To report five cases of patients diagnosed with differentiated thyroid carcinoma (DTC) with uptake in the thymic area after high-dose treatment with I-131 and to evaluate the potential causes and therapeutic management.
MethodsFive cases of young female patients with a mean age of 36.6 years (24–43) who had been treated with a mean dose of 106mCi of I-131 (100–150mCi) showing tracer uptake in the thymic area are reported. An I-131 whole-body scan (131I-WBS) was performed 7 days after therapeutic dose administration to each patient. Anterior and posterior planar images, followed by SPECT/CT of the head, neck and superior mediastinum were acquired in all patients. Thyroglobulin levels were measured with and without hormone replacement therapy in all cases. Samples taken from the superior mediastinum were sent to pathology for analysis, which confirmed the presence of thymic tissue.
ResultsTwo patients underwent elective total thymectomy due to the gross characteristics of the gland, local 131-I uptake, and high thyroglobulin levels. The remaining three patients had already undergone thymectomy as part of neck dissection during initial surgery, and no further invasive interventions were therefore performed. Pathological examination revealed no metastases in these five patients.
ConclusionsThymus visualization in young patients after administration of therapeutic doses of I-131 seems is a more common finding than usually thought. Absence of metastasis in the thymus despite high thyroglobulin levels was confirmed in all cases. Based on these results, we suggest that a more expectant and less aggressive therapeutic approach could be used. We also suggest that I-131 therapy for DTC should be considered in classification of the potential causes of true thymic hyperplasia in the subgroup of patients recovering from a stressor.
Descripción de cinco casos de pacientes diagnosticados de carcinoma diferenciado de tiroides (CDT) con captación en el área del timo después de un tratamiento con alta dosis de I-131, y evaluar las posibles causas y manejo terapéutico.
MétodosPresentamos cinco casos de mujeres jóvenes con una edad media de 36,6 años (24–43), que fueron tratadas con una dosis media de 106mCi de I-131(100–150) que mostraron captación del trazador en las región tímica. Se ralizaron rastreos de cuerpo completo a los 7 días de la administración de la dosis a todos los pacientes, se realizaron imágenes planares de cuerpo completo en proyecciones anterior, posterior y SPECT/TAC de cabeza, cuello y mediastino superior. Valorándose también los niveles de tiroglobulinas con y sin tratamiento sustitutivo hormonal. En todos los casos se confirmó mediante anatomía patológica que la captación visualizada en el mediastino superior correspondía a tejido tímico.
ResultadosDos pacientes fueron sometidas a una timectomía total debido a las características macroscópicas de la glándula, la captación de I-131 y los altos niveles de tiroglobulina. En los otros tres pacientes la timectomía ya se había realizado previamente como parte de la disección del cuello en el tratamiento quirúrgico inicial por lo que se deciden no reintervenir. Los cinco casos fueron informados por anatomía patológica como negativos para metástasis.
ConclusionesLa visualización del timo en pacientes jóvenes tras la administración de dosis terapéuticas de I-131 es un hallazgo más frecuente de lo que pudiéramos pensar.
En todos los casos se confirmó la ausencia de metástasis en el timo a pesar de los niveles elevados de tiroglobulinas. A la vista de estos resultados planteamos la posibilidad de una actitud terapéutica menos agresiva y expectante.
También proponemos que la terapia metabólica para el CDT se debe tomar en cuenta en la clasificación de las causas probables de la hiperplasia tímica verdadera en el subgrupo que incluye a los pacientes en recuperación que han sido sometidos a un factor estresante.
Differentiated thyroid carcinoma has 5–25% of local recurrence, of which 75% are nodal recurrences, 20% are in the thyroid bed and 5% in other locations. Several tools are needed to study local recurrence such as ultrasound, CT or MRI, Tg level determination before and after hormone replacement withdrawal, 131I-WBS and fine needle aspiration biopsy (FNAB).
I-131 is very important for initial staging, treatment and monitoring of DTC patients after a total thyroidectomy. In these studies doubtful uptake foci may appear due to physiological tracer distribution or true concomitant pathology.
