Laboratory tests are crucial for diagnosis and monitoring of thyroid disorders. It is therefore necessary to study the pattern and variability in requests of thyroid function tests.
The study objectives were to compare the inter-regional variability in the request of laboratory thyroid tests by general practitioners (GPs) in Spain, and to investigate the potential economic savings if the goals set for some suitability indicators were reached.
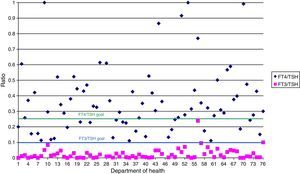
MethodsTest requests per 1000 inhabitants and test ratios (free thyroxine (FT4)/thyrotropin (TSH), free triiodothyronine (FT3)/TSH, thyroglobulin antibody (TgAb)/peroxidase antibody (TPOAb)) were compared between the different areas, according to their setting, location, and management. The resulting savings if each department achieved the goals for indicator (0.25 for FT4/TSH, 0.1 for FT3/TSH) were estimated.
ResultsSeventy-six laboratories covering a population of 17,679,195 inhabitants participated in the study. TSH was requested significantly less in urban-rural areas, and the requests for FT3/1000 inhabitants, FT3/TSH, and TgAb/TPOAb were higher in departments with private management. The savings generated if specifications for the ratios of related tests were met would be 937,260.5 €.
ConclusionsThe high variability reported in requests for thyroid function and autoimmunity tests in Spain suggests the need for implementing strategies to improve use of such tests.
Las pruebas de laboratorio son cruciales en el diagnóstico y seguimiento de las disfunciones tiroideas, lo que hace necesario estudiar cuál es el patrón de su demanda y la variabilidad en la solicitud. Los objetivos del trabajo fueron comparar la variabilidad en la solicitud de pruebas de función y autoinmunidad tiroidea (tirotropina tiroxina libre [T4L], triyodotironina libre [T3L], anticuerpos frente a la tiroglobulina [TgAb] y anticuerpos antiperoxidasa [TPOAb]) por parte de los médicos de atención primaria entre diferentes departamentos de salud españoles, y calcular el potencial ahorro económico que supondría alcanzar las metas de algunos indicadores de adecuación descritos previamente en la literatura.
MétodosSe compararon el número de pruebas por 1.000 habitantes y las ratios de pruebas relacionadas (T4L/TSH, T3L/TSH, TgAb/TPOAb) entre los diferentes departamentos en función de su ubicación, tipo de gestión y la región. Se calculó el ahorro generado si cada departamento alcanzara la meta propuesta en la literatura para los indicadores T4L/TSH (0,25) y T3L/TSH (0,1).
ResultadosUn total de 76 laboratorios que atienden a una población de 17.679.195 habitantes participaron en el estudio. La solicitud de TSH fue significativamente menor en los departamentos de salud rurales-urbanos y la solicitud de T3L, la ratio T3L/TSH y la ratio TgAb/TPOAb fueron mayores en los departamentos con gestión privada. El ahorro que se generaría si se cumplieran las especificaciones para las ratios de pruebas relacionadas ascendería a 937.260,5 €.
ConclusionesLa elevada variabilidad descrita en la solicitud de pruebas de función y autoinmunidad tiroidea en España hace necesario implementar estrategias para mejorar esta solicitud.
Thyroid dysfunctions (TDs) are the second leading cause of endocrine disease after diabetes mellitus.1 These conditions are associated, among other complications, with increases in cardiovascular complications2,3 and psychiatric disorders.4 The early detection of TDs is therefore essential, because adequate treatment prevents patient damage and complications, thus improving the course of the disease.
TD diagnosis and monitoring is currently performed at primary care (PC), usually through communication and collaboration between endocrinologists and PC physicians (PCPs). Laboratory tests are crucial for diagnosis and monitoring. In fact, the diagnosis of subclinical TD stages is based on biochemical measurements, because clinical symptoms are highly non-specific.5
Errors in requests for laboratory tests and the interpretation of their results are the factors mainly responsible for errors in TD diagnosis,6 and the participation of laboratory staff in TD management is essential.7
The measurement of thyroid-stimulating hormone (TSH) levels is the key laboratory test for the diagnosis of TDs. However, it is difficult to find a balance between the suitability of and the promotion of the request for TSH testing as a tool for early TD detection.8 Different studies and clinical guidelines recommend either processing or not processing thyroid hormone levels based on TSH levels using consensus algorithms,2,9,10 and there are a number of recommendations regarding what constitutes an adequate request for TSH measurements.11 However, in order to know to what extent the request for TSH levels should be promoted, we must first know the actual pattern of demand and the variability in the requests for thyroid function tests in Spain.
