Pituitary adenomas account for approximately 15% of intracranial benign tumors. The neurosurgical results achieved since the endoscopic endonasal transsphenoidal (EET) approach was introduced in our center in 2005 are reported here.
Patients and methodsA retrospective analysis of 121 patients with sellar lesions (58% females, age 55.7±16 years, range 18–82) who underwent EET surgery from February 2005 to January 2012 and were followed up for a mean time of 4.58 years (range 1.08–8.58).
ResultsSix Rathke cleft cysts (3 intra-suprasellar, 1 intrasellar, 2 suprasellar); 114 pituitary adenomas (16 microadenomas, 98 macroadenomas), and 1 case of normal MRI were included. Baseline findings included hormonal changes in 59 patients (48.7%) and visual field changes in 38 patients (31%); in 7 patients (5.8%), clinical presentation was pituitary apoplexy. Complete resection was achieved in 77 patients (63.6%), subtotal resection in 29 (23.9%), and partial resection in 15 (12.3%). In patients with Grade 3 and 4 cavernous sinus invasion, resection was subtotal in 30% (12/39) and complete in 46% (18/39). Hormonal remission was achieved in 16 patients with Cushing disease (84%), 18 patients with prolactinoma (78.2%), and 18 patients with acromegaly (85.7%). There were 12 cases (9%) of cerebrospinal fluid leak, 4 cases of diabetes insipidus, and 3 cases with transient SIADH/hyponatremia. Seven patients developed panhypopituitarism. Postoperative mortality rate was 2.4%. One hundred and three patients (85.3%) were discharged from the hospital less than 48h after surgery.
ConclusionOur results are similar to those reported by renowned pituitary units. Results achieved using an endoscopic approach in pituitary neurosurgery are better than those of microneurosurgery for cavernous sinus invasion.
Los adenomas hipofisarios representan un 15% de los tumores intracraneales benignos. Presentamos los resultados quirúrgicos obtenidos desde la introducción en nuestro centro del abordaje endoscópico endonasal transesfenoidal (EET) en 2005.
Material y métodosAnálisis retrospectivo de 121 pacientes con lesiones intraselares (58% mujeres; edad 55,7+/–16 años, rango 18-82) tratados mediante EET desde febrero del 2005 hasta enero del 2012, seguidos en promedio 4,58 años (rango 1,08-8,58).
ResultadosIncluimos 6 quistes de Rathke (3 intrasuprasellares, uno intrasellar y 2 suprasellares); 114 adenomas hipofisarios (16 microadenomas, 98 macroadenomas) y un caso con RMN normal. Los hallazgos basales incluían alteraciones hormonales en 59 pacientes (48,7%), seguidas de alteraciones del campo visual en 38 pacientes (31%); en 7 (5,8%) la presentación clínica fue una apoplejía hipofisaria. Logramos la resección completa en 77 casos (63,6%), subtotal en 29 (23,9%) y parcial en 15 (12,3%). En los pacientes con invasión de seno cavernoso de grado 3 y 4 la resección fue subtotal en 30% (12/39) y completa en 46% (18/39). Se obtuvo remisión hormonal en 16 pacientes con enfermedad de Cushing (84%), en 18 con prolactinoma (78,2%) y en 23 con acromegalia (89%). Hubo 12 casos (9%) de fístula de líquido cefalorraquídeo, 4 casos de diabetes insípida y 3 de SIADH/hiponatremia transitorias. Siete pacientes desarrollaron panhipopituitarismo. La tasa de mortalidad posquirúrgica fue de 2,4%. Ciento tres (85,3%) pacientes permanecieron ingresados menos de 48 horas tras la cirugía.
ConclusiónNuestros resultados son comparables con los de prestigiosos centros de referencia en patología hipofisaria; los resultados obtenidos mediante abordaje endoscópico en la neurocirugía hipofisaria son superiores a los de la microneurocirugía cuando existe invasión del seno cavenoso.
Pituitary tumors, usually benign, are the most common condition in the sellar region, account for approximately 15% of benign tumors, and are incidentally found in 5–20% of cases.1 Rathke cleft cysts, usually asymptomatic, may expand and cause compression symptoms such as campimetric defects or hormone changes, in which case they are amenable to surgery.2,3
The treatment of choice of many such lesions is surgery. The surgical approach, initially transcranial, has greatly evolved, first to the transsphenoidal microscopic and finally to the endonasal endoscopic transsphenoidal (EET) approach.
