Parathyroid carcinoma (PC) is an uncommon disease that accounts for less than 2% of cases of primary hyperparathyroidism.1 PC is usually associated with a great variety of symptoms and severe laboratory changes, with calcium and PTH higher than those seen in adenomas.2 PC develops inside the thyroid gland in 0.2% of cases due to the inadequate embryological migration of the parathyroid gland from the third and fourth branchial arches.1,3 Less than ten cases of PC have been reported.1,3–10 A clinical case which is quite unusual due to its initial clinical manifestations, imaging studies, and diagnosis is reported here. According to a literature review, this is the first case of intrathyroid PC in an adult to be identified in Spain.
A 25-year-old male patient with a family history of osteogenesis imperfecta initially complained of fragility fractures in the wrist and ankle, and also reported asthenia, weakness, the loss of 12kg in three weeks, and generalized bone pain. A genetic study ruled out osteogenesis imperfecta. After a physical examination, a 2cm tender nodule was palpated in the right thyroid lobe; there were no other nodules or laterocervical adenopathies. Laboratory test results revealed severe hypercalcemia (17.1mg/dL; reference range, 8.5–10.5mg/dL) and a PTH level of 800pg/mL (reference range: 15–88pg/mL). The patient was admitted to hospital for medical treatment and diagnostic work-up. Hypercalcemia was controlled with fluid replacement, loop diuretics, and a single dose of calcitonin and zolendronic acid.
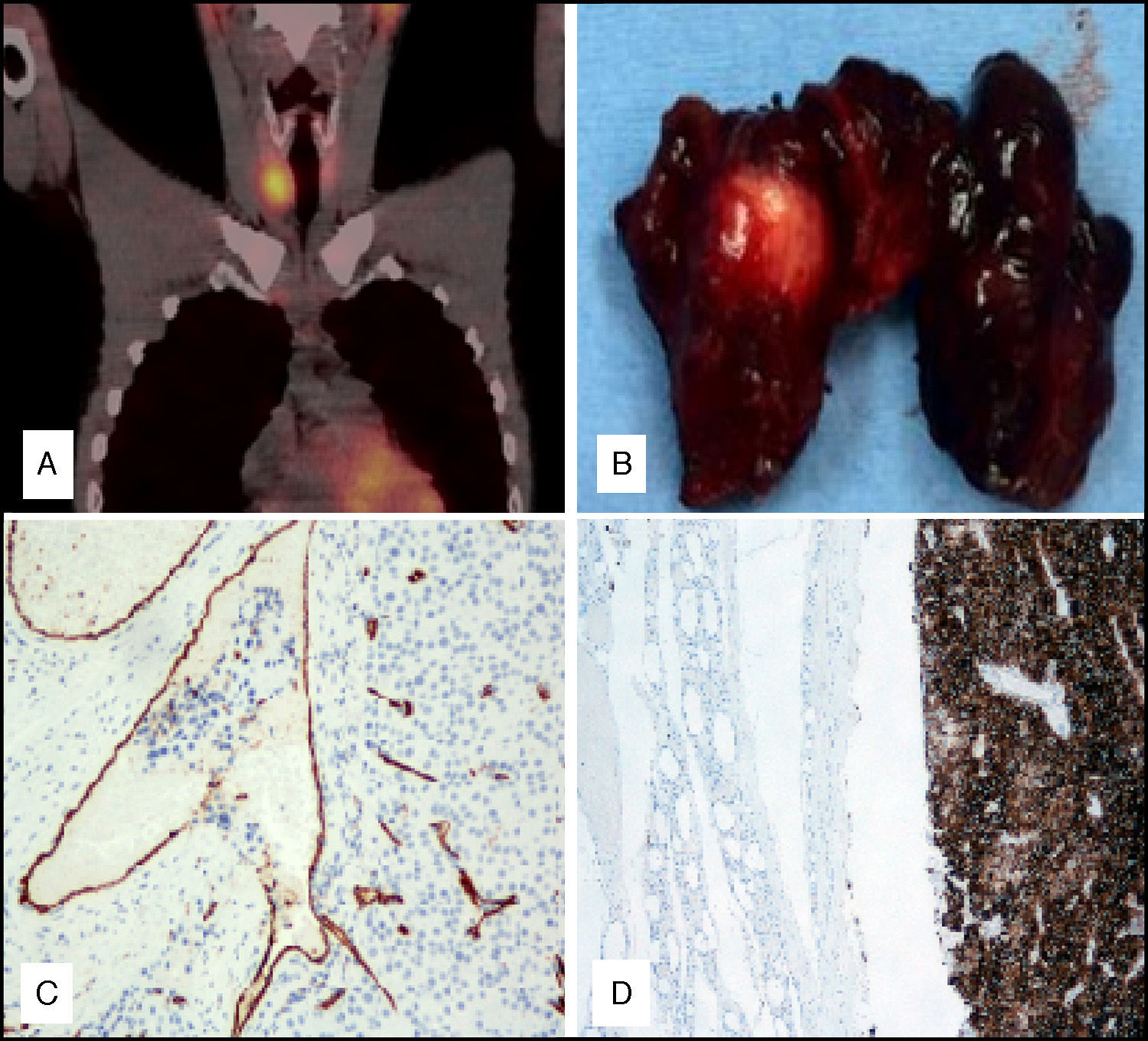
Neck ultrasonography showed a large nodule (25.03mm×21.63mm×34.24mm in size) in the lower pole of the right thyroid lobe which was isoechoic and had areas of cystic degeneration and colloid crystallization, with well-defined margins and peripheral vascularization. No adenopathies of a pathological appearance were seen on the side of the neck. Although the lesion was inside the thyroid gland, it had a lateral hypoechoic area, with apparent polar vascularization, which was punctured. Intratumoral PTH was measured and found to be elevated, and a parathyroid origin of the lesion was suspected. A cytological examination of fine needle aspiration revealed follicular thyroid proliferation suggesting a neoplasm, although a parathyroid follicular lesion could not be ruled out. Neck scintigraphy and SPECT-CT showed in the early phase good tracer uptake by the thyroid gland, with incomplete washout of activity in the late image, and a rounded hyperuptake focus site located in the right thyroid lobe, probably related to the suspected diagnosis of parathyroid gland disease (Fig. 1A).
