Communication failures may result in inadequate treatment and patient harm, and are among the most common causes of sentinel events. Checklists are part of cycles to improve quality of the care process, promote communication between professionals involved in the different stages, help detect failures and risks, and increase patient safety. The lack of checklists at each stage was identified as a factor contributing to communication failures.
ObjectiveTo design checklists at different stages of the thyroidectomy care process to improve the communication between the professionals involved.
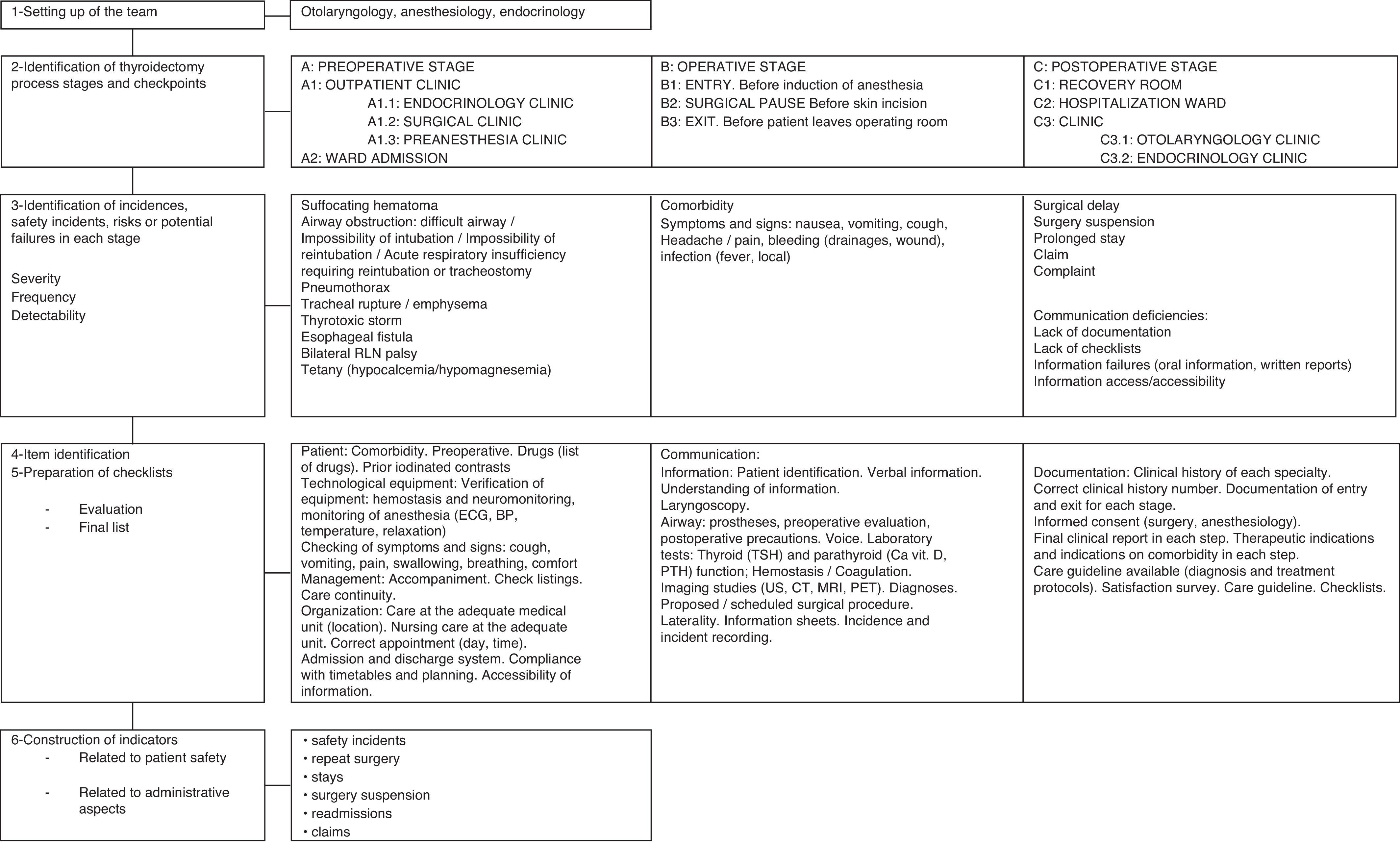
MethodMultidisciplinary working team consisting of specialists in otolaryngology, anesthesiology, and endocrinology. The process of thyroidectomy was divided into three stages (preoperative –A–, operative –B– and postoperative –C–). Potential safety incidents and failures at each stage and their contributing factors (causes) were identified by the literature review and brainstorming. Checklists for each checkpoint were designed by consensus of the working group.
