To assess glycemic control, the degree of control of cardiovascular risk factors, and treatment schemes used in patients with type 1 diabetes mellitus (T1DM) in Castilla-La Mancha (Spain).
Patients and methodsA cross-sectional, multicenter study on adult patients with T1DM seen at outpatient endocrinology clinics for 12 months (from September 2009 to August 2010). Diabetes duration was >5 years in all cases. Sociodemographic, clinical, anthropometric, and laboratory variables were collected, as well as treatment data. A multivariate logistic regression analysis was used to assess variables independently associated with good glycemic control.
ResultsA total of 1465 patients (48.5% women) with a mean age of 39.4±13.5 years and a mean diabetes duration of 19.4±10.6 years, were enrolled. Mean glycosylated hemoglobin (HbA1c) level was 7.8%, and 26% had HbA1c values≤7%. Predictors of good glycemic control (HBA1c≤7%) included intensive insulin treatment [odds ratio (OR): 2.56], non-smoking status (OR: 1.66), and a higher educational level (OR: 1.33). Fifteen percent of patients were obese, 35% had dyslipidemia, 23% were hypertensive, and 26% were smokers. Four or more of the recommended control goals were achieved by 68% of patients, but more than 33% required additional drug treatment.
ConclusionsGlycemic control was inadequate in this cohort of T1DM patients. Promotion of healthy attitudes and intensification of insulin treatment may improve glycemic control. Prevalence of cardiovascular risk factors is high, although a great proportion of patients achieve good lipid and blood pressure control.
Evaluar el grado de control glucémico y de los factores de riesgo cardiovascular y las pautas de tratamiento empleadas en pacientes con diabetes mellitus tipo 1 (DM1) atendidos en las 8 áreas de salud de Castilla-La Mancha.
Pacientes y métodosEstudio transversal multicéntrico que incluyó a pacientes diagnosticados de DM1 adultos y con más de 5 años de evolución, valorados en consultas externas durante 12 meses (septiembre 2009-agosto 2010). Se analizaron variables sociodemográficas, clínicas, antropométricas, analíticas y los tratamientos utilizados. Los factores asociados al control glucémico se estudiaron mediante un análisis de regresión logística múltiple.
ResultadosSe incluyó a 1.465 pacientes, 48,5% mujeres, con una edad media de 39,4±13,5 años y un tiempo de evolución de 19,4±10,6 años. El valor medio de la hemoglobina glucosilada (HbA1c) fue de 7,8%, y el 26% de los pacientes consiguieron HbA1c≤7%. Como factores predictivos de buen control (HbA1c≤7%) se hallaron: la utilización de pautas intensificadas de insulina con autocontrol glucémico activo (odds ratio [OR] 2,56), la ausencia de tabaquismo (OR 1,66) y alcanzar un nivel de estudios medio o superior (OR 1,33). El 15% tenían obesidad, el 35% dislipidemia, el 23% hipertensión y el 26% fumaban. El 68% de los pacientes cumplían 4 o más de los objetivos de control recomendados, precisando tratamiento farmacológico más de una tercera parte de los pacientes incluidos.
ConclusionesEl control glucémico de esta cohorte de pacientes es insuficiente. Fomentar la adquisición de hábitos saludables y la utilización de pautas de tratamiento insulínico activas podría aumentar la proporción de pacientes con un control óptimo. La prevalencia de los factores de riesgo cardiovascular es alta aunque un porcentaje amplio consigue buen control lipídico y tensional.
Type 1 diabetes mellitus (T1DM) is a chronic disease with a prevalence ranging from 0.2% to 0.4%, which accounts for 5–15% of all cases of diabetes. The incidence of T1DM is increasing in Europe1–3 and Spain,4 but with significant regional variations. In Castilla-La Mancha, recent data on the prevalence (1.44/1000 inhabitants under 15 years of age) and the incidence of T1DM in children and adolescents (27.6/100,000) suggest that they are both high in this region.5
T1DM represents a healthcare problem of less magnitude than that caused by type 2 diabetes mellitus (T2DM). In addition, the severe impact of microangiopathic chronic complications in T1DM has improved in recent decades with intervention measures.6 The results of the Diabetes Control and Complications Trial (DCCT)7 and the Epidemiology of Diabetes Interventions and Complications Study (EDIC)8 showed the benefits of more strict control of blood glucose in the intensive treatment group, where microangiopathic and macroangiopathic complications were reduced by approximately 50% in long-term follow-up.
