A cavernous hemangioma (CH) is a benign tumor commonly occurring in skin and liver, but extremely rare in the adrenal glands.1 Although the first case of an adrenal cavernous hemangioma (ACH) was reported in 1955,2 only 60 cases of ACH have been reported to date in the medical literature. ACHs are in most cases unilateral, non-functioning lesions occurring at between 50 and 70 years of age. Females are mainly affected, with a 2:1 sex ratio.3 Differential diagnosis of ACH with adrenal carcinoma represents a challenge for clinicians because the tumors are usually very large and, although they show some typical features in radiographic studies, the vast majority are only discovered after surgery and histological study.
We report the case of a 65-year-old male patient who was referred to our endocrinology outpatient clinic after an abdominal mass, probably dependent on the left adrenal gland, was found in an ultrasound examination. The patient first attended the gastroenterology outpatient clinic complaining of continuous, persistent pain in his left flank for the previous three months. Abdominal examination at the outpatient clinic revealed a palpable mass. An abdominal ultrasound examination showed a heterogeneous nodule with lobulated margins, approximately 7.5×6cm in diameter, in the upper pole of the left kidney, probably related to and originating in the left adrenal gland.
The patient's history included type 2 diabetes mellitus (T2DM), high blood pressure (HBP), and dyslipidemia, which were well controlled with medical treatment. The patient smoked two packs of cigarettes daily and had previously experienced a right carotid transient ischemic attack. Clinical examination at the endocrinology outpatient clinic found a weight of 78.7kg, a height of 172cm, and a BMI of 26.6kg/m2. Blood pressure levels were 137/85mmHg. Examination by organs and systems was unremarkable, except for a doubtful palpable mass in the left flank.
Laboratory tests reported normal complete blood count and coagulation values. The results of blood chemistry, including kidney, liver, bone, and lipid parameters, were also normal. HbA1c level was 5.4%. TSH and FT4 levels were normal. Basal cortisol was 12.53μg/dL (normal range, 6–28), and ACTH 17pg/mL (normal, 7.2–63.3). Urinary free cortisol (UFC) level was 88μg/24h. Normal levels were found of total and free testosterone, dehydroepiandrosterone sulphate (DHEA-S), prolactin, and 17-OH progesterone. Tumor markers: alpha-fetoprotein, β-HCG, carcinoembryonic antigen (CEA), CA 19.9, CA 125, cyfra 21.1, and prostate-specific antigen (PSA) levels were normal. Catecholamines and metanephrines in 24-h urine after a five-day diet were normal in two consecutive tests. Basal cortisol levels after a 1-mg overnight dexamethasone (DXM) suppression test were 4.89mcg/dL. After a subsequent 3-mg overnight dexamethasone (DXM) suppression test, the basal cortisol level was 1.6mcg/dL.
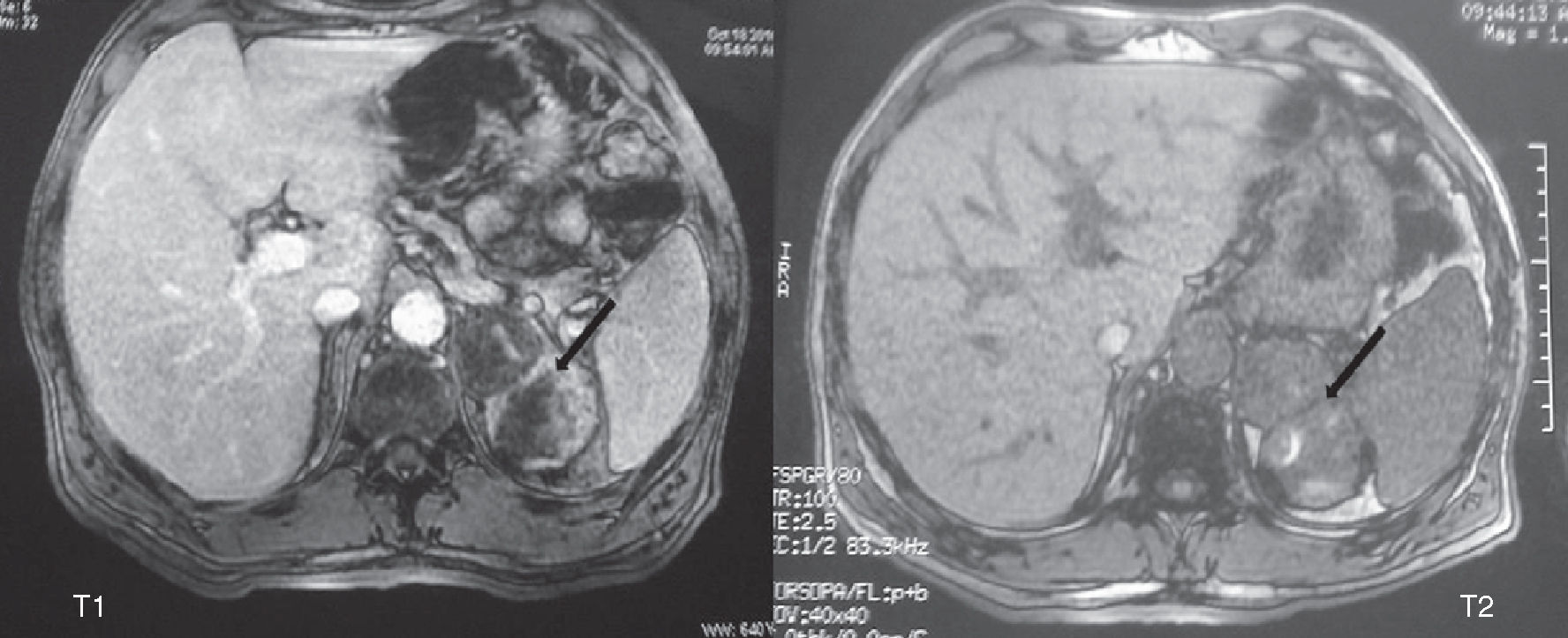
Based on these findings, resonance magnetic imaging (MRI) was performed with gadolinium, showing a bilobulated lesion 8×6cm in diameter with a heterogeneous signal in T1 and T2 sequences related to small hemorrhagic foci inside the lesion. After contrast administration, heterogeneous enhancement was seen, which was consistent with a left adrenal lesion/tumor, probably an adrenal carcinoma, although a pheochromocytoma could not be ruled out (Fig. 1). Because of this, and although the two consecutive catecholamine tests had been negative, a metaiodobenzylguanidine (MIBG) scintigraphy was performed, which was also negative.
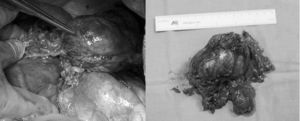