ResultsThe items correspond to factors contributing to the occurrence of incidents in the perioperative stage of thyroidectomy related to patients, technological equipment, environment, management, and organization. Lists of items should be checked by the appropriate specialist in each stage.
ConclusionsChecklists in thyroid surgery are tools that allow for testing at different checkpoints data related to factors contributing to the occurrence of failures at each stage of the care process.
Los fallos en la comunicación pueden provocar tratamiento inadecuado, daño al paciente y son una de las causas más frecuentes de aparición de eventos centinela. Las listas de verificación son herramientas que forman parte de los ciclos de mejora de la calidad del proceso asistencial, facilitan la comunicación entre los profesionales implicados, ayudan en la detección de fallos y riesgos e incrementan la seguridad del paciente. La falta de listados de verificación en cada etapa es un factor contribuyente en los fallos de comunicación.
ObjetivoDiseñar listas de verificación en distintas etapas del proceso asistencial de tiroidectomía para mejorar la comunicación entre los profesionales implicados.
MétodoEquipo de trabajo multidisciplinar constituido por especialistas en otorrinolaringología, anestesiología y endocrinología. El proceso de tiroidectomía se distribuyó en 3 etapas (preoperatoria [A], operatoria [B] y postoperatoria [C]). Se identificaron los posibles incidentes de seguridad y fallos en cada etapa y sus factores contribuyentes (causas) mediante revisión bibliográfica y tormenta de ideas. Se diseñaron listados de verificación para cada punto de control mediante consenso del grupo de trabajo.
ResultadosLos ítems se corresponden con factores contribuyentes en la presentación de incidentes perioperatorios en tiroidectomía relacionados con el paciente, los equipos tecnológicos, el entorno, la gestión y la organización.
ConclusionesLas listas de verificación en cirugía tiroidea son herramientas que permiten comprobar de forma reiterativa en distintos puntos de control del proceso de tiroidectomía datos que se relacionan con factores contribuyentes en la presentación de fallos en cada etapa del proceso asistencial.
The most common incidents after thyroid surgery include hypocalcemia (transient 15.5–19.5%1; permanent from 0–0.3%1 to 4.8%2), recurrent laryngeal nerve palsy (transient, 1.8–2.1%1; permanent, from 0–0.2%1 to 5.1%3), bleeding (0.5–0.9%),1 and airway obstruction.4 Overall mortality of thyroidectomy is however 46–64%,1 and is associated to multiple factors which have been investigated without reaching definitive conclusions.5 Treatment should therefore be aimed at improving several aspects from the preoperative period.6
The safety incident is the event or circumstance which caused or could have caused an unnecessary damage to the patient7; includes the concept of sentinel event (unexpected adverse event related to death, physical or psychological damage or risk of damage8). Thus, safety incidents result in actual or potential patient damage, use of treatments and care unusual for the procedure (increased care level, need for additional procedures and treatments), prolonged stay, inadequate stay, readmission, suspension of surgical programming, and increased cost.8–10
Complexity and greater instrumentation of care probably influence the occurrence of incidents.11 Safety incidents usually have multiple causes (system or individual failures12) and should be investigated using root cause analysis (RCA) and Healthcare Failure Mode Effects and Analysis (HFMEA).9,13 HFMEA assesses the criticality (frequency and severity) and detectability of each potential failure.9
The number of incidents related to health care has been estimated to range from 2.9% and 16.6%, and that 27.4% to 51.1% of them would be avoidable.14 Complications occur in 3–16% of surgical procedures requiring admission, leading to mortality or permanent disability rates of 0.4–0.8%. It is thought that such complications could be prevented in at least half the cases.15,16 In Spain, adverse events are avoidable in up to 42.8% of cases and occur in 9.3% of inpatients for reasons attributable to care, being 1.6 times more common in patients with risk factors and up to 2.5 times more common in patients over 65 years of age.10 Comorbidity has an impact on incident occurrence, stay, and cost.17 Assessment of comorbidity before surgery allows for evaluating the preoperative risk of morbidity and mortality based on individual risk factors,17–19 but does not consider other contributing factors (equipment, environment, management, etc.). Several scales should therefore be used20 and interpreted with caution, as no gold standard is available.21
There are various models which attempt to explain and analyze the causes of safety incidents.22,23 Clinical risk management systems allow for a systematic solution of problems, contributing to improve the quality and safety of medical action by preventing adverse events, identifying the conditions that expose patients to risk, and preventing or controlling such risk, involving several organizational levels.13,24 This “implies practicing health care free from avoidable damages”, which “involves development of systems and processes aimed at reducing the probability of occurrence of system failures and personal errors and at increasing the probability to detect them when they occur and to mitigate their consequences”.25 The safety system allows for establishing criteria to decrease risk of recurrence, which would increase the possibility of serious adverse outcomes.7,9
Communication of information from a healthcare professional to another is one of the nine solutions to improve patient safety proposed by the Joint Commission, because “communication gaps may cause serious interruption in care continuity, inadequate treatment, and potential damage to the patient”, and has been reported to be one of the most common causes of the occurrence of sentinel events.26
Checklists (CLs) are tools including a systematic sequence of events related to the care process27 intended to consolidate safety practices and to promote communication and teamwork between several clinical disciplines.15
In this regard, use of the “surgical safety checklist” has allowed for decreasing the morbidity (from 11% to 7%) and mortality (from 6.2% to 3.4%) associated to surgery.15,16 However, the World Health Organization (WHO) guidelines for surgical safety are unevenly applied, even in the most advanced environments.15
Adequate communication benefits professionals and patients, but there is no universally accepted model to transmit perioperative critical information in thyroid surgery based on a rational approach.28
The purpose of this study was to design CLs for different stages of the thyroidectomy care process in order to improve communication between the professionals involved.