As it occurs with T2DM patients, an integral approach to cardiovascular risk factors is currently the most adequate strategy in adult patients with T1DM. The recommended control goals are difficult to achieve in standard clinical practice, but most recent data from national registries9 show that results have improved over the years.
Few epidemiological studies are available in Spain showing the actual situation regarding metabolic control and complications in the population with T1DM.10–12 The DIACAM 1 study (DIAbetes tipo 1 en CAstilla-La Mancha, Type 1 diabetes in Castilla-La Mancha) was promoted by the Society of Endocrinology, Nutrition, and Diabetes of Castilla-La Mancha (SCAMENDI) and designed to ascertain the control and complications in patients with T1DM in the community of Castilla-La Mancha.
This first analysis addresses glycemic control, the extent of control of cardiovascular risk factors, and the treatment regimens used in the diabetic cohort enrolled into the DIACAM 1 study.
Patients and methodsDIACAM 1 was a cross-sectional, observational study of a cohort of 1465 patients aged ≥16 years with T1DM starting at least 5 years previously, where these patients were being regularly monitored at the endocrinology outpatient clinics from the 8 healthcare areas of Castilla-La Mancha (Albacete, Ciudad Real, Cuenca, Guadalajara, Mancha-Centro, Puertollano, Talavera de la Reina, and Toledo). The patients enrolled had attended the endocrinology outpatient clinics at least twice during the 12 months during which data collection took place (September 2009–August 2010). Only patients who had undergone a complete assessment of metabolic control risk factors, chronic complications, and treatments used were enrolled. Pregnant women with T1DM were excluded from the study.
Patients were classified as having T1DM based on clinical criteria (acute clinical onset with symptoms of frank hyperglycemia and ketosis or ketoacidosis) and the need for insulin therapy from the onset of diabetes or soon afterwards. In patients diagnosed in recent years, the presence of pancreatic autoimmunity was considered to classify them into the following subtypes: type 1a DM (positive autoimmunity), type 1b DM (negative immune markers with insulinopenia and baseline C-reactive peptide<1ng/mL), and latent autoimmune diabetes of the adult (LADA) (onset at >30 years with positive immune study, less acute start of symptoms, progressive impairment of pancreatic beta function, and the need for insulin therapy).
This patient sample represented one-third of the population with T1DM aged over 14 years in the autonomous community. Data were estimated from the diabetic population registries of the primary care teams in Castilla-La Mancha (Turriano, activity report of the Department of Health of Castilla-La Mancha, 2008), which showed a 5% incidence and a 0.31% prevalence of T1DM in the population aged over 14 years. For each of the 8 healthcare areas, a representative number of patients was established based on the population census.
The study was approved by the Ethics Committee (EC) of the Toledo Hospital Complex as an investigating-coordinator center, and patients gave their informed consent to participate in the study.
Variables testedThe following variables were tested in each patient:
- 1.
Demographic variables: current age, sex, type of diabetes, reference, healthcare area, ethnicity, and educational level.
- 2.
Clinical variables: age at diabetes onset, diabetes duration, and the presence of conventional cardiovascular risk factors. Patients were considered to have high blood pressure (HBP) if their systolic blood pressure (SBP) measured during the visit was ≥140mmHg and/or their diastolic blood pressure (DBP) was ≥90mmHg (mean of two measurements), or if they were receiving antihypertensive treatment. Patients were considered to have dyslipidemia if they had total cholesterol levels>200mg/dL, low density lipoprotein cholesterol (LDL-C) levels>130mg/dL, or triglyceride levels>150mg/dL, or if they were receiving lipid lowering treatment. Obesity was defined as a body mass index (BMI)≥30kg/m2, and active smoking as smoking at least 1–2 cigarettes daily for the past month.
- 3.
Anthropometric variables: weight, height, BMI, waist circumference, SBP, and DBP.
- 4.
Laboratory variables: creatinine, urea, total cholesterol, LDL-C, high density lipoprotein cholesterol (HDL-C), and triglycerides. To assess glycemic control, the mean value of the last two measurements of glycosylated hemoglobin (HbA1c) performed during the study period was used. HbA1c was measured at all sites by high pressure ion exchange chromatography (BioRad Variant II or Menarini) using methods certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized to the DCCT reference method (normal range, 4–6%). Glycemic, lipid, and blood pressure control was assessed based on recommendations by the American Diabetes Association (ADA).13
- 5.