Current endoscopes are based on the design of Harold H. Hopkins in the 50s. In the 90s, endoscopes started to be used in the endonasal approach to nasosinusal pathology, and also as an auxiliary tool to the surgical microscope used in neurosurgery. Jho and Carrau reported in 1997 a series of 50 patients operated on by the endonasal endoscopic route with very good results.4
Advantages of the EET approach over the microscopic approach include shorter operating time and hospital stay. At our hospital, as in other hospitals experienced in the EET approach, this is the preferred route for treatment of sellar and parasellar tumors.5,6
The purpose of this article is to report the experience in surgical treatment of lesions in the sellar region using the EET approach at Hospital Clínico y Provincial in Barcelona, and to discuss its clinical and hormonal results and complications. The experience of a single neurosurgeon (J.E.) is reported, in accordance with most international consensuses.
Patients and methodsA retrospective, descriptive study was conducted of patients with sellar lesions who underwent surgery using an EET approach at Hospital Clínico y Provincial in Barcelona from February 2005 to January 2012. Exclusion criteria included all cases where the approach was extended to the cranial base and inflammatory or metastatic lesions, as well as craniopharyngiomas and other tumor lines because of their different prognosis. Patients followed up for less than one year were also excluded, except for those who died in the perioperative period. A total of 121 patients with a mean follow-up time of 4.58 years (range 1.08–8.58) were included.
Diagnosis and preoperative studiesClinical presentation and radiographic and endocrine findings were assessed in all patients. A differentiation was made between patients with acute or subacute (pituitary apoplexy) clinical onset and those with more insidious neurological and/or endocrine symptoms. SITA 24-2 computed campimetry was performed in all patients to define the degree of visual field involvement. From the endocrine viewpoint, integrity of the hypothalamic–pituitary axis was first assessed by measuring basal plasma levels of FSH, LH, ACTH, cortisol, IGF-1, prolactin, TSH, free T4, estradiol (females), and testosterone (males) using the standard laboratory tests at the hospital. Potential hypersecretion was also assessed, when suspected based on clinical data, using the diagnostic procedures recommended for each hypersecretion syndrome, including catheterization of inferior petrosal sinuses for differential diagnosis from an ectopic origin of ACTH in some selected cases of Cushing's disease.7