Materials and methodsTo develop the CL, the methodology proposed by Stufflebeam,29 summarized in the following points, was used:
- (1)
Setting up of the multidisciplinary work team, consisting of specialists in otolaryngology, anesthesiology, and endocrinology.
- (2)
Identification of the critical stages in the thyroidectomy process: preoperative (A), operative (B), and postoperative (C). In each stage, checkpoints were identified in a logical sequential order.27
- (3)
Identification of incidences, safety incidents, risks, and potential failures in each stage. Safety incidents were defined as those related to sentinel events, any other safety incident, quality indicator failures, incidents recorded in the medical or nursing clinical history, adverse effects of drugs, and patient complaints or claims.9,12 HFMEA methodology8,9 was used to select potential failures. The risk matrix was created based on frequency (incidence at our center and in the reviewed literature), severity (impact on the patient12), and detectability (difficulty to detect the risk or situations preceding the failure). Incidents of very high severity (catastrophic), undetectable (or difficult to detect) incidents, or highly critical incidents (severity by frequency product) were prioritized.8,9
- (4)
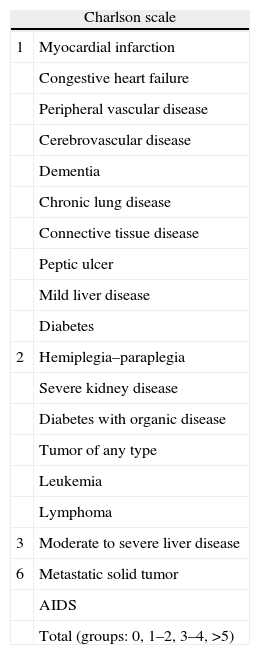
Item identification. Items related to safety incidents and failures in each stage, as well as contributing factors (causes), were selected by brainstorming adapting the taxonomy used in the literature reviewed.7,9,12 The lack of CLs in each stage was identified as a factor contributing to communication failures. Evaluation of comorbidity in the preoperative period was included using the Charlson and Elixhauser scales18,19 (Table 1). The operative period included the WHO listing.15
Table 1.Recording of comorbidity. Charlson and Elixhauser scales.
Charlson scale 1 Myocardial infarction Congestive heart failure Peripheral vascular disease Cerebrovascular disease Dementia Chronic lung disease Connective tissue disease Peptic ulcer Mild liver disease Diabetes 2 Hemiplegia–paraplegia Severe kidney disease Diabetes with organic disease Tumor of any type Leukemia Lymphoma 3 Moderate to severe liver disease 6 Metastatic solid tumor AIDS Total (groups: 0, 1–2, 3–4, >5) Elixhauser scale 1. Congestive heart failure 2. Cardiac arrhythmia 3. Heart valve disease 4. Lung circulation disease 5. Peripheral vascular disease 6. High blood pressure 7. Paralysis 8. Other neurological diseases 9. Chronic lung disease 10. Uncomplicated diabetes 11. Complicated diabetes 12. Hypothyroidism 13. Kidney failure 14. Liver disease 15. Peptic ulcer without bleeding 16. HIV disease 17. Lymphoma 18. Metastatic cancer 19. Solid tumor with no metastasis 20. Rheumatoid arthritis or vascular collagen disease 21. Coagulopathy 22. Obesity 23. Weight loss 24. Fluid and body electrolyte impairment 25. Anemia from blood loss 26. Anemia from other deficiencies 27. Alcoholism 28. Drug abuse 29. Psychosis 30. Depression - (5)
CL preparation Items for each process stage were ranked by consensus of the work group. A first review of CL contents was done to verify all items, checkpoints, and CL availability, and to assess the mean time needed to verify each point (2min, 95% CI: 1.14–2.86min).
