corresponding individuals online. The Swab2know project was extended to 5 more European countries (Denmark, Slovenia, Spain, Portugal and Romania) as part of the Euro HIV EDAT project (www.eurohivedat.eu). This article presents the results of the Swab2know project in Spain, the objectives of which were to report the viability and yield of a pilot intervention aimed at MSM, migrant sex workers and trans women in Spain, consisting of offering self-testing for HIV at outreach activities and subsequent making the results available to the corresponding individuals online.
MethodsA new website has been developed in Spanish (www.swab2know.eu) based on the Swab2know project.25 The purpose of the website was to offer information about HIV and messages about prevention and to enable individuals to check the results of the tests from the outreach activities.
The following target populations are defined: MSM, trans women and migrant sex workers (cisgender women, trans women and cisgender men, all born outside Spain). MSM and some trans women were recruited by the association Stop Sida [Stop AIDS] in nightclubs, bars, sex shops, sex parlours, cruising areas, themed parties and pride festivals in Barcelona and Sitges.26 Sex workers were recruited by Ámbit Prevenció [Prevention Area], Associació Antisida Lleida [Lleida Anti-AIDS Association] and Actuavallès [Act Vallès] on the street, roadside, clubs and flats where sex work takes place in Barcelona, Castelldefels, Lleida and various municipalities in Vallès Occidental. The inclusion criteria were being an adult, belonging to one of the established target populations, providing an e-mail address (if they lacked an e-mail address, health workers provided one) and signing the informed consent form (on paper). The study period was March 2016 to June 2017.
Health workers provided the target population with information about the study, invited them to take part, obtained informed consent and helped them to register on the study website using a tablet or the participant's own smartphone. Each account was unique and linked to an e-mail address. Next, the participants completed a sociodemographic and behavioural questionnaire on the website. They were also given the chance to complete the questionnaire on paper where there was no Wi-Fi coverage. Participants took their own oral fluid samples using the Oracol Saliva Collection System (Malvern Medical Developments Limited, Worcester, United Kingdom) with help from the health workers. They were then given a card with the identifier for the sample associated with their account, informed consent and questionnaire. The samples were stored at room temperature and sent to the reference laboratory (Microbiology Department, Hospital Germans Trias i Pujol [Germans Trias i Pujol Hospital], Badalona, Spain).
The samples were analysed to detect HIV antibodies using the previously validated Genscreen HIV-1/2 Version 2 (Bio-Rad, Marnes-la-Coquette, France).27 The results were categorised as negative (which ruled out HIV infection taking into account a window period of 3 months), reactive (indicating potential HIV infection requiring confirmation by a blood test), weakly reactive (indicating a likely false positive result requiring confirmation by a blood test) and invalid sample (not analysed due to poor quality). Once the results had been obtained, they were posted to the website by the coordinating site and participants received an automated e-mail informing them that their result was available. To check it, they had to log into the website with their username and password and then enter the sample code. The website included post-testing advice and information about where participants with a reactive result could go for a confirmation test. Reminders were sent by e-mail and text message to participants who did not check their result. Two reminders were sent to those with a negative result (2 and 4 weeks after their results were made available) and four reminders were sent to those with a reactive result (one reminder every week for 4 consecutive weeks).
The study was approved by the Hospital Germans Trias i Pujol Independent Ethics Committee. The website was protected in accordance with European legislation and standards and requirements for data protection and privacy through the Secure Sockets Layer protocol, and it had a security certificate issued by Belnet (the Belgian federal government organisation that provides Internet connectivity and services to Belgian universities, research centres and governmental departments in Belgium).
MSM, cisgender female sex workers and trans women were analysed separately. Statistical analysis was performed using SPSS version 19 (IBM, Amonk, United States). Descriptive analyses were performed. Chi-squared tests were used for categorical variables and the Mann–Whitney U test for independent samples was used for the continuous variables as the data lacked a normal distribution. A level of significance of 5% was applied. Descriptive statistics for all oral fluid samples collected are presented.