All patients were performed thin-slice (2mm) 1.5-Tesla MRI. In patients in whom the lesion could not be differentiated from the adjacent pituitary parenchyma, dynamic MRI of the pituitary gland was performed.
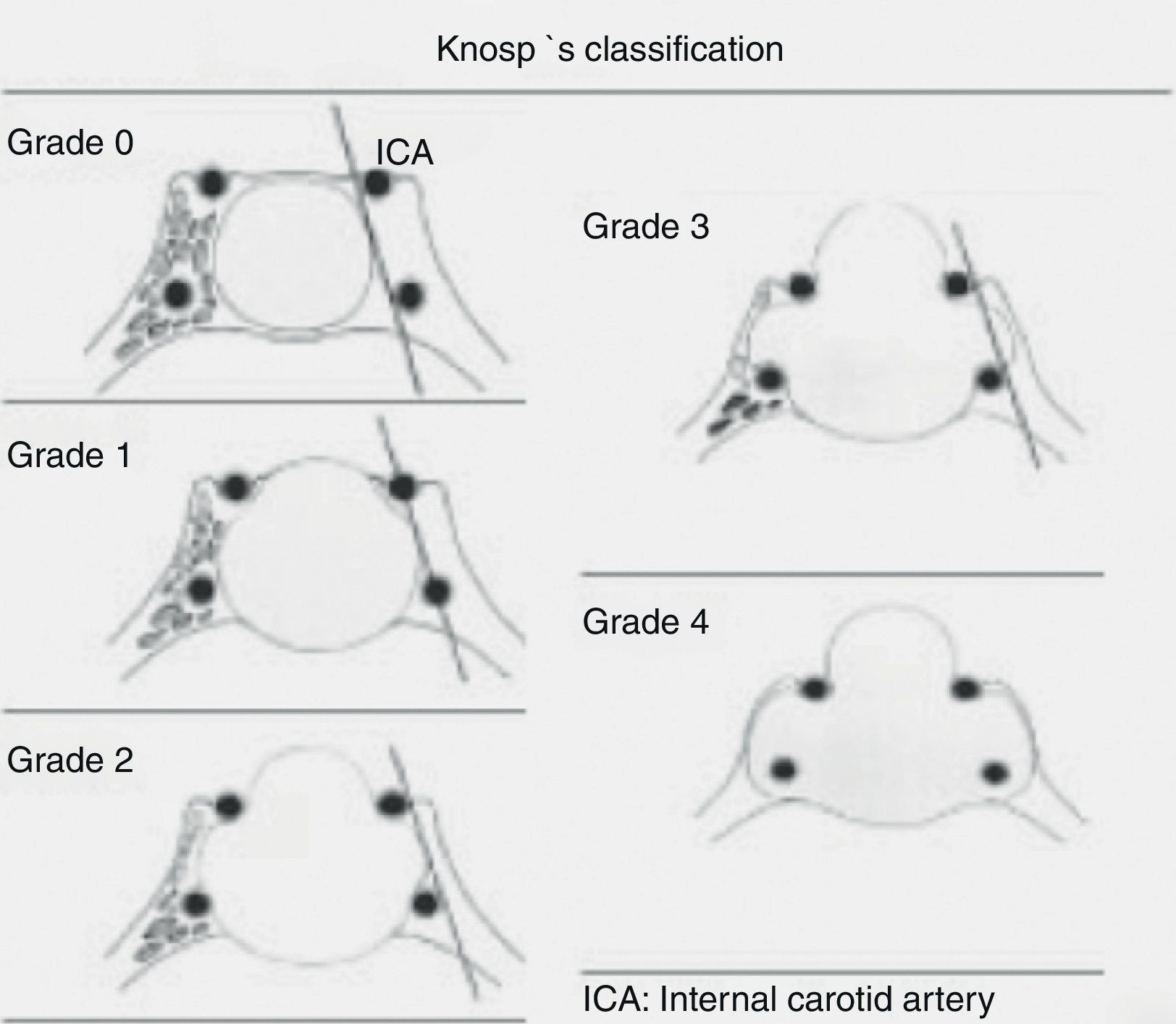
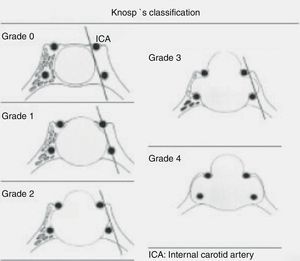
Lesions were classified based on preoperative images as (1) Rathke cleft cysts and (2) pituitary adenomas. Rathke cleft cysts were categorized as intrasellar, suprasellar, and intrasuprasellar based on their relationship to sellar diaphragm. Adenomas were divided into microadenomas and macroadenomas based on their size (≤1cm or >1cm). Macroadenomas were categorized by their extension within the cavernous sinus according to Knosp's classification (Fig. 1) due to its relationship to prognosis of recurrence.8,9
SurgeryAn EET approach not involving resection of any nasal structure, only lateralization of middle turbinate, was performed.10 A neuronavigator was used for repeat surgeries. The resected material was sent to the pathological laboratory for standard histological and immunohistochemical study.
Postoperative managementThe clinical, radiographic, and hormonal parameters assessed at baseline were re-evaluated in all patients. The first assessment was done three months after hospital discharge, and repeat assessments were performed every year thereafter. Based on the findings of the postoperative MRI performed in the last clinical and radiographic control, tumor resection was classified in the following categories: (1) complete resection: no visible tumor remnants in the control MRI; (2) subtotal resection: resection of more than 90% of the initial tumor; and (3) partial resection: resection of less than 90% of tumor volume. Clinically, patients with campimetric deficit were grouped into three categories: (1) clinical signs of patient worsened after surgery; (2) there were no changes; and (3) preoperative clinical signs improved.
Hormonal cure criteria for secreting tumors, assessed at three months, included:
- -
Acromegaly: GH level less than 1ng/dL after oral glucose tolerance test (OGTT) and IGF-1 level normal for age.
- -
Prolactinoma: PRL <30ng/dL in females and <15ng/dL in males.
- -
Cushing's disease: presence of adrenal insufficiency (basal plasma cortisol level <2ng/dL in the morning) or normalization of hypercortisolism (normal urinary free cortisol and/or salivary cortisol 0h and plasma cortisol suppression to <2ng/dL after dexamethasone 1mg, or 0.5mg/6h 48h).