Increased functional activity of the thymus may be physiological in children and adolescents. In adults it is associated with thymic hyperplasia, primary neoplasms, metastases, inflammatory processes or even in normal parenchyma.1
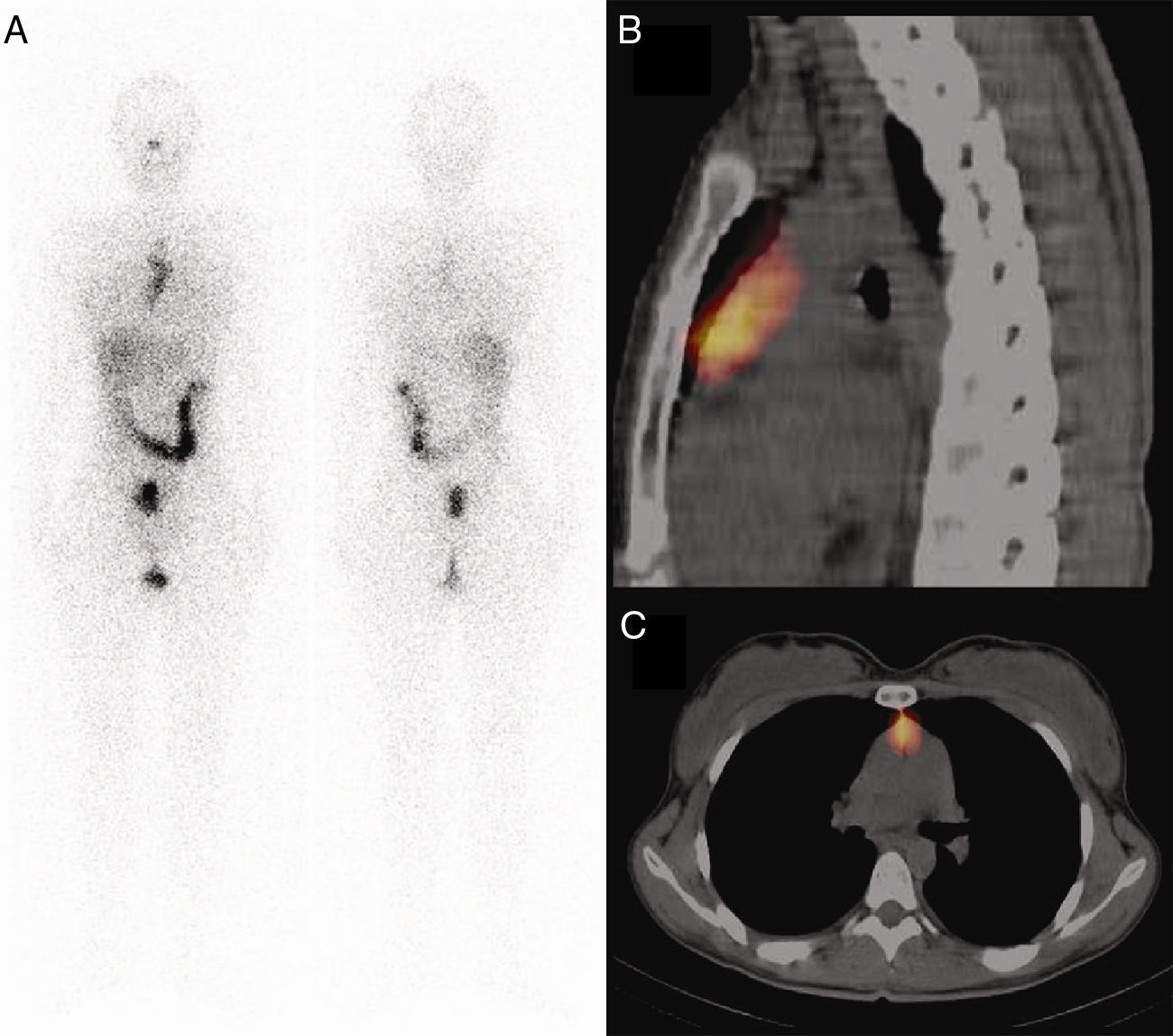
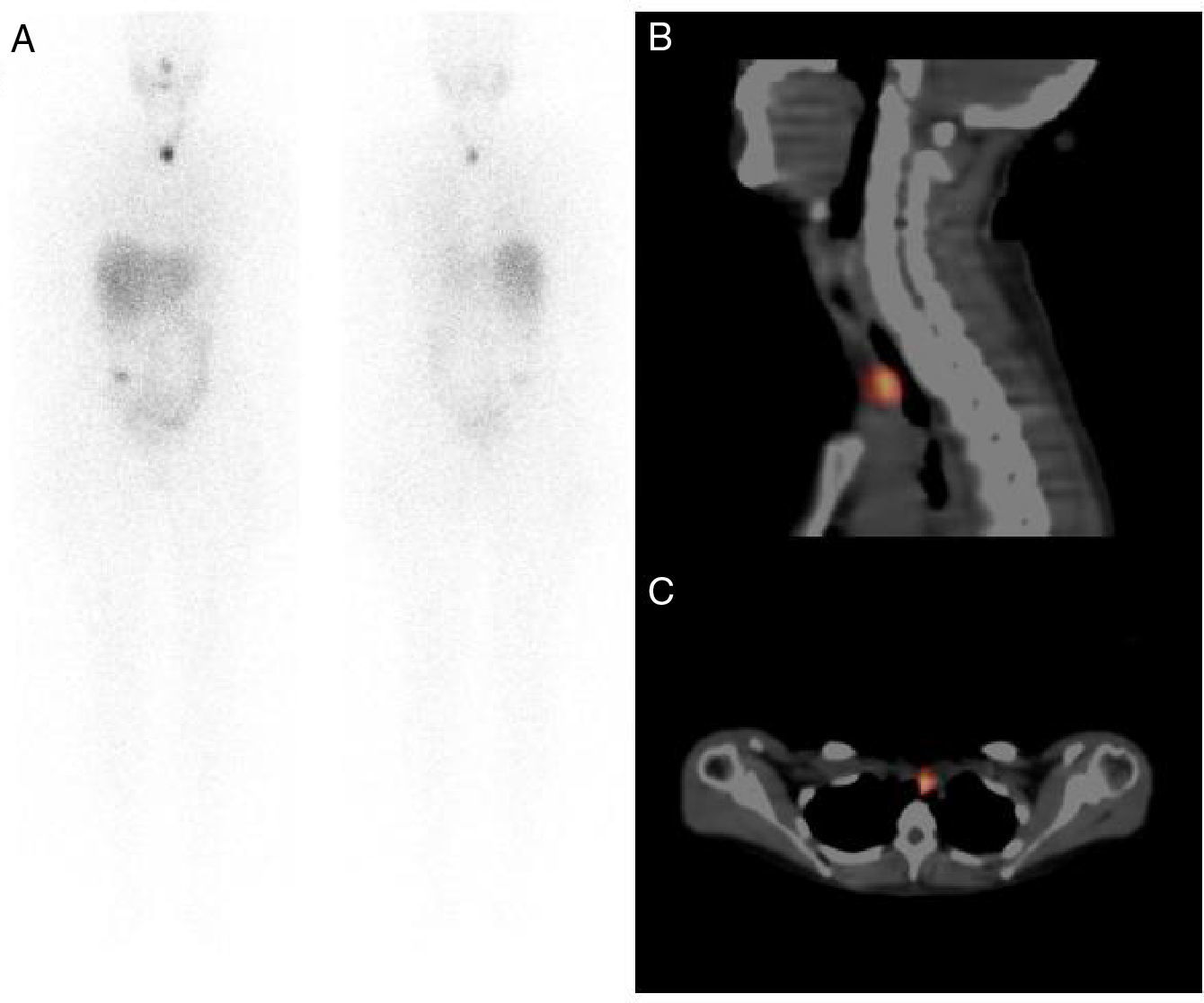
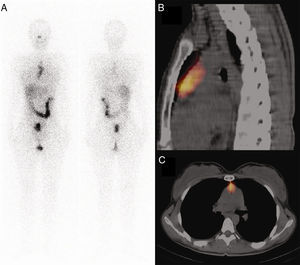
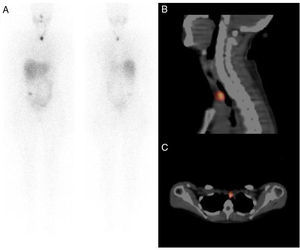
We present five cases in which after high-dose I-131 therapy we observed tracer uptake in the upper mediastinum that we identified as the thymus, with the help of our SPECT/CT (Figs. 1 and 2).
