Primary thyroid lymphoma (PTL) is an uncommon condition which, to be categorized as such, must only affect the thyroid gland and, eventually, the locoregional lymph nodes. Primary disease in other location should be ruled out.1,2 Diagnosis of PTL is complex, and surgery is often required to make a definitive diagnosis. Therapeutic management has greatly changed over time, and chemotherapy, with or without radiotherapy, is the current treatment of choice.1,2 We report our experience in PTL management since introduction of the new chemotherapy protocols in order to analyze: (1) the need for surgery; (2) recurrences; and (3) changes over time.
Patients treated at our hospital in the past 10 years with histological diagnosis of any of the pathological variants of PTL were selected for the study. Epidemiological, diagnostic, therapeutic, histological, and evolutionary variables were analyzed.
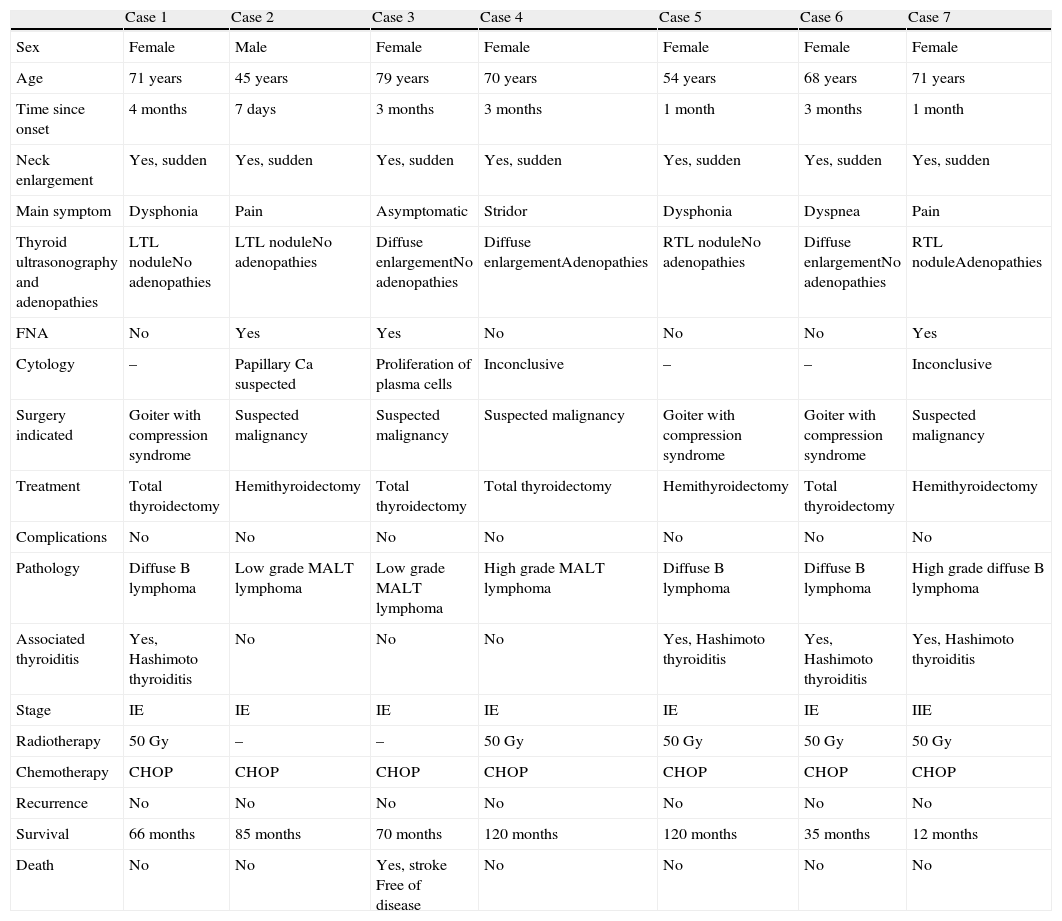
Seven patients, a majority of them women with a mean age of 64 years, met the diagnostic criteria for PTL. PTL occurred in all cases as a rapidly growing neck tumor, associated to compression symptoms in six of them (86%) (Table 1). Ultrasonography showed diffuse thyroid enlargement in 3 patients (43%) and a thyroid nodule occupying a great part of the corresponding half of the thyroid gland in the other 4 patients. Surgery was indicated in all patients, in 4 (57%) due to suspected malignancy and in the other 3 for compression symptoms. Five patients (71%) underwent total thyroidectomy, and the other 2, hemithyroidectomy. There were no postoperative complications. Four patients (57%) had a diffuse B lymphoma, and 3 patients a low grade MALT lymphoma. B lymphomas were associated to Hashimoto thyroiditis. A stage IE tumor was found in 6 patients (86%), and the remaining patient had a stage IIE tumor. All patients were given adjuvant CHOP chemotherapy (cyclophosphamide, adriamycin, vincristine, and prednisone), associated to radiotherapy with 50Gy in 5 patients (71%). Six patients are currently alive and free of disease, and one patient died at 8 years for a cause unrelated to the disease.