A total of 121 patients were included, 70 females (58%) and 51 males (42%) with a mean age of 55.7 years (range, 18–82 years).
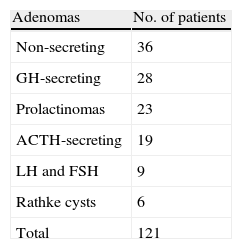
Preoperative findingsPreoperative image: 6 Rathke cysts (3 intrasuprasellar, one intrasellar, and 2 suprasellar) and 114 pituitary adenomas (16 microadenomas and 98 macroadenomas), subclassified as follows: Knosp grade 0, 41 cases; Knosp grade 1, 5 cases; Knosp grade 2, 13 cases; Knosp grade 3, 18 cases; and Knosp grade 4, 21 cases. MRI was normal in a patient with Cushing's disease, in whom diagnosis was made by catheterization of inferior petrosal sinuses.
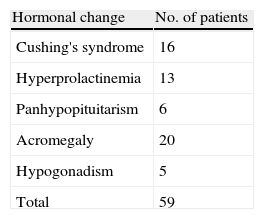
Clinical presentation: Hormone changes with specific manifestations of hormonal hyperfunction or hypofunction were overall the most common clinical presentation in our series, occurring in 59 patients (48.9%) (Table 1). Prolactinomas included were cases resistant or intolerant to dopaminergic treatment. Campimetric changes were seen in 38 patients (31%). Seven cases of pituitary apoplexy started with a sudden change in at least one cranial nerve associated to hormone insufficiency. Six patients with non-specific symptoms were incidentally diagnosed. The initial manifestation of Rathke cysts was a campimetric defect in one patient, headache in two patients, and hormone changes in the remaining three patients.
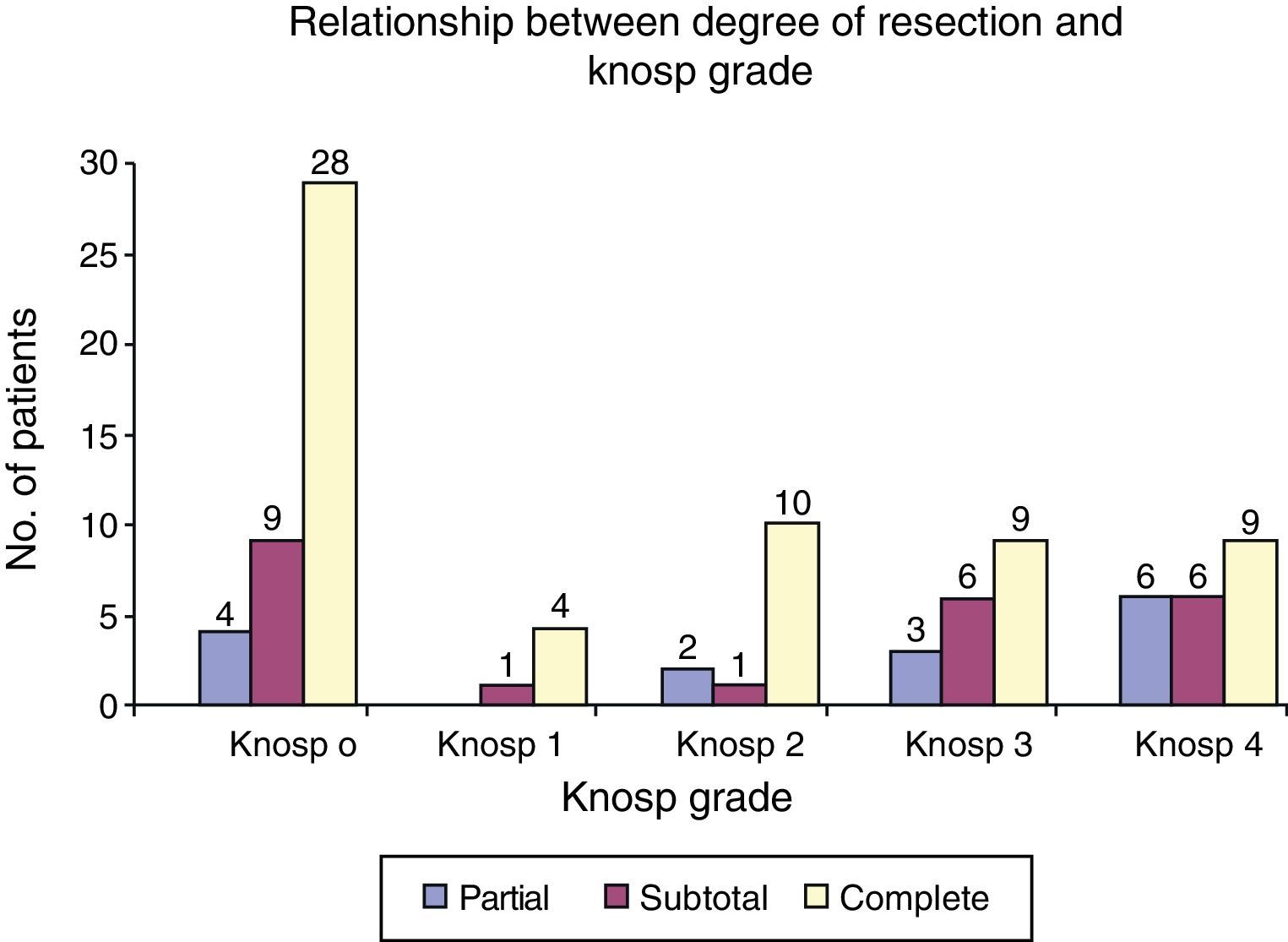
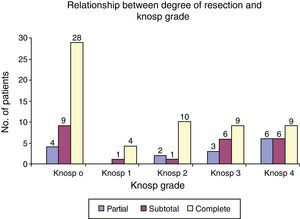
Results of surgeryDegree of surgical resection: overall, complete resection was achieved in 77 patients (63.6%), subtotal resection in 29 (23.9%), and partial resection in 15 (12.3%). Tumor resection greater than 90% was achieved in 88% of patients. As regards degree of resection as a function of cavernous sinus invasion, in patients with maximum cavernous sinus invasion (Grades 3 and 4), subtotal resection was achieved in 46% (18/39), and complete resection in 46% (18/39). In tumors with little invasiveness of the cavernous sinus (Grades 1 and 2), complete resection was achieved in 77% of cases (Fig. 2).
Pathological results: according to the histological and immunohistochemical study, non-secreting tumors were most common (36 cases), followed by tumors secreting growth hormone, prolactin, and ACTH (Table 2). Tumors secreting gonadotropins (LH and FSH) and seven tumors positive for GH according to immunohistochemical data had non-secreting clinical behavior. Some tumors secreting GH, PRL, and ACTH were also not identified at the preoperative study.