ResultsDuring the study period, 834 participants were recruited; 612 were MSM (73.4%), 203 were cisgender female sex workers (24.3%) and 19 were transexual women (2.3%). MSM, cisgender female sex workers and trans women were analysed separately. Of the 19 trans women included in the study, 17 were recruited in places where sex work took place and the remaining 2 were recruited in gay entertainment venues. The latter were not considered to be sex workers.
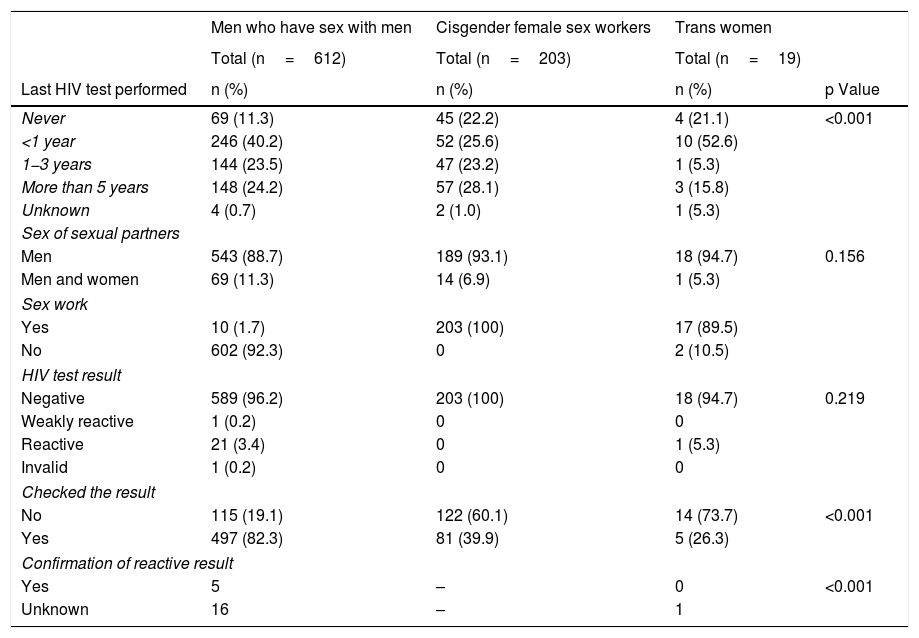
Table 1 shows the characteristics of the people recruited (MSM, cis female sex workers and trans women). The median age of the MSM was 34; 40.2% of them had undergone HIV testing less than a year ago, and their median number of sexual partners in the last 3 months was 4 (IQR: 2−10). The cisgender female sex workers recruited had a median age of 31; 25.6% had undergone HIV testing in the last year, and their median number of sexual partners in the last 3 months was 100 (IQR: 50−200) (Table 1). Over half (52.6%) of the trans women who participated in the study had undergone HIV testing within the last year, and their median number of sexual partners in the last 3 months was 50 (IQR: 15-120) (Table 1). The percentage of those who checked their results varied among the participants; while 82.6% of the MSM checked their result (Table 1), only 39.9% and 26.3% of the cisgender female sex workers and trans women, respectively, checked their result. Significant differences were seen between the 3 populations in terms of time since last HIV test, whether they checked or did not check their result and whether they confirmed their result.