The treatments received by each patient at the enrollment visit were:
- -
Insulin therapy: the current insulin therapy regimen, daily total dose in IU/kg/day, and time since the last change in regimen were collected. Five regimens were defined: conventional (2–3 daily doses with manual mix or fixed premixes, with one or less capillary blood glucose controls daily and occasional self-adjustment of insulin dose), premixes (≥2 doses of premixed insulin with ≥2 blood glucose controls and self-adjustment), basal-bolus with isolated self-adjustment (≤2 daily controls), basal-bolus with frequent self-adjustment (≥3 controls and daily self-adjustment of insulin dose), and continuous subcutaneous insulin infusion (CSII). Patients were considered to use an intensified insulin regimen if they used CSII or a basal-bolus regimen with frequent self-adjustment.
- -
Other treatments: data were collected on the use of antihypertensive, lipid lowering, antiplatelet aggregant, and anticoagulant drugs, and on the use of metformin as an insulin sensitizing agent.
- -
- 6.
The number of severe hypoglycemia events (defined as impaired consciousness requiring administration of intravenous glucose or glucagon by healthcare staff or relatives) occurring in the past year was collected.
Quantitative variables are given as mean±standard deviation. Descriptive analysis of qualitative variables is given as percentages with their 95% confidence intervals (95% CI). Parametric tests used included a Student's t test for means comparison and an ANOVA test to compare multiple variables, and a Tukey's HSD test was used for post hoc comparisons. Differences between proportions in qualitative variables were analyzed using a Chi-square test. To assess the factors independently associated with good glycemic control (defined as HbA1c≤7%), univariate (Chi-square) and multivariate (logistic regression) analyses were performed using different models to estimate the adjusted odds ratio (OR, 95% CI). A value of p<0.05 was considered statistically significant for all tests. SPSS V.15 software was used for data analysis.
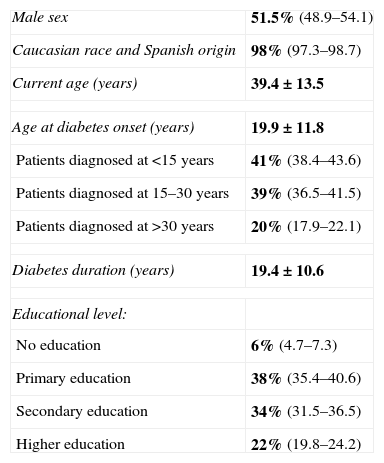
ResultsDemographic and clinical characteristicsTable 1 summarizes the characteristics of the 1465 patients enrolled in the study. Mean current age was 39 years (range, 16–83 years), mean age at diabetes onset was 20 years (range, 0.2–70 years), and mean diabetes duration 19 years (range, 5–73 years). There were no differences between healthcare areas, except in mean current age, which was somewhat higher in Cuenca and lower in the central area of La Mancha (41.9±13.7 years vs 36.2±13.7 years, p<0.05).
Clinical and demographic characteristics of the study group.
| Male sex | 51.5% (48.9–54.1) |
| Caucasian race and Spanish origin | 98% (97.3–98.7) |
| Current age (years) | 39.4±13.5 |
| Age at diabetes onset (years) | 19.9±11.8 |
| Patients diagnosed at <15 years | 41% (38.4–43.6) |
| Patients diagnosed at 15–30 years | 39% (36.5–41.5) |
| Patients diagnosed at >30 years | 20% (17.9–22.1) |
| Diabetes duration (years) | 19.4±10.6 |
| Educational level: | |
| No education | 6% (4.7–7.3) |
| Primary education | 38% (35.4–40.6) |
| Secondary education | 34% (31.5–36.5) |
| Higher education | 22% (19.8–24.2) |
Data are given as mean±standard deviation (quantitative variables) or as percentage with its 95% confidence interval (95% CI).
Values in bold are the percentage of each variable, and are given this way to emphasize data as compared to 95% CI.
As regards diabetes subtypes, 82% (95% CI: 80–84%) had type 1a diabetes, 11% (95% CI: 9.4–12.6%), and 7% (95% CI: 5.7–8.3%) LADA.