The first study objective was to compare and analyze the variability in the request for thyroid function tests among the different Spanish regions depending on the different organizational characteristics of the various healthcare departments, and the second objective was to investigate the potential savings to be derived from the achievement of the goals in some indicators of suitability previously reported in the literature.
Materials and methodsData collectionAfter the results obtained in prior studies in the Valencian Community12 and throughout Spain,13,14 141 Spanish laboratories were invited to participate via electronic mail. The activity (the number of tests requested by PCPs) during 2012 of laboratories located in different departments of health in various Spanish regions was collected. Any patient seen at a PC center of any of these departments was enrolled into the study, regardless of the reason for consultation.
Each participating laboratory was required to supply organizational data regarding the health department to which it belonged (the population covered, type of management, and location).
Five thyroid function and thyroid antibody tests were examined in a cross-sectional study: TSH, free thyroxine (FT4), free triiodothyronine (FT3), thyroglobulin antibodies (TgAb), and peroxidase antibodies (TPOAb).
Data processingAfter data collection, two types of suitability indicators were calculated: (a) the number of tests per 1000 population and (b) the ratios of related tests (FT4/TSH, FT3/TSH, and TgAb/TPOAb).
To investigate inter-practice variability, a variability index was calculated using the following formula: first decile divided by lower decile (90th percentile/10th percentile). The difference between the indicators depending on department location (rural, urban, or urban-rural) and on the type of management (public or private) was also calculated.
To study request variability between regions, the results of the indicators obtained in the laboratories of the three autonomous communities with the most departments participating in the study (The Valencian Community, Andalusia, and Castile and León) were compared with each other and with the combined results of the remaining regions.
The potential savings to be achieved if all health departments reached the standard given in the literature for the indicators FT4/TSH and FT3/TSH (0.25 and 0.1 respectively) were estimated.8,12 These savings were estimated based on the reagent cost only (€1.9 per FT4 measurement), irrespective of other laboratory costs (such as staff, consumables, etc.).
Statistical methodsStatistical data processing included distribution, mean, 95% confidence interval for the mean, standard deviation, median, and interquartile range. A Kolmogorov–Smirnov test was used to analyze the distribution of the indicators. The differences between the indicators as a function of the organizational characteristics of the department and by region were calculated using a Kruskal–Wallis or a Mann–Whitney test, as appropriate. A value of p≤0.05 was used as a criterion to reject the null hypothesis.
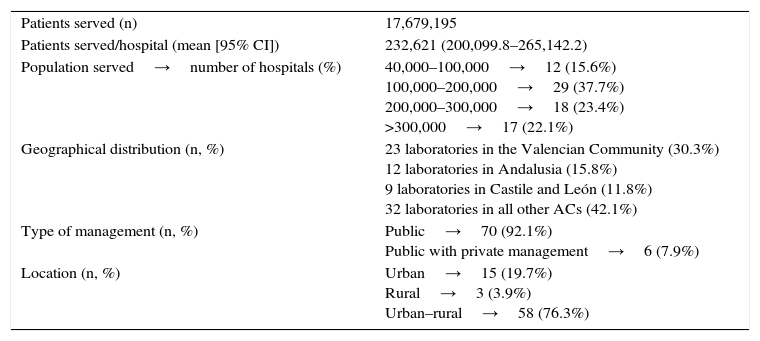
ResultsA total of 76 laboratories from the health departments of various Spanish regions covering a total population of 17,649,195 patients participated in the study. Table 1 gives a summary of the organizational data of the health departments collaborating in the study.