Cases of primary thyroid lymphoma.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
| Sex | Female | Male | Female | Female | Female | Female | Female |
| Age | 71 years | 45 years | 79 years | 70 years | 54 years | 68 years | 71 years |
| Time since onset | 4 months | 7 days | 3 months | 3 months | 1 month | 3 months | 1 month |
| Neck enlargement | Yes, sudden | Yes, sudden | Yes, sudden | Yes, sudden | Yes, sudden | Yes, sudden | Yes, sudden |
| Main symptom | Dysphonia | Pain | Asymptomatic | Stridor | Dysphonia | Dyspnea | Pain |
| Thyroid ultrasonography and adenopathies | LTL noduleNo adenopathies | LTL noduleNo adenopathies | Diffuse enlargementNo adenopathies | Diffuse enlargementAdenopathies | RTL noduleNo adenopathies | Diffuse enlargementNo adenopathies | RTL noduleAdenopathies |
| FNA | No | Yes | Yes | No | No | No | Yes |
| Cytology | – | Papillary Ca suspected | Proliferation of plasma cells | Inconclusive | – | – | Inconclusive |
| Surgery indicated | Goiter with compression syndrome | Suspected malignancy | Suspected malignancy | Suspected malignancy | Goiter with compression syndrome | Goiter with compression syndrome | Suspected malignancy |
| Treatment | Total thyroidectomy | Hemithyroidectomy | Total thyroidectomy | Total thyroidectomy | Hemithyroidectomy | Total thyroidectomy | Hemithyroidectomy |
| Complications | No | No | No | No | No | No | No |
| Pathology | Diffuse B lymphoma | Low grade MALT lymphoma | Low grade MALT lymphoma | High grade MALT lymphoma | Diffuse B lymphoma | Diffuse B lymphoma | High grade diffuse B lymphoma |
| Associated thyroiditis | Yes, Hashimoto thyroiditis | No | No | No | Yes, Hashimoto thyroiditis | Yes, Hashimoto thyroiditis | Yes, Hashimoto thyroiditis |
| Stage | IE | IE | IE | IE | IE | IE | IIE |
| Radiotherapy | 50Gy | – | – | 50Gy | 50Gy | 50Gy | 50Gy |
| Chemotherapy | CHOP | CHOP | CHOP | CHOP | CHOP | CHOP | CHOP |
| Recurrence | No | No | No | No | No | No | No |
| Survival | 66 months | 85 months | 70 months | 120 months | 120 months | 35 months | 12 months |
| Death | No | No | Yes, stroke Free of disease | No | No | No | No |
PTL is an uncommon disease with a greater incidence in women over 60 years of age. Risk of PTL development is 80-fold higher in lymphocytic Hashimoto thyroiditis, but evolution from this condition to lymphoma is uncommon (0.1%).1 In our series, B lymphoma was universally associated to Hashimoto thyroiditis, but in no case to MALT lymphomas.
The most common clinical presentation is a rapidly growing mass that causes symptoms due to compression or tissue infiltration, as seen in our patients. Some authors suggest that patients often experience neck adenopathies, but these did not occur in most of our patients. It should be noted that B symptoms only occur in 10% of thyroid lymphomas.1,2
Diagnosis of certainty usually requires a surgical biopsy, because most examinations have a low sensitivity for diagnosis of lymphoma.2 However, although surgical biopsy appears to be the gold standard for diagnosis, fine needle aspiration (FNA) should be the initial test of choice. Conventional cytological examination will probably be insufficient, and should therefore be supplemented with immunohistochemistry, molecular techniques, flow cytometry, and detection of monoclonal Ig heavy chains by PCR.3 However, this technology may not be available in many hospitals. Thus, Matsuzuka et al.4 stated that 78% of cases may be adequately diagnosed by FNA, and Graff-Baker et al.5 reported an 81% decrease in surgery in their 1973–1987 series, and a 61% decrease in their 1997–2005 series. It should be noted, however, that many patients diagnosed with rapidly growing goiter suspected of malignancy still undergo surgery to make a definitive diagnosis.6 It should be reminded that most PTLs are non-Hodgkin lymphomas, either diffuse large B cell lymphoma or MALT lymphoma, with the follicular, small lymphocytic, and Burkitt subtypes being less common.2,5 All tumors in our series were B cell or MALT lymphomas.
Surgery used to be the standard treatment, but the current treatment of choice is CHOP chemotherapy, and association of rituximab, with or without radiotherapy, is now recommended.7 Some authors prescribe radiotherapy without chemotherapy for low grade lymphomas,8 especially MALT lymphomas.9 Today, the only situation where thyroidectomy could be indicated would be stage IE MALT lymphoma, in which it would lead to a better prognosis as compared to chemotherapy. Treatment is decided based on the Ann Arbor stage. Prognosis depends on disease stage, and 5-year survival rates for stages IE, IIE, and iii-IVE are 80%, 50%, and 35% respectively.1,10 Patients in our series were in poorly advanced stages, and survival to date is 100%.
In conclusion, PTL should be suspected in women with rapid thyroid growth and associated compression symptoms. If tumor is diagnosed at an early stage, prognosis is good with adequate chemotherapy and radiotherapy. Surgery is mainly useful for diagnostic purposes.
Please cite this article as: Ríos A, Rodríguez JM, Febrero B, Parrilla P. Linfoma primario del tiroides. Endocrinol Nutr. 2014;61:497-499.