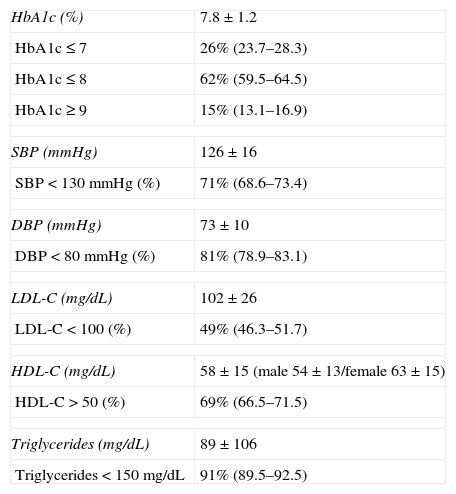
Glycemic control and related factorsMean HbA1c level was 7.8±1.2%, with levels ≤7% in 26% of the study group (Table 2). There were no differences in glycemic control between the different healthcare areas.
Glycemic, blood pressure, and lipid control results in the DIACAM 1 group. Achievement of goals of the American Diabetes Association for glycosylated hemoglobin, blood pressure, and lipids.
| HbA1c (%) | 7.8±1.2 |
| HbA1c≤7 | 26% (23.7–28.3) |
| HbA1c≤8 | 62% (59.5–64.5) |
| HbA1c≥9 | 15% (13.1–16.9) |
| SBP (mmHg) | 126±16 |
| SBP<130mmHg (%) | 71% (68.6–73.4) |
| DBP (mmHg) | 73±10 |
| DBP<80mmHg (%) | 81% (78.9–83.1) |
| LDL-C (mg/dL) | 102±26 |
| LDL-C<100 (%) | 49% (46.3–51.7) |
| HDL-C (mg/dL) | 58±15 (male 54±13/female 63±15) |
| HDL-C>50 (%) | 69% (66.5–71.5) |
| Triglycerides (mg/dL) | 89±106 |
| Triglycerides<150mg/dL | 91% (89.5–92.5) |
Data are given as mean±standard deviation (quantitative variables) or as percentage with its 95% confidence interval (95% CI). HDL-C: high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol; HbA1c: glycosylated hemoglobin; DBP: diastolic blood pressure; SBP: systolic blood pressure.
The 2010 goals of the American Diabetes Association16 include: SBP<130mmHg, DBP<80mmHg, LDL-C<100, HDL-C>50, and triglycerides<150.
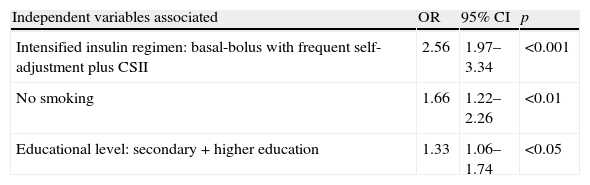
A univariate analysis of factors associated with the achievement of better glycemic control (defined as HbA1c≤7%) showed the following independent variables: educational level (middle plus higher education vs primary or no education), time since diabetes onset shorter than 10 years, absence of active smoking, absence of hyperlipidemia, absence of obesity, absence of retinopathy, and use of an intensified insulin regimen. In the multivariate analysis, variables independently associated with improved glycemic control included: use of an intensified insulin regimen with active glucose self-monitoring by patients, absence of smoking, and secondary or higher education (Table 3).
Factors associated with an improved control in the multivariate analysis (glycosylated hemoglobin≤7%).
| Independent variables associated | OR | 95% CI | p |
| Intensified insulin regimen: basal-bolus with frequent self-adjustment plus CSII | 2.56 | 1.97–3.34 | <0.001 |
| No smoking | 1.66 | 1.22–2.26 | <0.01 |
| Educational level: secondary+higher education | 1.33 | 1.06–1.74 | <0.05 |
95% CI: 95% confidence interval; CSII: continuous subcutaneous insulin infusion; OR: odds ratio.
At least one event of severe hypoglycemia was experienced by 19% (95% CI 16.8–21.2%) of patients in whom this data was recorded (n: 1222). A total of 668 events were recorded (0.54 events of severe hypoglycemia/patient/year). Fifty-two patients (4.3%) experienced recurrent severe hypoglycemia (defined as three or more events in one year). No increased risk was found in patients with intensified insulin regimens (relative risk [RR] 1.06; 95% CI 0.9–1.2) or better metabolic control by HbA1c≤7% (RR 1.06, 95% CI 0.8–1.3).