Descriptive characteristics of hospitals/departments participating in the study.
| Patients served (n) | 17,679,195 |
| Patients served/hospital (mean [95% CI]) | 232,621 (200,099.8–265,142.2) |
| Population served→number of hospitals (%) | 40,000–100,000→12 (15.6%) 100,000–200,000→29 (37.7%) 200,000–300,000→18 (23.4%) >300,000→17 (22.1%) |
| Geographical distribution (n, %) | 23 laboratories in the Valencian Community (30.3%) 12 laboratories in Andalusia (15.8%) 9 laboratories in Castile and León (11.8%) 32 laboratories in all other ACs (42.1%) |
| Type of management (n, %) | Public→70 (92.1%) Public with private management→6 (7.9%) |
| Location (n, %) | Urban→15 (19.7%) Rural→3 (3.9%) Urban–rural→58 (76.3%) |
CI: confidence interval for the mean; ACs: autonomous communities.
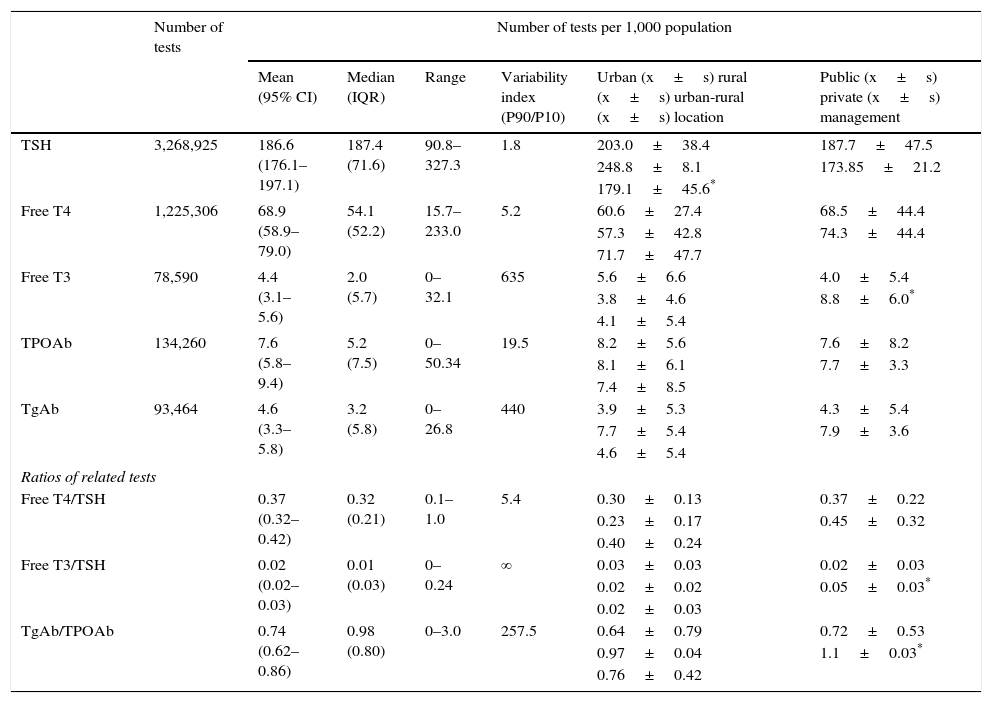
Descriptive statistics and the variability index of indicators are shown in Table 2. TSH was requested up to three times more frequently in some health departments. Variability in FT4 requests was also high, as the test was requested up to approximately 14 times more frequently in some departments. Seven laboratories that did not perform FT3 measurements are shown. Variability in requests for thyroid antibody (TPOAb and TgAb) testing was even greater as compared to all other tests.
Descriptive statistics and variability index (90th percentile/10th percentile) for each of the indicators proposed and their relationship with study variables.