Characteristics of the study participants. N: 834, Catalonia (Spain).
| Men who have sex with men | Cisgender female sex workers | Trans women | ||
|---|---|---|---|---|
| Total (n=612) | Total (n=203) | Total (n=19) | ||
| Last HIV test performed | n (%) | n (%) | n (%) | p Value |
| Never | 69 (11.3) | 45 (22.2) | 4 (21.1) | <0.001 |
| <1 year | 246 (40.2) | 52 (25.6) | 10 (52.6) | |
| 1−3 years | 144 (23.5) | 47 (23.2) | 1 (5.3) | |
| More than 5 years | 148 (24.2) | 57 (28.1) | 3 (15.8) | |
| Unknown | 4 (0.7) | 2 (1.0) | 1 (5.3) | |
| Sex of sexual partners | ||||
| Men | 543 (88.7) | 189 (93.1) | 18 (94.7) | 0.156 |
| Men and women | 69 (11.3) | 14 (6.9) | 1 (5.3) | |
| Sex work | ||||
| Yes | 10 (1.7) | 203 (100) | 17 (89.5) | |
| No | 602 (92.3) | 0 | 2 (10.5) | |
| HIV test result | ||||
| Negative | 589 (96.2) | 203 (100) | 18 (94.7) | 0.219 |
| Weakly reactive | 1 (0.2) | 0 | 0 | |
| Reactive | 21 (3.4) | 0 | 1 (5.3) | |
| Invalid | 1 (0.2) | 0 | 0 | |
| Checked the result | ||||
| No | 115 (19.1) | 122 (60.1) | 14 (73.7) | <0.001 |
| Yes | 497 (82.3) | 81 (39.9) | 5 (26.3) | |
| Confirmation of reactive result | ||||
| Yes | 5 | – | 0 | <0.001 |
| Unknown | 16 | – | 1 | |
| Median (IQR) | Median (IQR) | Median (IQR) | ||
|---|---|---|---|---|
| Age | 34 years (27−43) | 31 years (26−37) | 31 years (22−37) | 0.488 |
| Number of sexual partners in the last 3 months | 4 (2−10) | 100 (50−200) | 50 (15−120) | 0.489 |
CI: confidence interval; IQR: interquartile range; HIV: human immunodeficiency virus.
Fig. 1 shows the study diagram. There were 22 reactive tests for HIV (2.6%), one weakly reactive test that was confirmed to be negative and one invalid sample. Of the 22 reactive tests, 21 corresponded to members of the MSM population (3.4%); none of them were sex workers. One reactive test was detected among the trans women (5.3%), who were not considered to be sex workers, and no reactive tests were detected among the cisgender female sex workers. Of the 21 MSM participants with a reactive test result, 6 (28.6%) did not check their result and 15 (71.4%) did. The trans woman with a reactive result did not check her result. Of the participants who checked their result, information was only available for 6 participants who underwent confirmation testing (40.0%); of these, 5 were confirmed to be positive (23.8%) and one was a false positive. No information was available for the remaining 9 participants (60.0%).
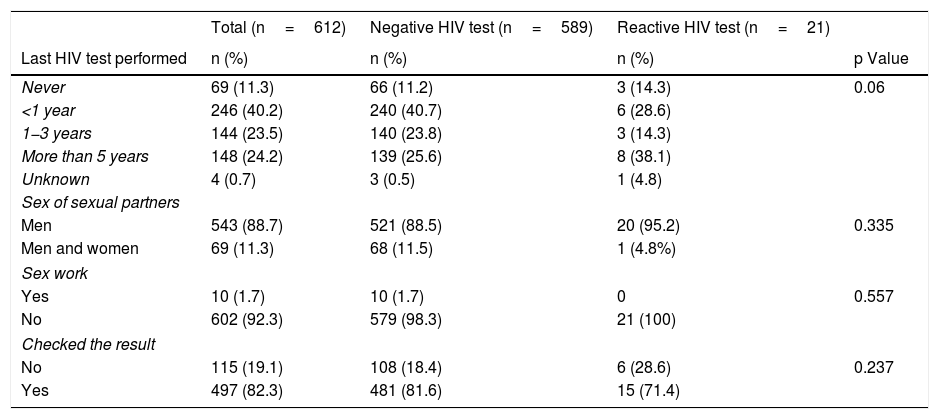
No statistically significant differences were seen between the MSM with a reactive result and those with a negative result in terms of age, previous HIV testing, sex worker status, having sex exclusively with men or with men and women, or number of sexual partners in the last 3 months (Table 2). The trans woman with a reactive result was 21 years old and her last HIV test was over 5 years ago. She had sex exclusively with men and had one partner in the last 3 months.