The protocol in our institution for patients with DTC includes a total or near-total thyroidectomy, all are placed on a low-iodine diet and ceased to receive thyroid hormone replacement therapy 4 weeks before radioiodine treatment.
The 131I-WBS was performed 7 days after the therapeutic dose administration. Anterior and posterior planar images followed by SPECT/CT of head, neck and upper mediastinum were performed in all patients using a Symbia TruePoint dual detector SPECT with a 2-slice CT (Siemens, Erlangen, Germany).
Thyroglobulin levels were measured with and without hormone replacement therapy as a standard protocol in all cases.
We present five cases of young female patients with a mean age of 36.6 years (24–43) diagnosed with DTC, which were treated with a mean dose of 106mCi of I-131 (100–150mCi) that showed tracer uptake in the thymic area. In 3 patients the first diagnostic scan with low dose (5mCi I-131) was negative, but because of elevated thyroglobulin levels a blind therapeutic dose of I-131 was administered (thymic uptake was seen after therapeutic dose). In the remaining two, one corresponds to a 131I-WBS after remnants ablation treatment with also a high dose of I-131 and the remaining one to a 131I-WBS after treatment for lymph node metastases in the central compartment.
In every case the samples obtained from the upper mediastinum were sent to pathology for analysis and the presence of thymic tissue was confirmed.
ResultsIn cases 1 and 2 an elective total thymectomy was performed due to the macroscopic characteristics of the gland, the local 131-I uptake and high thyroglobulin levels.
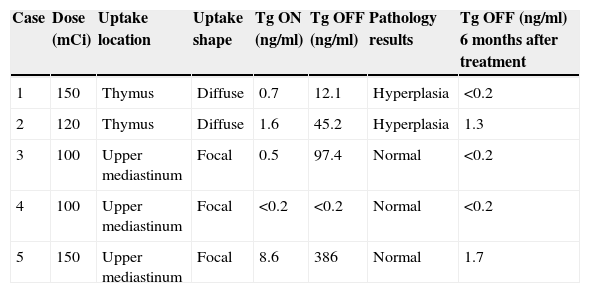
Patients 3–5 already had gone through a partial thymectomy as part of a prior neck dissection, that included level VII (superior mediastinal) during the initial surgery, so non-additional invasive procedures were considered necessary due to the normal previous pathology reports of the thymus (Table 1 for details). All five cases were reported by pathology as negative for metastasis in the thymic region.
Tg ON: Tg levels during hormone replacement therapy, Tg OFF: Tg levels after hormone replacement therapy withdrawal.
| Case | Dose (mCi) | Uptake location | Uptake shape | Tg ON (ng/ml) | Tg OFF (ng/ml) | Pathology results | Tg OFF (ng/ml) 6 months after treatment |
|---|---|---|---|---|---|---|---|
| 1 | 150 | Thymus | Diffuse | 0.7 | 12.1 | Hyperplasia | <0.2 |
| 2 | 120 | Thymus | Diffuse | 1.6 | 45.2 | Hyperplasia | 1.3 |
| 3 | 100 | Upper mediastinum | Focal | 0.5 | 97.4 | Normal | <0.2 |
| 4 | 100 | Upper mediastinum | Focal | <0.2 | <0.2 | Normal | <0.2 |
| 5 | 150 | Upper mediastinum | Focal | 8.6 | 386 | Normal | 1.7 |
In every case Tg OFF values dropped considerably 6 months after I-131 treatment (Table 1).
DiscussionThe cases described above have aroused us the concern of reviewing this issue, especially because we have found that most of the published cases like these describe a normal or hyperplasic thymus.
