Primary adrenal leiomyosarcoma is an infrequent malignant neoplasm arising from adrenal veins. These tumors probably originate from the smooth muscle layer of the adrenal vessels. Although they may be clinically silent, compressive symptoms usually appear in large tumors. Frequently, final diagnosis is made after histopathology study of the specimen because of the lack of pathognomonic signs on imaging studies.1 Only 18 cases of primary adrenal leiomyosarcoma have been reported in the international literature up to 2009.2 We describe a case of primary adrenal leiomyosarcoma which was treated by laparoscopic adrenalectomy.
A 44-year-old woman with an unremarkable medical history was admitted at our institution having an insidious right upper abdominal pain that started the previous twelve months. On physical examination, she was normotensive, and there were no signs of hypercortisolism or virilization.
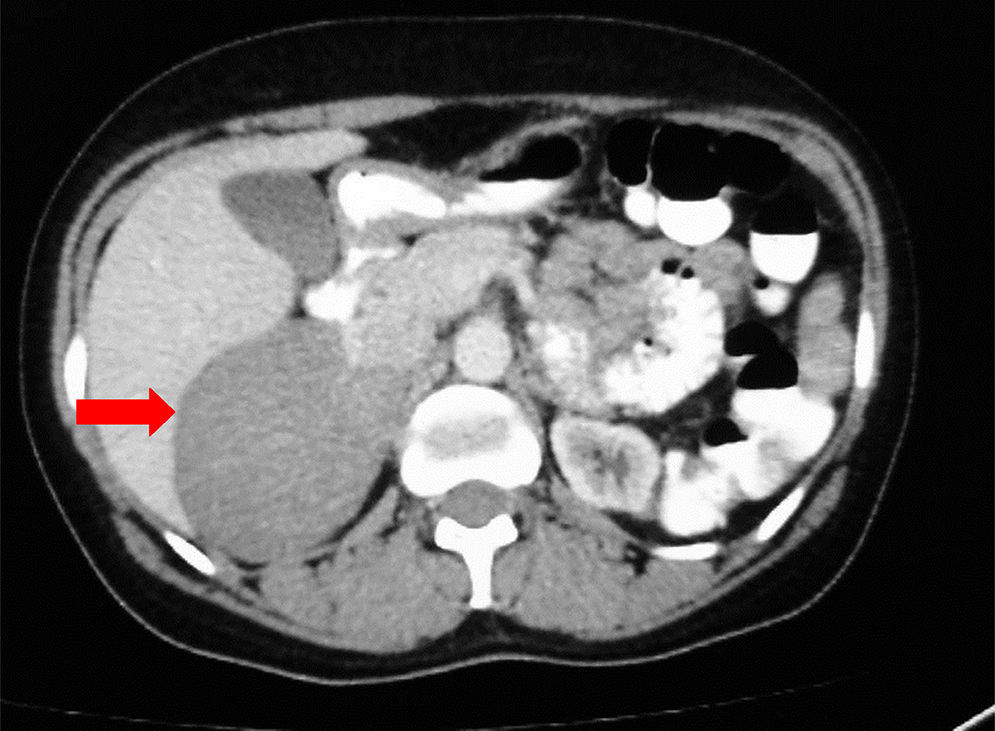
On ultrasonography a mass was diagnosed in the right adrenal gland. A computed tomography (CT, Fig. 1) scan showed an enlarged right adrenal gland measuring 7.4cm×5.2cm without evidence of regional adenopathies or infiltration of surrounding tissues. Additional tests were carried out in order to detect hormonal secretion: urinary adrenaline: 0.7μg/24h (normal<27), urinary noradrenaline 14μg/24h (normal <97), urinary vainillylmandelic acid 3mg/24h (normal <8.5), cortisol post 1mg dexamethasone 0.6μg/dl (normal<1.8).