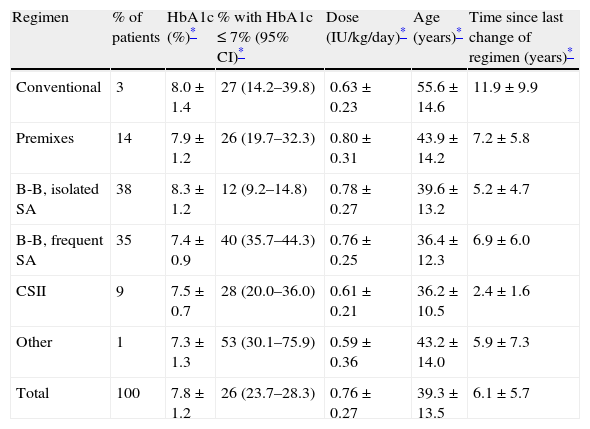
Insulin therapyMost patients enrolled into the study used physiological treatment regimens with multiple insulin doses (basal-bolus) or CSII (82%). However, only 44% used treatment with an intensified regimen with active self-monitoring. Patients on intensified regimens had better glycemic control and used lower insulin doses (Table 4). Older patients used conventional treatment regimens. The distribution of insulin therapy by healthcare areas was heterogeneous and significantly different, particularly as regards CSII, which was used in 2–26% of patients seen in each area (p<0.001).
Insulin therapy regimens: glycemic control and goals for glycosylated hemoglobin, insulin dose, and time of each regimen.
| Regimen | % of patients | HbA1c (%)* | % with HbA1c≤7% (95% CI)* | Dose (IU/kg/day)* | Age (years)* | Time since last change of regimen (years)* |
| Conventional | 3 | 8.0±1.4 | 27 (14.2–39.8) | 0.63±0.23 | 55.6±14.6 | 11.9±9.9 |
| Premixes | 14 | 7.9±1.2 | 26 (19.7–32.3) | 0.80±0.31 | 43.9±14.2 | 7.2±5.8 |
| B-B, isolated SA | 38 | 8.3±1.2 | 12 (9.2–14.8) | 0.78±0.27 | 39.6±13.2 | 5.2±4.7 |
| B-B, frequent SA | 35 | 7.4±0.9 | 40 (35.7–44.3) | 0.76±0.25 | 36.4±12.3 | 6.9±6.0 |
| CSII | 9 | 7.5±0.7 | 28 (20.0–36.0) | 0.61±0.21 | 36.2±10.5 | 2.4±1.6 |
| Other | 1 | 7.3±1.3 | 53 (30.1–75.9) | 0.59±0.36 | 43.2±14.0 | 5.9±7.3 |
| Total | 100 | 7.8±1.2 | 26 (23.7–28.3) | 0.76±0.27 | 39.3±13.5 | 6.1±5.7 |
p<0.001 for all comparisons. B-B, isolated SA: basal-bolus with isolated self-adjustment; B-B, frequent SA: basal-bolus with frequent self-adjustment; HbA1c: glycosylated hemoglobin; 95% CI: 95% confidence interval. Daily insulin dose is given as IU/kg/day; CSII: continuous subcutaneous insulin infusion. Other: widely diverse treatment regimens that could not be included in any of the five regimens defined.
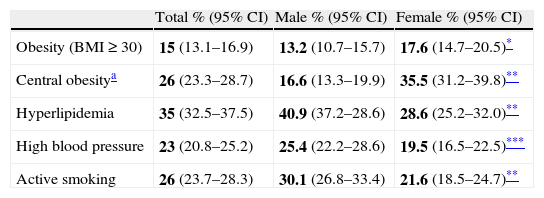
Table 5 shows the prevalence of conventional cardiovascular risk factors in study patients. Female sex was associated with a greater prevalence of obesity, while males had a greater prevalence of hyperlipidemia, HBP, and smoking. In the univariate analysis, a low educational level (no or primary education) was associated with a greater prevalence of all cardiovascular risk factors (p<0.001). Patients with any associated risk factors had significantly higher HbA1c levels (7.8% in patients with one associated risk factor vs 8.5% in patients with four associated factors; p<0.001).
Prevalence of associated conventional cardiovascular risk factors in the DIACAM 1 group, overall and by sex.
| Total % (95% CI) | Male % (95% CI) | Female % (95% CI) | |
| Obesity (BMI≥30) | 15 (13.1–16.9) | 13.2 (10.7–15.7) | 17.6 (14.7–20.5)* |
| Central obesitya | 26 (23.3–28.7) | 16.6 (13.3–19.9) | 35.5 (31.2–39.8)** |
| Hyperlipidemia | 35 (32.5–37.5) | 40.9 (37.2–28.6) | 28.6 (25.2–32.0)** |
| High blood pressure | 23 (20.8–25.2) | 25.4 (22.2–28.6) | 19.5 (16.5–22.5)*** |
| Active smoking | 26 (23.7–28.3) | 30.1 (26.8–33.4) | 21.6 (18.5–24.7)** |
95% CI: 95% confidence interval; BMI: body mass index.