| Number of tests | Number of tests per 1,000 population | ||||||
|---|---|---|---|---|---|---|---|
| Mean (95% CI) | Median (IQR) | Range | Variability index (P90/P10) | Urban (x±s) rural (x±s) urban-rural (x±s) location | Public (x±s) private (x±s) management | ||
| TSH | 3,268,925 | 186.6 (176.1–197.1) | 187.4 (71.6) | 90.8–327.3 | 1.8 | 203.0±38.4 | 187.7±47.5 |
| 248.8±8.1 | 173.85±21.2 | ||||||
| 179.1±45.6* | |||||||
| Free T4 | 1,225,306 | 68.9 (58.9–79.0) | 54.1 (52.2) | 15.7–233.0 | 5.2 | 60.6±27.4 | 68.5±44.4 |
| 57.3±42.8 | 74.3±44.4 | ||||||
| 71.7±47.7 | |||||||
| Free T3 | 78,590 | 4.4 (3.1–5.6) | 2.0 (5.7) | 0–32.1 | 635 | 5.6±6.6 | 4.0±5.4 |
| 3.8±4.6 | 8.8±6.0* | ||||||
| 4.1±5.4 | |||||||
| TPOAb | 134,260 | 7.6 (5.8–9.4) | 5.2 (7.5) | 0–50.34 | 19.5 | 8.2±5.6 | 7.6±8.2 |
| 8.1±6.1 | 7.7±3.3 | ||||||
| 7.4±8.5 | |||||||
| TgAb | 93,464 | 4.6 (3.3–5.8) | 3.2 (5.8) | 0–26.8 | 440 | 3.9±5.3 | 4.3±5.4 |
| 7.7±5.4 | 7.9±3.6 | ||||||
| 4.6±5.4 | |||||||
| Ratios of related tests | |||||||
| Free T4/TSH | 0.37 (0.32–0.42) | 0.32 (0.21) | 0.1–1.0 | 5.4 | 0.30±0.13 | 0.37±0.22 | |
| 0.23±0.17 | 0.45±0.32 | ||||||
| 0.40±0.24 | |||||||
| Free T3/TSH | 0.02 (0.02–0.03) | 0.01 (0.03) | 0–0.24 | ∞ | 0.03±0.03 | 0.02±0.03 | |
| 0.02±0.02 | 0.05±0.03* | ||||||
| 0.02±0.03 | |||||||
| TgAb/TPOAb | 0.74 (0.62–0.86) | 0.98 (0.80) | 0–3.0 | 257.5 | 0.64±0.79 | 0.72±0.53 | |
| 0.97±0.04 | 1.1±0.03* | ||||||
| 0.76±0.42 | |||||||
CI: confidence interval for the mean; IQR: interquartile range; P10: 10th percentile; P90: 90th percentile; TgAb: thyroglobulin antibodies; TPOAb: peroxidase antibodies; x±s: mean±standard deviation.
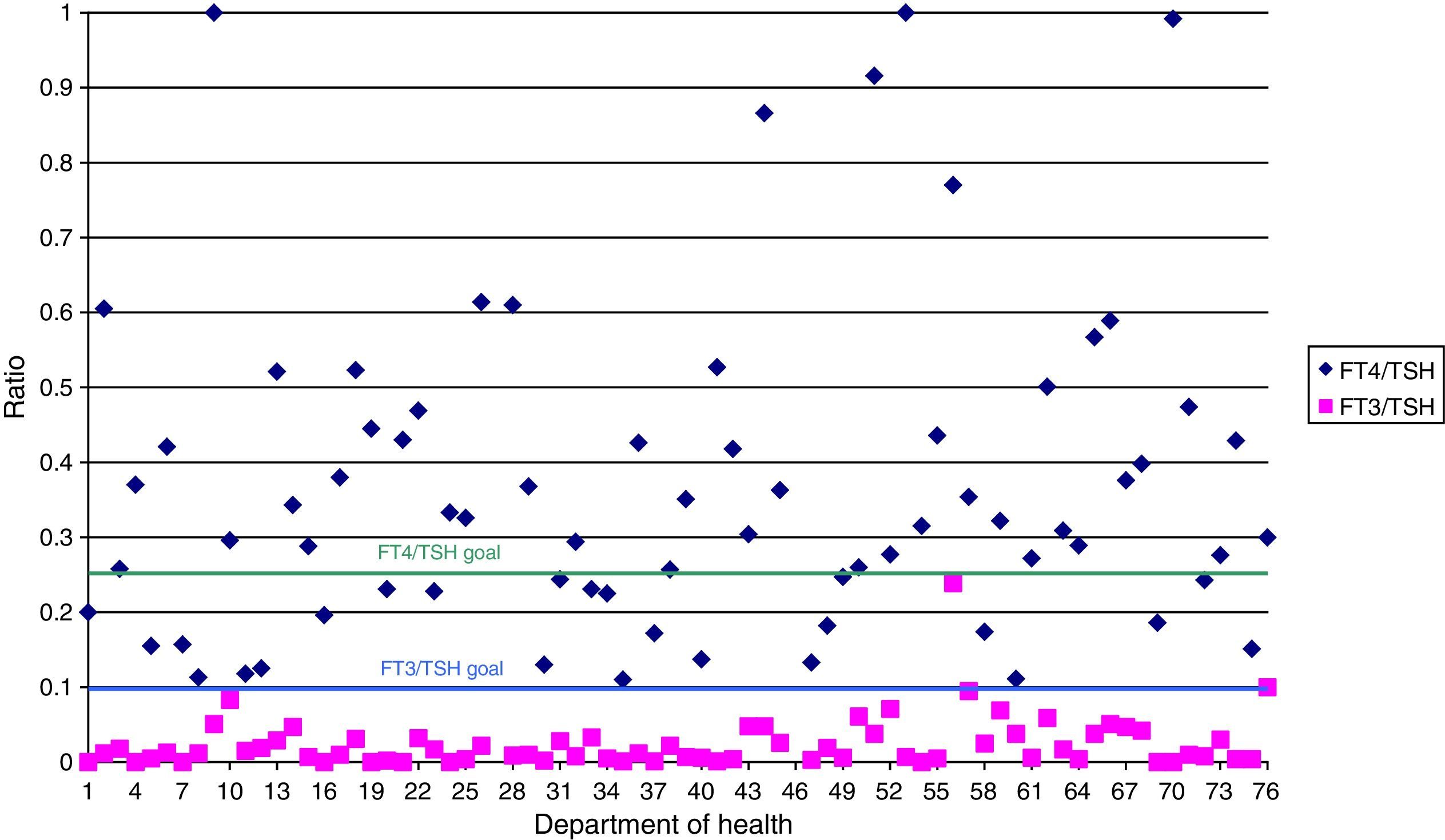