ComplicationsTwo patients died from pulmonary thromboembolism (PTE) and ischemic stroke. The first patient experienced hospital-acquired pneumonia followed by PTE. The second patient, with history of stroke on antiplatelet aggregation therapy and who had to be excluded from surgery, experienced basilar artery thrombosis. CSF leak occurred in 12 patients (9%). Two of these patients experienced meningitis and showed a good response after antibiotic therapy and fistula management. One patient had a carotid-cavernous fistula that required endovascular treatment, and another patient was found to have a surgical bed hematoma with no clinical consequences.
Seven patients (5.7%) were found panhypopituitarism requiring hormone replacement therapy. These deficiencies were already present before surgery in two of these patients, while another four patients had partial deficiencies which became complete. Diabetes insipidus and transient SIADH/hyponatremia were found in four and three patients respectively.
Hospital stay: 103 patients remained at the hospital less than 48h after surgery, 11 patients from 2 to 10 days, and 7 patients more than 10 days.
Change over time in visual field: among the 38 patients with prior campimetric deficit, 21 (55%) experienced complete remission, 14 (37%) showed no improvement, and the campimetric deficit worsened in the first year of follow-up in three patients.
Results in each tumor subtype- -
Non-secreting adenomas: this group includes the nine patients with immunohistochemical diagnosis of adenoma secreting LH-FSH clinically behaving as non-secreting tumors and the seven patients with immunohistochemical diagnosis of GH secretion but no clinical manifestations of acromegaly. Resection was complete in 31 patients (65%), subtotal in 17 (37.7%), and partial in 4 (8.8%) patients. Fifty-four percent of patients experienced complete improvement of visual deficits, while the remaining patients had partial or no improvement. Three patients developed panhypopituitarism, which was definitive in two and transient in one who experienced hypogonadism, and another four patients developed transient hypothyroidism.