For sex comparison.
Values in bold are the percentage of each variable, and are given this way to emphasize data as compared to 95% CI.
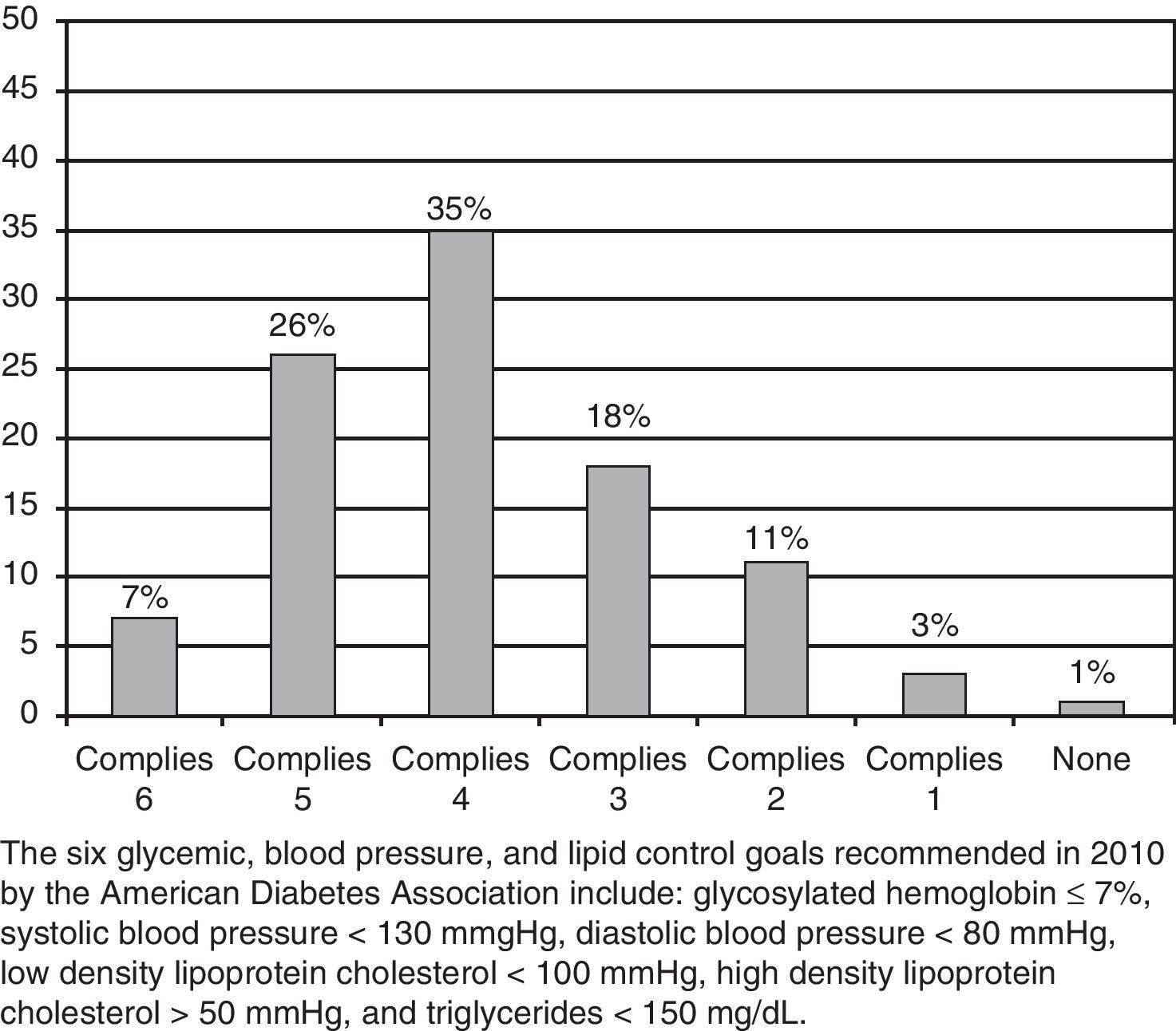
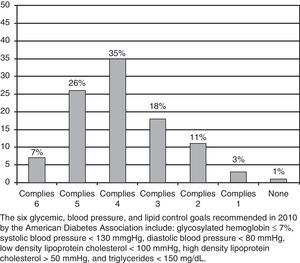
Table 2 shows mean lipid and blood pressure levels and the proportion of patients who achieved adequate control according to the recommended goals. Only 7% of patients analyzed achieved satisfactory compliance with all six control goals recommended by the ADA,13 although 61% showed a good compliance with four or five goals (Fig. 1).