False positive images, as a result from thymic radioiodine uptake, are a well-known cause of unnecessary surgery.2,3 The incidence of thymus visualization on 131-I scintigraphy has been reported between 3.4% and 26.3% in four series, the largest with 489 patients by Haveman et al.4
It seems that there is a link in the embryological development between the thymus and thyroid gland; during the sixth week of gestation, the thymus arises from the third and fourth pharyngeal pouch, in the seventh week it elongates and acquires a cylindrical shape and migrates caudally to the superior mediastinum. The thyroid gland is derived from the pharyngeal epithelium, but there are suggestions of some authors that there is a contribution from the fourth pharyngeal pouch. During the migration of both glands, tissue debris might be lost and incorporated as isolated nests in either glands.6–8
There are reports of epithelial tumors with thymic differentiation in the thyroid gland.6 Also Ion mass spectrometry microscopy performed in some cases of radioiodine thymic uptake in thyroid carcinoma demonstrated iodine only in the thymic Hassall's bodies which have been considered almost identical to thyroid follicules.9
The ability to concentrate iodine is almost exclusive of thyroid tissue, but also the human symporter gene sodium-iodine (hNIS) is expressed in other tissues but with less strength like the thymus; this may explain that in most of the cases thymic uptake is observed after high therapeutic doses of radioiodine.2,5,9–12 It is also known that thymus visualization is more likely in younger patients.5
The thymus-pineal axis activity decreases significantly with age up to a gland atrophy and can even be replaced completely with fatty tissue but this does not mean it cannot be reactivated; growth and reactivation of thymic endocrine activity in aged animals who have been exogenously treated with thyroxine and triiodothyronine have been described.12 There are also reported cases of thymic hyperplasia in patients with non-treated Graves’ disease.13
Thymic hyperplasia can be divided in two types: true thymic hyperplasia and follicular hyperplasia. The true thymic hyperplasia is characterized by an increase in the size and weight of the gland with preserved microscopic features,1,14,15 whereas lymphoid or so called follicular hyperplasia consists in the appearance of lymphoid follicles within the thymus. Lymphoid follicles are similar to reactive germinal centers and contain predominantly B-lymphocytes, of which there is only a small number in the normal thymus. Although follicular hyperplasia can occur in various inflammatory or chronic immunological diseases it is more frequently found in myasthenia gravis (65–75% of patients present).16,17
Clinically, patients with true thymic hyperplasia can be classified into 3 subgroups: those who do not have a preexisting pathologic condition, those who are in recovery from a stressor such as pneumonia, steroid therapy, radiotherapy, chemotherapy, surgery and burns and those with disorders such as hyperthyroidism, sarcoidosis and red cell aplasia.1,18
As for the diagnostic and therapeutic decision in patients with these findings we believe it is essential to rely on techniques such as SPECT-CT, diagnostic CT and/or its fusion to pinpoint the thymus and assess anatomical characteristics as in case of true thymic hyperplasia, that usually is described as a diffuse enlargement, a fine blend of fatty and lymphoid tissue with regular contours and normal vessels. Michigishi et al.5 suggest that in patients with mediastinal uptake the following findings may be helpful in excluding the presence of mediastinal metastasis: mediastinal uptake which becomes visually prominent as the number of radioiodine sessions increase, mediastinal uptake which needs higher than usual doses of radioiodine to be demonstrated, detection of a diffusely enlarged thymus and no other abnormal appearance on CT scans, a serum Tg value of less than 10ng/ml 2 weeks following hormone replacement withdrawal, and young age patients, since the residual amount of thymus parenchyma that can accumulate 131-I can be higher.
With this information we can catalog cases 1 and 2 as true thymic hyperplasia and we think that can be classified in the second subgroup described earlier, associated with patients in recovery from a stressor considering that these patients are subjected to a strict diet low in iodine up to 4 weeks like in our center, hormone replacement withdrawal, complete isolation for a few days, etc. Both cases comply with almost all findings required to exclude the presence of mediastinal metastasis described above, with the exception of Tg values lower than 10ng/ml after hormone replacement withdrawal.
Given these findings, we think it is reasonable to consider taking a more conservative stance in future cases with a periodic determination of thyroglobulin levels.
ConclusionVisualization of the thymus in young patients after the administration of therapeutic doses of I-131 seems to be more frequent than we might think.
In all cases the absence of metastasis in thymus despite high levels of thyroglobulin was confirmed. With these results we propose the possibility of a more expectant and less aggressive therapeutic approach.
We also propose that I-131 therapy for DTC should be taken in consideration in the classification of possible causes of true thymic hyperplasia in the subgroup which includes patients in recovery from a stressor.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Arce MB, Molina TC, Hernández TM, de la Cinta Calvo Morón M, Herrero CH, De La Riva Pérez PA, et al. Captación tímica después del tratamiento a dosis elevadas con I-131 en pacientes con carcinoma diferenciado de tiroides: revisión breve de posibles causas y manejo. Endocrinol Nutr. 2013;62:19–23.