Characteristics of the men who have sex with men who participated in the study. N=612, Catalonia (Spain).
| Total (n=612) | Negative HIV test (n=589) | Reactive HIV test (n=21) | ||
|---|---|---|---|---|
| Last HIV test performed | n (%) | n (%) | n (%) | p Value |
| Never | 69 (11.3) | 66 (11.2) | 3 (14.3) | 0.06 |
| <1 year | 246 (40.2) | 240 (40.7) | 6 (28.6) | |
| 1−3 years | 144 (23.5) | 140 (23.8) | 3 (14.3) | |
| More than 5 years | 148 (24.2) | 139 (25.6) | 8 (38.1) | |
| Unknown | 4 (0.7) | 3 (0.5) | 1 (4.8) | |
| Sex of sexual partners | ||||
| Men | 543 (88.7) | 521 (88.5) | 20 (95.2) | 0.335 |
| Men and women | 69 (11.3) | 68 (11.5) | 1 (4.8%) | |
| Sex work | ||||
| Yes | 10 (1.7) | 10 (1.7) | 0 | 0.557 |
| No | 602 (92.3) | 579 (98.3) | 21 (100) | |
| Checked the result | ||||
| No | 115 (19.1) | 108 (18.4) | 6 (28.6) | 0.237 |
| Yes | 497 (82.3) | 481 (81.6) | 15 (71.4) | |
| Median (IQR) | Median (IQR) | Median (IQR) | ||
|---|---|---|---|---|
| Age | 34 years (27−43) | 34 years (27−43) | 35 years (25−43.5) | 0.854 |
| Number of sexual partners in the last 3 months | 4 (2−10) | 4 (2−10) | 4 (1−9) | 0.579 |
CI: confidence interval; IQR: interquartile range; HIV: human immunodeficiency virus.
Early diagnosis of HIV infection reduces the morbidity and mortality of the people affected, reduces healthcare costs and modifies behaviours that foster HIV transmission.3–6 In 2015, the Joint United Nations Programme on HIV/AIDS (UNAIDS) published a report entitled "90−90–90: an ambitious treatment target to end the AIDS epidemic",28 in which it proposed that, by 2020, 90% of people living with HIV know their HIV status. It is estimated that, currently, 12% of people infected with HIV in Catalonia do not know their serological status.29 Even if the proportion of people infected who knew their serostatus approaches 90%, the target has still not been achieved.
The results of this study demonstrate that offering self-testing in outreach activities, sending and subsequently analysing samples at a reference laboratory and enabling the corresponding individuals to check their results online is a viable option in Spain for the MSM, cisgender female sex worker and trans women populations, due to both the type of sample used and fact of offering self-testing in outreach activities in a community setting. However, this intervention showed significantly different results between the groups studied in relation to rates of reactivity, whether the participants checked their results and whether the participants confirmed their results. Regarding rates of reactivity, a high proportion of participants with a reactive result for HIV was observed among the MSM (3.4%) and trans women (5.3%), whereas not even not one reactive test was detected in the group of cisgender female sex workers. Rates at which participants checked their results were inconsistent. Whereas most of the MSM participants (sex workers and non-sex workers) checked their results on the project website, the cisgender female sex workers and trans women (sex workers and non-sex workers) did so to a lesser extent. All the cisgender female sex workers and trans women were migrants and many had language comprehension difficulties. In addition, health workers frequently reported difficulties with technology use, as well as a lack of Internet access, among the cisgender female sex workers and trans women. The percentage of participants who confirmed reactive results obtained during the study was very low. Information was only available for 6 of the 22 participants with a reactive result for HIV who underwent confirmation testing (27.3%) and it is not known whether they were linked to the healthcare system. A key aspect of the public health programmes focused on early HIV diagnosis is timely provision of HIV antiretroviral treatment through an effective strategy of linkage to care, in order to improve the prognosis of the recently diagnosed patient, disrupt the current chain of transmission and prevent new infections, given that the potential for an HIV+person with an undetectable viral load to transmit the virus to a sexual partner is equivalent to zero.30 No information was available as to whether there were false positive in those for whom there was no information on whether they confirmed their reactive results.