Thirty-eight percent (95% CI 35.4–40.6%) of patients were receiving lipid lowering treatment, mainly statins (32%). Twenty-eight percent (95% CI 25.7–30.3%) of the group were being treated with antihypertensive drugs for HBP or nephropathy, 26.4% were taking renin–angiotensin system blockers (44% angiotensin-converting enzyme inhibitors [ACEIs], 47% angiotensin receptor blockers [ARBs], 8% combinations of ACEIs and ARBs, and 1% renin inhibitors).
DiscussionOnly one-fourth of patients in the DIACAM 1 study achieved HbA1c levels less than 7%. This study shows, in a representative cohort of the adult population with T1DM in Castilla-La Mancha, the difficulty of achieving optimum glycemic control despite the use of treatment regimens with multiple insulin doses or insulin infusion pumps. It should be noted that the vast majority of patients enrolled (62%) achieved an acceptable level of control (HbA1c≤8%), and only 15% showed poor control (HbA1c≥9%).
This difference between the goals recommended by scientific societies and the results obtained in actual practice is consistently seen in the large European9 and American14 registries of populations with T1DM. In some Spanish studies conducted on smaller groups of patients with T1DM,10–12 less than 30% of patients achieved optimum glycemic control.
The DCCT study clearly showed that intensive insulin therapy (three or more daily injections of subcutaneous pump infusion) was essential for improving blood glucose levels and patient course.7,8 Moreover, the treatment of patients with T1DM by the administration of multiple insulin doses is known to be cost-effective as compared to non-intensive treatments.15 However, control goals will not be achieved if treatment with complex and more physiological insulin regimens is not associated with the active self-adjustment of insulin dose based on carbohydrate consumption, capillary blood glycose,16 and planned physical activity.
The results of this study reflect this situation because although most our patients used multiple doses of subcutaneous insulin or CSII (82%), the results achieved by the different regimens differed significantly. The worst HbA1c results were found in the subgroup of patients using the basal-bolus regimen with no active self-adjustment. Among the 44% of patients using intensive, active insulin therapy, no differences were seen between the results achieved by patients with insulin pumps and by those using multiple insulin doses and active self-adjustment, except in the daily insulin dose used. This agrees with the literature reports.17
In Spain, CSII is used by 3–5% of the population with T1DM. Some experts estimate that approximately 15–20% of patients are likely to achieve the greatest benefit from the use of CSII.18 The choice of the most adequate insulin treatment regimen for patients with T1DM continues to be controversial because of the availability of increasingly physiological but more expensive modalities. The objective of all professionals involved in the treatment of T1DM should possibly be to try to extend the use of intensified treatment with multiple insulin doses to the greatest possible number of patients. In cases where this approach proves ineffective, the group of patients who may achieve the greatest benefit from pump treatment, or patients who should use more conventional insulin therapy regimens because of their profile, should be identified.
The occurrence rate of severe hypoglycemia found in this study was somewhat lower than that reported in other clinical studies of patients with T1DM,19 and also lower than that recently estimated in Spanish patients with T1DM.20 The use of insulin analogs in most of our patients and the proportion of T1DM patients using insulin pumps may possibly have contributed to these results.21 It should also not be forgotten that severe hypoglycemia results in significant direct healthcare expenses, and its prevention based on educational programs and active self-monitoring will contribute to decreasing its social, psychological, and financial impact.20
However, some results of the DIACAM 1 study suggest how the final results of glycemic control goals may be improved. Thus, smoking cessation and greater patient involvement in treatment self-adjustment and insulin regimen intensification would allow for achieving better HbA1c levels and for reaching control goals in a higher proportion of patients. It should also be noted that more than 40% of patients in our group had no or only primary education. In this regard, recent data suggest that a low socioeconomic and educational status of patients with T1DM has a negative impact on disease self-care, glycemic control,22 and the occurrence of chronic complications.23
More than one-fourth of study patients were active smokers, and an even higher percentage of smokers were found in patients under 40 years of age, mainly male. Smoking has been independently associated with greater insulin resistance and poorer metabolic control in T1DM.24 Therefore, the prevention of active smoking and the development of educational programs for smoking cessation in adolescents and adults with T1DM should be part of treatment protocols and would possibly lead to improved glycemic control.