Because of tumor size a multidisciplinary team recommended surgical excision without the use of preoperative percutaneous biopsy. At that time, the possibility to perform a PET-TC was unavailable at our institution. Laparoscopic adrenalectomy through four ports was performed according to the preoperative evaluation of the tumor size. During surgical procedure a right adrenal tumor displacing normal tissues was found and an enlarged right adrenal vein measuring 15mm was clipped and sectioned. Subsequently, a typical surgical dissection of the tumor was performed. Finally, the tumor was extracted inside a bag through an enlarged port incision. Patient was discharged on the second postoperative day. Pathological examination showed a 12cm×7cm×3.5cm adrenal tumor completely removed. Histological examination revealed interlacing fascicles of spindle cells, with elongated hyperchromatic nuclei and marked pleomorphism, with up to 12 mitoses/10 high power field. The immunohistochemical evaluation showed strong immunoreactivity forvimentin (80%), H caldhemon (90%), actin HHF35 (80%), actin smooth muscle (70%), desmin (10%), CD34 (60%), ki67 (20%). The antibodies CD117, CD68, S100 and cytokeratin AE1AE3 were negative. These results excluded other primary neoplasms such as angiosarcoma, gastrointestinal stromal tumor, metastatic carcinoma and melanoma. Final diagnosis was grade 2 (Fédération Nationale de Centres de Lutte Contre le Cancer classification) adrenal leiomyosarcoma. A multidisciplinary team evaluation decided only a close follow up performing chest and abdominal CT scans every three months for the next two years. Three years after surgery the patient remains without evidence of local or distant recurrence.
Leiomyosarcoma is a subtype of soft tissue sarcoma arising in smooth muscle and is the second most common retroperitoneal sarcoma. This tumor can arise from soft tissues, visceral, vascular structures and skin. Vascular leiomyosarcoma represents less than 2% of all leiomyosarcomas and they are frequently originated in large blood vessels of the retroperitoneum, most commonly inferior vena cava, and lower extremity.3
It is hypothesized that these tumors might arise from the principal adrenal vein or their tributaries.4 Frequently, these lesions present as a large abdominal mass with an average size greater than 10cm.5 The presence of abdominal or back pain, as in the patient presented here, is a common finding in previous reports.4–7
Adrenal leiomyosarcoma occurs equally in females and males. The majority of patients present unilateral lesions although bilateral tumors have been reported.5
The etiology of these neoplasms remains uncertain. Predisposition to the development of smooth muscle tumors is higher in immunocompromised patients, such as transplants recipients, those on chemotherapy, or those with HIV/AIDS. Epstein Barr virus infection has been reported to be involved in the oncogenesis of these neoplasms.1,2
Because of the lack of tumor markers that aid the diagnosis of leiomyosarcoma the most useful tools for characterization of adrenal tumors are the CT and magnetic resonance imaging (MRI). Nevertheless, these imaging studies commonly do not distinguish this tumor from others more frequent malignant adrenal neoplasms such as adrenal metastases and adrenocortical carcinoma. Occasionally, an intravascular thrombus can be detected on CT or MRI and this finding should alert about the possibility of the tumor might be a leiomyosarcoma.4,7 On positron emission tomography, adrenal leiomyosarcoma shows enhanced 18F-FDG uptake.8 In our patient, preoperative diagnosis of adrenal leiomyosarcoma was not achieved based on CT images and it was diagnosed after surgery.
It is accepted that multiple factors influence the biological behavior of leiomyosarcomas. Mainly, tumor size, type of surgical resection, location and histologic grade (mitotic activity, necrosis and nuclear atypia) are the most important associated features that determine the chance of local and distant recurrence.6 Mohanty et al. reported a range of recurrence nearly to 50% on a review of 13 previous published cases and this data confirm the poor prognostic observed for this malignancy.9 Recurrence can occurs early in the evolution and the development of distant metastases can affect multiple sites, most frequently lung and liver.
The low incidence of adrenal leiomyosarcoma makes it difficult to draw a consistent treatment recommendation. However, if one extrapolates the experience made with the treatment of leiomyosarcomas of others locations it would be rational that complete resection with negative margins represents the most useful therapeutic option.2 Laparoscopic approach in malignant adrenal diseases remains a controversial issue. However, reports about its feasibility have increased in the last years.10 Likewise, laparoscopic adrenalectomy is recommended in tumor less than 10cm; in our patient we chose this approach on the basis of CT findings. Discordance in size with the histological result could be explained by tumor growth until surgery. We report a successful laparoscopic resection of an adrenal leiomyosarcoma as there are few reports in the literature. Nevertheless, when the diagnosis is suspected preoperatively we advocate for an open approach. Postoperative adjuvant radiotherapy may be recommended in locally advanced tumors or after a marginal resection.11 The role of other treatments remains unclear, but leiomyosarcomas appear to be largely unresponsive to chemotherapy.
Conflict of interestNo potential conflict of interest relevant to this article was reported.