Fig. 1 shows the number of laboratories that reached the established goal in FT4/TSH and FT3/TSH ratios. Only 24 laboratories reached the desirable value of the FT4/TSH indicator. The FT3/TSH objective, however, was achieved in almost all indicators.
As regards differences between indicators depending on the location of the health department, requests for TSH testing was significantly lower in urban–rural departments as compared to urban and rural departments.
The indicators FT3/1000 population, FT3/TSH, and TgAb/TPOAb were significantly higher in laboratories under private management. These results may also be seen in Table 2.
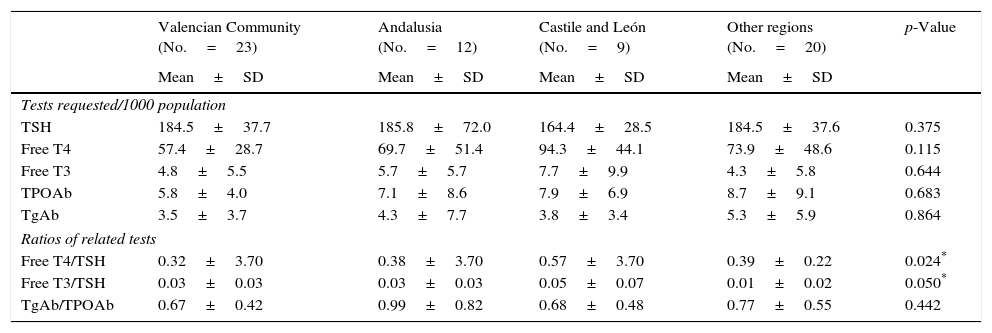
Table 3 shows the differences in each suitability indicator between regions. The indicators FT4/TSH and FT3/TSH were significantly higher in the autonomous community of Castile and León.
Comparison of the different Spanish regions: Valencian Community, Andalusia, Castile and León, and other regions.
| Valencian Community (No.=23) | Andalusia (No.=12) | Castile and León (No.=9) | Other regions (No.=20) | p-Value | |
|---|---|---|---|---|---|
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | ||
| Tests requested/1000 population | |||||
| TSH | 184.5±37.7 | 185.8±72.0 | 164.4±28.5 | 184.5±37.6 | 0.375 |
| Free T4 | 57.4±28.7 | 69.7±51.4 | 94.3±44.1 | 73.9±48.6 | 0.115 |
| Free T3 | 4.8±5.5 | 5.7±5.7 | 7.7±9.9 | 4.3±5.8 | 0.644 |
| TPOAb | 5.8±4.0 | 7.1±8.6 | 7.9±6.9 | 8.7±9.1 | 0.683 |
| TgAb | 3.5±3.7 | 4.3±7.7 | 3.8±3.4 | 5.3±5.9 | 0.864 |
| Ratios of related tests | |||||
| Free T4/TSH | 0.32±3.70 | 0.38±3.70 | 0.57±3.70 | 0.39±0.22 | 0.024* |
| Free T3/TSH | 0.03±0.03 | 0.03±0.03 | 0.05±0.07 | 0.01±0.02 | 0.050* |
| TgAb/TPOAb | 0.67±0.42 | 0.99±0.82 | 0.68±0.48 | 0.77±0.55 | 0.442 |
SD: standard deviation; TgAb: thyroglobulin antibodies; TPOAb: peroxidase antibodies.