The high rates of reactivity observed among MSM and trans women highlight the yield of the proposed strategy for these populations; the study found prevalences 34 and 53 times higher, respectively, than 0.1%, the minimum prevalence at which offering routine HIV testing is considered cost-effective.31 Conversely, the low rate at which trans women checked their results and the low percentage of confirmation of results in both groups would render this strategy difficult to implement. If only participants known to have confirmed their result were taken into account, 122 MSM should be screened to detect one HIV+MSM, such that the intervention would have a low yield if this aspect were not improved. Moreover, the fact that not one reactive result was found among the cisgender female sex workers and the fact that less than half of them checked their result demonstrate the low yield of implementing this strategy in this group.
The study has various limitations. First, no data on the acceptability of the intervention to the participating individuals is available. No acceptability survey was conducted among them. In addition, no information is available on the percentage of individuals who declined the intervention, given that in most outreach activities, healthcare workers, instead of approaching the potential participants, situated themselves in places that were visible from the recruitment sites/areas and waited for the potential participants to approach them. Secondly, as mentioned, this study had a low percentage of confirmation among participants with a reactive result. It is necessary to implement strategies to actively seek out these participants, including personalised follow-up via telephone calls to check that they have obtained their result, have confirmed their result and are referred for specialised care. In this study, the research group decided to refrain from implementing these strategies to avoid them being perceived by the participants as intrusive. Finally, convenience sampling was used and the results cannot be generalised to all MSM, sex workers and trans women in Spain.
Our results show that this intervention is viable for the populations studied but is only effective among the MSM group. This intervention could reach difficult-to-access populations who have not been reached with current screening methods, but its success would depend on improving the proportion of participants who check and confirm their result and by facilitating, as much as possible, the referral of participants with a reactive result for confirmation and eventual access to treatment. It is important to note the difficulty of gathering information about this last stage, as has occurred in other screening strategies such as screening programmes implemented at pharmacies and community centres.
FundingThis work was funded by the Consumers, Health, Agriculture and Food Executive Agency (CHAFEA) of the European Commission (Grant Agreement: 20131101) and the Department of Health of the Regional Government of Catalonia.
AuthorsC. Agustí coordinated the study in Spain, adapted the protocol to the Spanish context, analysed and interpreted the results obtained, and wrote the manuscript. R. Muñoz carried out the fieldwork, interpreted the results and helped draft the manuscript. V. González analysed the oral fluid samples and contributed to the review of the manuscript. L. Villegas, J. Fibla, M. Meroño and A. Capitán helped with the fieldwork and contributed to the review of the manuscript. L. Fernández-López contributed to the study coordination and the review of the manuscript. T. Platteau designed the Swab2know study and wrote the protocol, coordinated the study in Europe and contributed to the review of the manuscript. J. Casabona contributed to the drafting of the protocol and the review of the final version of the manuscript. All the signatories reviewed the final version of the manuscript and approved its publication.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We would like to thank the Department of Health of the regional government of Catalonia, the fieldworkers and all the participants.
Please cite this article as: Agustí C, Muñoz R, González V, Villegas L, Fibla J, Meroño M. et al. Oferta de la prueba del VIH en fluido oral en actividades de acercamiento y consulta de los resultados online: intervención piloto en Catalu˜na. Enferm Infecc Microbiol Clin. 2021;39:3–8.