After this comprehensive diagnostic work-up and based on the results of the supplemental tests, a preliminary diagnosis of a left adrenal carcinoma was made, and surgical removal of the mass for histological study was decided upon. After approval by the anesthesiologist, a left adrenalectomy was performed through a subcostal approach. Gross examination revealed an adrenalectomy specimen 164.5g in weight and 8.5×6×4cm in diameter with a highly vascularized surface and two well-circumscribed, brownish red 4.3cm and 4.2cm nodules (Fig. 2). Microscopic examination showed a tumor well circumscribed by a fibrous capsule with two nodules consisting of a proliferation of dilated blood vessels with endothelium without atypia or mitosis, red blood cells with endothelial proliferation, and infarction areas with hemorrhage and fibrin. Final histological diagnosis was a large left adrenal cavernous hemangioma.
While a CH is a common benign tumor in certain sites, such as the liver, a CH originating in the adrenal glands is extremely rare. The importance of our case lies in the complexity of the preoperative diagnosis of this tumor. Differential diagnosis with an adrenal carcinoma and sometimes with a pheochromocytoma is difficult.4 In addition, massive spontaneous retroperitoneal hemorrhage has been reported as a complication of adrenal CH causing high morbidity and mortality rates.5
There are typical radiographic signs, not specific to an ACH, that may suggest diagnosis. In computed tomography (CT), a CH appears as a well-circumscribed mass with calcification and fat areas. In dynamic studies following the administration of intravenous contrast, progressive contrast enhancement from the periphery to the middle of the tumor is seen. In MRI, a CH appears as a heterogeneous mass with low signal intensity in T1-weighted sequences and high signal intensity in T2-weighted sequences. In the dynamic series after the administration of gadolinium, late peripheral enhancement occurs.6 Our patient first underwent abdominal ultrasonography, and adrenal MRI was subsequently performed as a confirmatory radiographic technique. Signs suggesting a possible ACH, such as size, small hemorrhagic foci, and heterogeneous contrast enhancement, were reported. Because of the rarity of ACHs and the large size of the lesion, a left adrenal carcinoma was initially considered as the most probable diagnosis.
Although the vast majority of ACHs reported were non-functioning, some exceptional cases where catecholamines, and even aldosterone, were produced by the tumor have been documented. Hormone hypersecretion does not therefore rule out its diagnosis.7 The reported patient, with a history of grade I overweight, type 2 DM, HBP, and dyslipidemia, showed inadequate cortisol suppression after the 1-mg overnight DXM suppression test. ACTH and 24-h UFC levels were within the normal range. A repeat 3-mg overnight DXM suppression test, recommended by some authors to avoid false positives,8 showed adequately suppressed basal cortisol. This showed that there was no significant autonomous cortisol production, and perioperative corticotherapy was therefore not required. If tumor growth had continued, cortisol secretion could possibly had become autonomous over time, resulting in Cushing's syndrome which would have required steroid use during and after surgery.
To conclude, an ACH is a rare tumor that should be considered in differential diagnosis of adrenal masses, particularly if they are large and unilateral and show radiographic signs which suggest this diagnosis.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please, cite this article as: González Duarte DJ, et al. Hemangioma cavernoso adrenal de gran tamaño como hallazgo inesperado tras estudio de masa abdominal. Endocrinol Nutr. 2012;59:69–83.