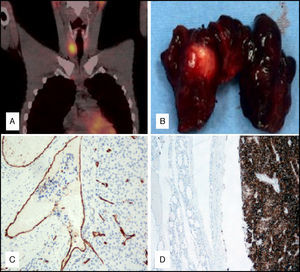
(A) SPECT-CT after the administration of technetium-99m: incomplete washout of uptake on late image. (B) Surgical specimen: right thyroid lobe with longitudinal dissection. (C) Immunohistochemistry for CD31 marking vascular endothelium. Tumor cell plaques entering the vessel. (D) Immunohistochemistry for PTH. Intrathyroid lesion: intensely positive tumor, in contrast to the negative result in the rest of the thyroid gland.
An exploratory cervicotomy revealed a whitish, well-defined intrathyroid nodule approximately 20mm in size (Fig. 1B). A right lower parathyroid gland was not identified; none of the other parathyroid glands showed any gross changes, and no adenopathies or infiltration of adjacent structures were seen either. The right thyroid lobe was resected, and peroperative PTH levels were measured before and after surgical resection, showing the expected decrease. The patient was symptom-free from the first day after surgery. Ca levels decreased to 9.6mg/dL and PTH levels to 64.3pg/dL, and he was therefore discharged. During monitoring, the patient showed transient hypoparathyroidism, which was managed with oral calcium and vitamin D until symptom relief and normalization of calcium and PTH levels were achieved.
Examination of the surgical specimen revealed a 35×28mm whitish brown nodule, homogeneous on sectioning, with a fleshy appearance. It had a double encapsulation area, as well as areas of minimal capsule infiltration and vascular invasion foci (Fig. 1C). The immunohistochemical profile included negative thyroglobulin, PTH and Ki67 of 20% (Fig. 1D). These findings were consistent with a giant intrathyroid PC of a mixed type, with chief cells and oncocytic cells. In the 16 months of follow-up to date, the patient has remained symptom-free, with no changes in ultrasonographic and laboratory monitoring.
There are criteria, such as the clinical manifestations (asthenia, pathological fractures, oliguria, renal stones, palpable mass, etc.) usually associated with high PTH and calcium levels, which suggest that primary hyperparathyroidism is the consequence of a PC.2 Nine cases of intrathyroid PC have been reported to date,1,3–11 most of them occurring in women with clinical characteristics similar to our case and with a high suspicion of carcinoma. In SPECT-CT, good tracer uptake by the thyroid gland in the early phase, with incomplete activity washout in the early image, makes it possible to differentiate the parathyroid origin of the lesion, even if this is inside the thyroid gland. Adequate localization was achieved in only two of the reported cases.1,3–10 An intrathyroid lesion may be smaller, but causes clinical and laboratory changes similar to extrathyroid lesions.11
PC should be treated with surgery. A conservative approach was used in most of the reported cases, with resection of the affected thyroid lobe only, as no radiographic or peroperative signs were seen of any invasion of adjacent structures or suspicious adenopathies.3–8,10 Metastatic disease occurred in a single case, and all patients showed normal calcium levels during follow-up. A diagnosis of carcinoma can only be confirmed by the final pathological examination of the specimen, which should find signs of vascular, capsular invasion, prominent nucleoli, and a high mitotic index, the findings made in the reported patient.1,3–10
The PC reported was unique because of its unusual location. No such case had previously been reported in Spain, which made diagnosis even more difficult because our well-grounded suspicion was not supported by the literature, and a more rigorous work-up of the patient was therefore required. Imaging studies are undoubtedly the current mainstay in endocrine surgery, but clinical experience and suspicion will continue to be indispensable for making a diagnosis which is correct, however unlikely it may appear.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Tejera Hernández AA, Gutiérrez Giner MI, Vega Benítez V, Fernández San Millan D, Hernández Hernández JR. Carcinoma paratiroideo intratiroideo. Descripción de un caso y revisión de la literatura. Endocrinol Nutr. 2016;63:46–48.