- -
Acromegaly: 18 of the 21 patients (85.7%) experienced remission. Of the three patients who continued to show hormone activity, one underwent repeat surgery and the other two were given radiotherapy.
- -
Prolactinomas: prolactin levels normalized in 18 of the 23 cases (78.2%). Hyperprolactinemia persisted in five patients, two of whom underwent repeat surgery (one of them two times). Hyperprolactinemia was not resolved, and these patients therefore continue to be treated with dopamine agonists.
- -
Cushing's disease: hypercortisolism was resolved in 16 of the 19 patients (84%). Two of these patients experienced transient adrenal insufficiency, and another two suffered permanent panhypopituitarism. The remaining three patients continued to have active Cushing's disease and required other treatment modalities.
- -
Rathke cysts: complete resection and symptom improvement were achieved in five of the six patients (83.3%). The remaining patient, a woman with severe restrictive lung disease, experienced in the postoperative period hospital-acquired pneumonia followed by lung thromboembolism, which resulted in death. No follow-up allowing for assessment of degree of resection is available.
This study portrayed our experience and depicted results with surgery of pituitary lesions using a simple endoscopic transsphenoidal approach.
According to international consensus on the treatment of acromegaly, the term surgical experience is defined as publication of the results achieved and adequate clinical and laboratory follow-up in at least 100 cases, and performance of at least 25 surgical procedures in the pituitary gland per year.11 We think that these requirements may be extended to all pituitary tumors. Our group performed 121 simple surgeries in the sellar region by EET, excluding extended approaches and simple approaches for inflammatory or metastatic diseases or tumor of other cell lines.
The term cure is avoided in result evaluation because this is a difficult to define situation that cannot be established without a follow-up time which is not established either and involves a dichotomous categorization that prevents evaluation of intermediate results, also beneficial for patients. In the specific case of secreting adenomas, it is known that the longer the follow-up time, the higher the number of recurrences. Thus, a longer follow-up period is needed to ascertain the final outcome of surgery in terms of secretion control.
In our series, complete lesion resection based on radiographic criteria was achieved in 77 (63.6%) patients, while subtotal resection was achieved in 29 (23.9%) patients and partial resection in 15 (12.3%) patients. Gondim et al. achieved complete resection in 38% and partial resection in 18% of patients. In this series, Knosp grade ≥3 was associated to greater probability of subtotal resection.12 Koutourousiou et al. reported resections greater than 90% (subtotal) in 66% of 55 patients with giant adenomas.13 Cavallo, Cappabianca, and di Maio achieved complete resection rates of approximately 60% in all their series.14–17
The inverse relationship seen between the tumor resection achieved and Knosp grades, which may undoubtedly be attributed to the greater technical difficulty associated to cavernous sinus involvement, should be emphasized. One of the major advantages of the endoscopic procedure over microsurgery is the possibility to better explore cavernous sinuses. This is reflected in our series, where greater than 90% tumor resections (partial 30%, complete 40%) were achieved in 76.9% of patients with lesions with high cavernous sinus invasiveness (grades 3 and 4). A comparison with other microsurgical series, such as the Knosp et al. series, shows that no complete resection was achieved by these authors in grade 4 tumors.9
Non-secreting adenomas were the most common cause of campimetric changes in our series. An essential objective of surgery is resolution of such changes, which was fully achieved in 54% of cases. Partial improvement or stability was achieved in all other patients. Paluzzi et al. reported 237 patients, 80% of which experienced complete or partial improvement in visual symptoms irrespective of adenoma subtype.18 In the Robenshtok et al. series of 105 patients, visual defect improvement occurred in 74%.19 Since the postoperative control image shows a resection greater than 90% in 93% of patients with non-secreting macroadenomas, we think that time since tumor onset and development of an irreversible optic nerve lesion possibly explain that visual deficit recovery is only complete in a little over half the cases.