The second part of the study analyzed the prevalence of cardiovascular risk factors and their control in the study cohort. Although most studies on cardiovascular risk have focused on patients with T2DM, T1DM is also associated with an increased incidence of cardiovascular disease in both males and females.25 Each type of diabetes has a clearly different cardiovascular risk profile, but our data show that the proportion of T1DM patients with conventional risk factors is substantial and similar to that reported in other studies.9,10,14 However, a high number of patients received treatment in this study and goal achievement was good, although clearly improvable for the LDL-C goal.
Some studies in patients with T1DM have shown sex differences in predictors of cardiovascular disease.25 Microalbuminuria is also a factor strongly associated with the pathogenesis of macroangiopathy in T1DM26 and, as occurred in this study, the prevalence of conventional cardiovascular risk factors is associated in middle-aged T1DM patients with a lower educational level.22 In addition, some studies suggest that in young patients with T1DM in our environment and in the absence of other risk factors, there is evidence of accelerated, preclinical atherosclerosis, as measured by carotid intima–media thickness.27 It seems clear therefore that, in patients with T1DM, strategies to prevent cardiovascular disease should be implemented. Such strategies, combined with intensified glycemic control, would decrease the progression of atherosclerosis.8,28
The study had some limitations that should be taken into account. First, the cross-sectional design of the study did not allow for the prospective assessment of the evolution of metabolic control in the study population and its impact on microvascular and macrovascular complications. This study should possibly be continued and a community registry of patients with T1DM similar to the large national registries be implemented.29 These registries have represented a tool for the continued improvement of the quality of care in diabetic patients. In this regard, a community registry of diabetes in patients under 15 years of age has been created in Castilla-La Mancha.30 A second study limitation resulted from the selection of study patients. Since this was not a population-based study and only enrolled patients attending the endocrinology clinic, a potential bias may have been introduced by assessing only those patients who most frequently visited a physician and who were theoretically more involved in the control of their disease. Finally, it should be noted that although heterogeneity has been shown in the use of the different insulin regimens between the eight healthcare areas of Castilla-La Mancha, no differences were found between them in the degree of glycemic control, and such heterogeneity does not appear to have affected the interpretation of the results.
Finally, we conclude that the data collected in this study suggest the difficulties involved in achieving adequate glycemic control in a representative, wide group of adult patients with T1DM despite the use of complex insulin regimens in most cases. These results could be improved if we could get patients to perform more active glucose self-monitoring and to improve their lifestyles, as well as by structured educational intervention by healthcare professionals. Finally, an active approach should be maintained in cardiovascular prevention in patients with T1DM, emphasizing the significance of controlling conventional risk factors.
Conflicts of interestThe authors state that they have no conflicts of interest.
Albacete University Hospital Complex: J.J. Alfaro, S. Aznar, F. Botella, A. Hernández, C. Lamas, L. López, L. Louhibi, J.J. Lozano. Hospital Virgen de la Luz, Cuenca: M. Alramadán, S. Aranda, C. Gómez, D. Martín. Guadalajara University Hospital: V. Álvarez. Ciudad Real General Hospital: R. Chamorro, M. Delgado, P. Rozas. Mancha Centro Hospital Complex: A. García Manzanares, I. Gómez, M. López, J. Silva. Hospital Santa Bárbara, Puertollano: J.C. Padillo. Hospital Nuestra Señora del Prado, Talavera de la Reina: P. de Diego, I. Quiroga, M.A. Valero. Toledo Hospital Complex: B. Cánovas, E. Castro, I. Luque, E. Maqueda, A. Marco, E. Martínez, V. Peña, R. Sanchón, A. Vicente.
Researchers in the study group DIACAM 1 are reflected in Appendix A.
Please cite this article as: Sastre J, et al. Situación de control metabólico y pautas de tratamiento en pacientes con diabetes tipo 1 en Castilla-La Mancha: estudio de diabetes tipo 1 en Castilla-La Mancha. Endocrinol Nutr. 2012;59:539–46.