If each laboratory had reached the goals stated in the literature8,12 for the indicator FT4/TSH, 493,295 FT4 tests, which would have cost €937,260.5 in 2012, would not have been processed.
DiscussionThe study demonstrated the great variability in Spain regarding requests from PC for tests related to thyroid metabolism. The great variability seen in requests for TSH measurements suggests that the test may be overused in some health departments and underused in others.
All but three laboratories participating in the study performed fewer measurements of FT4 as compared to TSH. However, only 24 laboratories reached the goal described for the indicator. The measurement of TgAb also appears to have been overused. The proportion of TgAb requests seems greater than expected, although in some areas patients with thyroid cancer may be treated in PC. This may indicate that in some regions PCPs are probably requesting these tests inappropriately, or that the agreed algorithms are not being applied at laboratories despite the recommendations.11
Variability in test requests may be explained by regional differences in thyroid dysfunction, or may be due to differences in the prevalence of iodine deficiency, which is not always uniform in Spain. In fact, this deficiency is more prevalent in some health departments.15–17 However, the variability seen is so high that it is probably due to additional reasons.
In one of the healthcare departments considered, 327.3 TSH tests/1000 population were requested. TSH measurement has been promoted for years8 because it is an affordable test (financially and technically) and allows for the diagnosis of a potentially serious disease. But to what extent should requests for this test be promoted? The test is very helpful in many situations: women over 40 years of age with mild psychological/psychiatric symptoms18 or pregnant women.19 However, despite the high prevalence of TD, the high request rates for TSH levels by some health departments are difficult to understand. On the other hand, a request rate of 90.8 TSH tests/1000 population appears to be insufficient for detecting TD, especially in the elderly.20–22
Historically, thyroid tests were the first group of tests processed based on algorithms, depending on TSH and FT4 results. The measurement of TSH is the best test for screening TDs in PC.7 In fact, most scientific bodies recommend the measurement of TSH for the detection of TDs in PC, provided the test used has a functional sensitivity of 0.02mIU/L or less.23–25 This is the reason for the lower request rate of FT4 as compared to TSH in most healthcare departments. There were, however, two departments where the ratio in the demand for both tests continued to be 1:1, and more than half the departments studied did not reach the value of 0.25 for the FT4/TSH indicator. The request rate for FT3 was very low and reached the value of 0.1 proposed for the FT3/TSH indicator in all laboratories. This low request rate demonstrated that the measurement of FT3 has little clinical application, although when combined with FT4 measurement it may be helpful for uncommon or complex conditions of hyperthyroidism and other unusual situations. The measurement of FT3 levels may be relevant for the diagnosis of some cases of hyperthyroidism due to multinodular goiter, thyrotoxicosis from Graves–Basedow disease versus other causes of hyperthyroidism, the evaluation of thyroid changes in the setting of serious illness, in conditions causing changes in thyroid hormone binding proteins, genetic disorders of intracellular thyroid hormone transport, and in the monitoring of treatments with hyperthyroidism.26
It is difficult to know whether requests for TPOAb tests are adequate. In fact, there is controversy regarding the value of TgAb measurement for assessing the presence of autoimmune thyroid disease.27 TgAb testing is only helpful for monitoring patients operated on for differentiated thyroid carcinoma. However, elevated titers may be found in subjects with autoimmune thyroiditis. TgAb are only present in 8–36% of the population, and measurement is only relevant in patients operated on for differentiated thyroid carcinoma.28 It therefore appears to be requested excessively, although additional studies are needed to confirm this. The value of the TgAb/TPOAb indicator was 1 in 95% of the healthcare departments analyzed. This result shows that laboratory staff should work together with endocrinologists and PCPs to achieve an adequate request rate by designing and implementing protocols for the optimum and cost-effective management of patients with TDs.