Losa et al. advocate surgery as treatment for incidentalomas in all cases.20 Gamma knife radiosurgery (GKR) is another treatment alternative, and is especially indicated in some cases of recurrence or when surgery is contraindicated. In a multicenter study on 512 patients with non-secreting adenomas treated in a second time with GKR, Sheehan et al. reported late hypopituitarism in 21% and cranial nerve changes in 9%. Thus, GKR is not a noninvasive procedure, and should be reserved for highly selected cases not amenable to surgery.21
Surgery is the treatment of choice for acromegaly. In patients with persistently high postoperative IGF-1 levels and with no evidence of residual lesion in control MRI, late improvement and normalization of IGF-1 levels may occur in up to 59% of cases at three months, and in an additional 24% in the 12–57 months after surgery. In our series, normalization of IGF-1 and GH levels occurred during follow-up in 85.7% of patients.22 According to the Spanish Acromegaly Register, 81.2% of patients were treated with surgery, with a 40.3% cure rate, while only 28% of irradiated patients achieved cure.23,24 The high remission rate in our series may possibly be due to our good results in tumors with significant grades of cavernous sinus invasion, which we attribute to the EET approach.
In management of prolactinoma, the most common pituitary tumor, surgery is only indicated in selected patients who want to become pregnant, are intolerant or resistant to treatment with dopamine agonists, or have visual deficits or tumors greater than 20mm. It is also indicated in young patients with a great probability of complete resection using transsphenoidal surgery and who do not want to take medication for a long time.25,26 Partial resection also has the potential benefit of allowing for control of hyperprolactinemia with lower doses of dopamine agonists.26 Ikeda et al. recently reported an 89% success rate of surgery during long-term follow-up in a series of 138 prolactinomas in women who wanted to become pregnant.27 In our series, prolactin normalization was achieved in 78.2% of the 23 patients. One patient underwent surgery due to pituitary apoplexy causing sudden headache and cranial nerve changes.
The high risk of bleeding from these adenomas as an incidental finding is also known. There are studies reporting prevalence rates of 6.8% in pituitary adenomas and greater than 20.3% in prolactinomas. Our series included seven cases of pituitary apoplexy, of which only one occurred in a prolactinoma and ACTH-secreting adenomas were most common.
Diagnosis and treatment of Cushing's disease represent a real challenge. According to the literature, transsphenoidal surgery achieves adequate disease control in 65–90% of microadenomas. Success rates are somewhat lower in macroadenomas, with greater chance of infiltration when lesions are greater than 20mm. Results of our series agree with those reported in the literature, with short-term control in 84% of cases. Various series have reported use of the EET approach. Prevedello et al. reported 88% remission in a series of 167 patients. Intraoperative adenoma identification was associated to better results.28 Dickerman et al. reported 72% remission, while Starke et al. found remission in 95% of 65 patients.29,30
In Rathke cleft cysts, the primary objective of surgery is to resolve compression symptoms. If endocrine function is normal and extrasellar structures are not compressed, follow-up may be decided with no risk. The Aho et al. series, one of the largest reported, included 118 patients and reported complete resection in 97%, improvement in prior hormonal clinical signs in 18%, and improvement in prior visual clinical signs in 98%, but with almost 20% ID and 18% recurrence.31 Higgins et al. reported 61 patients who underwent transsphenoidal surgery, 32 with complete resection and 29 with partial resection/decompression. They found no differences between the procedures in repeat surgery rate, but the complication rate was 34% in patients with complete resection (diabetes insipidus and CSR leak) and only 10% in those with partial resection/decompression.32 Several studies recommend decompression instead of resection surgery, arguing that similar results are achieved and that complications are more common with the latter procedure. However, Madhok et al. reported 35 patients with complete resection in 100% and no postoperative complications, and two patients with radiographic recurrence not requiring repeat surgery.3 In our series, including very few patients with this condition, resolution was achieved in all patients but one, who died from a respiratory complication. No patient required surgery for a recurrence (lesion growth and symptoms re-occurrence). As regards hormonal results, transient diabetes insipidus and hypothyroidism occurred in one patient each, and were followed by complete recovery.
ConclusionThe results achieved in our series using endonasal endoscopic surgery were similar to the best results currently achieved with pituitary surgery. Interdisciplinary management and use of a single neurosurgeon to treat these conditions are essential for adequate management. The endoscopic procedure provides for a better resection in tumors with cavernous sinus invasion.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Torales J, Halperin I, Hanzu F, Mora M, Alobid I, De Notaris M, et al. Cirugía endoscópica endonasal en tumores de hipófisis. Resultados en una serie de 121 casos operados en un mismo centro y por un mismo neurocirujano. Endocrinol Nutr. 2014;61:410–416.