The study showed no differences in request rates between urban, rural, or urban-rural departments, except for TSH tests, which were significantly less requested in urban-rural departments. This may be explained by an older population in these departments, the request habits of PCPs, or a less common referral to endocrinology.
The significantly higher results in the FT3/1000 population, FT3/TSH, and TgAb/TPOAb indicators at private institutions may suggest a lower efficiency in the application of algorithms for thyroid function and autoimmunity tests at these centers as compared to public institutions. On the other hand, an older population may explain the higher results in the FT4/TSH and FT3/TSH indicators in Castile and León as compared to all other regions.29
The savings that could have been achieved if the FT4/TSH indicator had reached the proposed goal are high. Or as other authors have put it, “(c)ollaborations among primary care physicians, laboratory professionals, and bioinformatics experts could generate electronic tools to address the challenges identified…, thus enhancing the safety, effectiveness, efficiency, and timeliness and decreasing the cost of clinical laboratory testing”.30
Our study has some limitations. First of all, differences in requests for laboratory tests between the different Spanish regions may partly be explained by the greater or lesser extent to which PCPs manage thyroid disease at the healthcare departments studied, by disease variations between regions, and even by differences in iodine deficiency between departments, since no analysis has been made as to whether or not there is an association between changes in demand and iodine deficiency. Second, it could not be established whether the tests analyzed had all been individually requested by PCPs or whether the laboratory request policy (request profiles or algorithms) influenced the data so that they reflect laboratory practices rather than clinical behavior. Finally, it is difficult to ascertain if the tests were being overused or underused without examining the clinical data of the patients. It is not known if the reason for the request was the screening of a population with other problems, such as non-specific general symptoms, amenorrhea, obesity, etc., or a clear thyroid dysfunction, or the monitoring of a dysfunction under treatment. It may only be assumed that if requests were made by PCPs, the main reason was the diagnosis or monitoring of primary hyperthyroidism. Finally, whether the results were used to start treatment, to refer the patient to a specialist, or were simply recorded as data is also unknown.
In fact, the “ideal” ratios to be achieved of 0.25 and 0.1 for FT4/TSH and FT3/TSH are considered in our study to be hypothetical indicators of potential economic savings, but in fact have no clinical rationale.
The great variability in requests for laboratory tests to assess thyroid function and autoimmunity in Spain suggests the need for designing and implementing interventions to improve the use of the clinical laboratory. Collaboration between departments and regions is crucial for developing protocols and guidelines for optimizing the use of thyroid tests and the taking of clinical decisions.
Conflicts of interestNone to declare.
This research has received a grant (Investigación Ignacio H. de Larramendi research grants) from Fundación MAPFRE.
The members of the working group for the suitability of laboratory test requests, REDCONLAB, are as follows: Alfonso Pérez-Martínez (Hospital Morales Meseguer); Amparo Miralles (Hospital de Sagunto); Ana Santo-Quiles (Hospital Virgen de la Salud, Elda); Ángeles Giménez-Marín (Hospital de Antequera); Antonio Buño-Soto (Hospital La Paz, Madrid); Antonio Gómez del Campo (Complejo Asistencial, Ávila); Antonio León-Juste (Hospital Juan Ramón Jiménez, Huelva); Antonio Moro-Ortiz (Hospital de Valme, Seville); Begoña Laiz (Hospital Universitario y Politécnico La Fe, Valencia); Berta González-Ponce (Hospital Da Costa, Burela); Carmen Hernando de Larramendi (Hospital Severo Ochoa, Leganés); Carmen Vinuesa (Hospital de Vinarós); Cesáreo García-García (Hospital Universitario, Salamanca); Consuelo Tormo (Hospital General Universitario, Elche); Cristina Santos-Rubio (Hospital Río Tinto, Huelva); Cristóbal Avivar (Hospital de Poniente, El Ejido); Diego Benítez Benítez (Hospital de Orihuela); Eduardo Sánchez-Fernández (Hospital del Vinalopo, Elche); Emilia Moreno-Noguero (Hospital Can Misses); Enrique Rodríguez-Borja (Hospital Clínico Universitario, Valencia); Esther Roldán-Fontana (Hospital La Merced. Área de Gestión Sanitaria Sevilla Este); Fco. Javier Martín Oncina (Hospital Virgen del Puerto de Plasencia, Cáceres); Félix Gascón (Hospital Valle de los Pedroches, Pozoblanco); Fidel Velasco Peña (Hospital Virgen de Altagracia, Manzanares); Goitzane Marcaida (Consorcio Hospital General Universitario, Valencia); Inmaculada Domínguez-Pascual (Hospital General Universitario Virgen del Rocío, Seville); Isidoro Herrera Contreras (Complejo Hospitalario, Jaén); José Luis Barberà (Hospital de Manises); José Luis Quilez Fernández (Hospital Universitario Reina Sofía, Murcia); José Luis Ribes-Vallés (Hospital de Manacor); José Miguel González Redondo (Hospital Santiago Apóstol, Miranda de Ebro); José Sastre (Hospital Virgen de los Lirios, Alcoy); José Antonio Ferrero (Hospital General de Castellón); José Vicente García-Lario (Hospital Virgen de las Nieves, Granada); Juan Ignacio Molinos (Hospital Sierrallana, Torrelavega); Juan Molina (Hospital Comarcal de La Marina, Villajoyosa); Julián Diaz (Hospital Francesc de Borja, Gandía); Laura Navarro Casado (Complejo Hospitalario Universitariom, Albacete); Leopoldo Martín-Martín (Hospital General de La Palma); Lola Máiz Suárez (Hospital Universitario Lucus Augusti, HULA, Lugo); M. Dolores Calvo (Hospital Clínico, Valladolid); M. Amalia Andrade-Olivie (Hospital Xeral-Cíes, CHU Vigo); M. Ángeles Rodríguez-Rodríguez (Complejo Asistencial, Palencia); M. Carmen Gallego Ramírez (Hospital Rafael Méndez, Lorca); M. Mercedes Herranz-Puebla (Hospital Universitario, Getafe); M. Victoria Poncela-García (Hospital Universitario, Burgos); M. José Baz (Hospital de Llerena, Badajoz); M. José Martínez-Llopis (Hospital de Denia); Mabel Llovet (Hospital Verge de la Cinta, Tortosa); Mamen Lorenzo (Hospital de Puertollano); Marcos López-Hoyos (Hospital Universitario Marqués de Valdecilla); María José Zaro (Hospital Don Benito-Villanueva); Mario Ortuño (Hospital Universitario La Ribera); Marisa Graells (Hospital General Universitario, Alicante); Marta García-Collía (Hospital Ramón y Cajal, Madrid); Martín Yago (Hospital de Requena); Mercedes Muros (Hospital Nuestra Señora de la Candelaria, Tenerife); Nuria Estañ (Hospital Dr. Peset, Valencia); Nuria Fernández-García (Hospital Universitario Río Hortega, Valladolid); Pilar García-Chico Sepúlveda (Hospital General Universitario, Ciudad Real); Ruth González Tamayo (Hospital de Torrevieja); Silvia Pesudo (Hospital La Plana); Vicente Granizo-Domínguez (Hospital Universitario, Guadalajara); Vicente Villamandos-Nicás (Hospital Santos Reyes, Aranda del Duero); Vidal Pérez-Valero (Hospital Regional, Málaga). Ricardo Franquelo (Hospital Virgen de la Luz, Cuenca); Luis Rabadán (Complejo Asistencial, Soria); Concepción Magadán (Hospital Arquitecto Marcide); Fernando Rodriguez Cantalejo (Hospital Universitario Reina Sofia, Cordova); Francisco Miralles (Hospital Lluis Alcanyis, Xativa); Ignacio Arribas (Hospital Universitario Principe de Asturias); Juan Ramon Martinez Ingles (Hospital Santa Lucia, Cartagena); Raquel Blazquez (Hospital Universitario, Mostoles); Maria Luisa Lopez Yepes (Hospital Virgen del Castillo, Yecla); Maria Teresa Avello (Hospital San Agustín-Aviles).
The names of the components of REDCONLAB are available in Annex 1.
Please cite this article as: Salinas M, López-Garrigós M, Pomares FJ, Flores E, Uris J, Leiva-Salinas C. Solicitud de pruebas de función tiroidea desde Atención Primaria en España. Endocrinol Nutr. 2016;63:19–26.