Fig. 1 summarizes the methodology used for designing CLs.
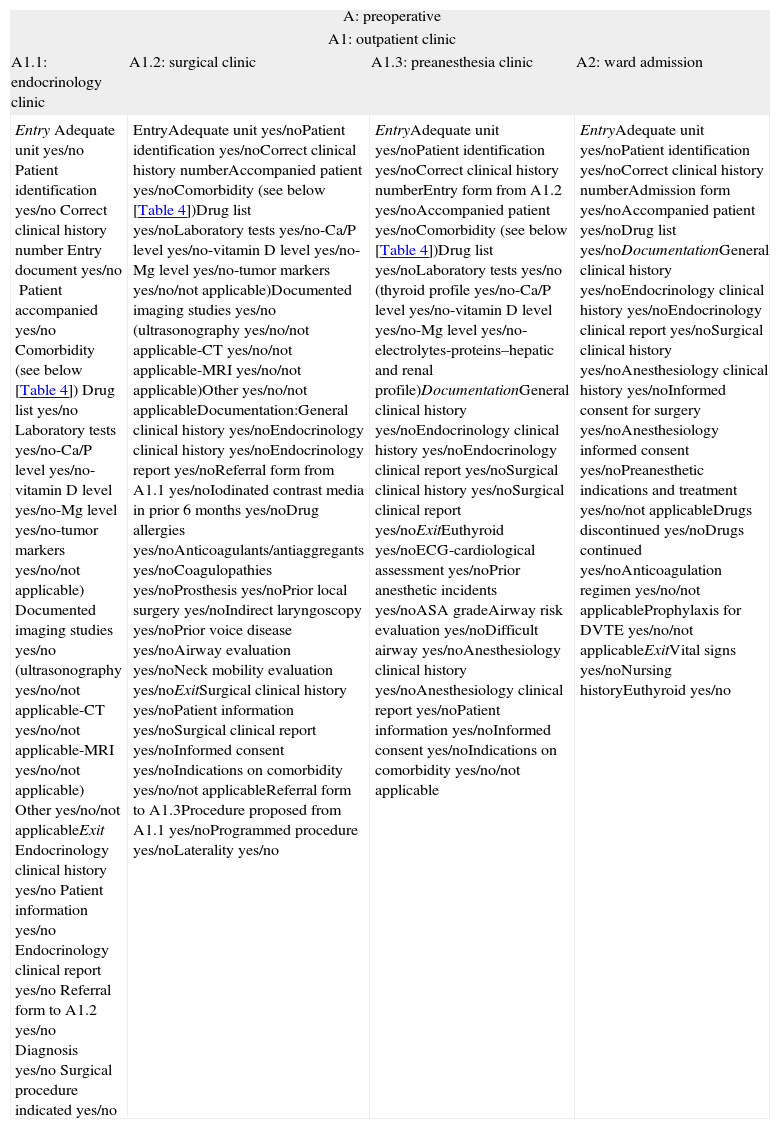
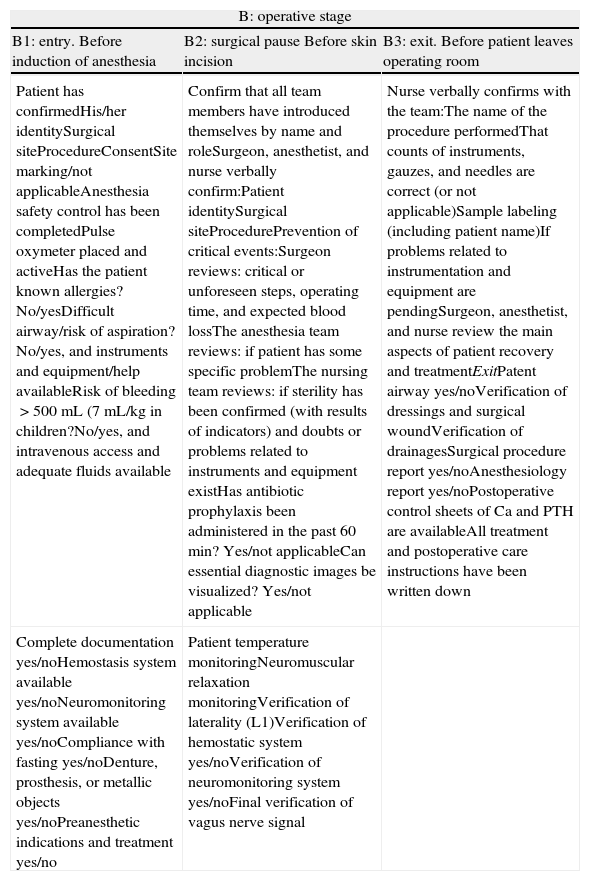
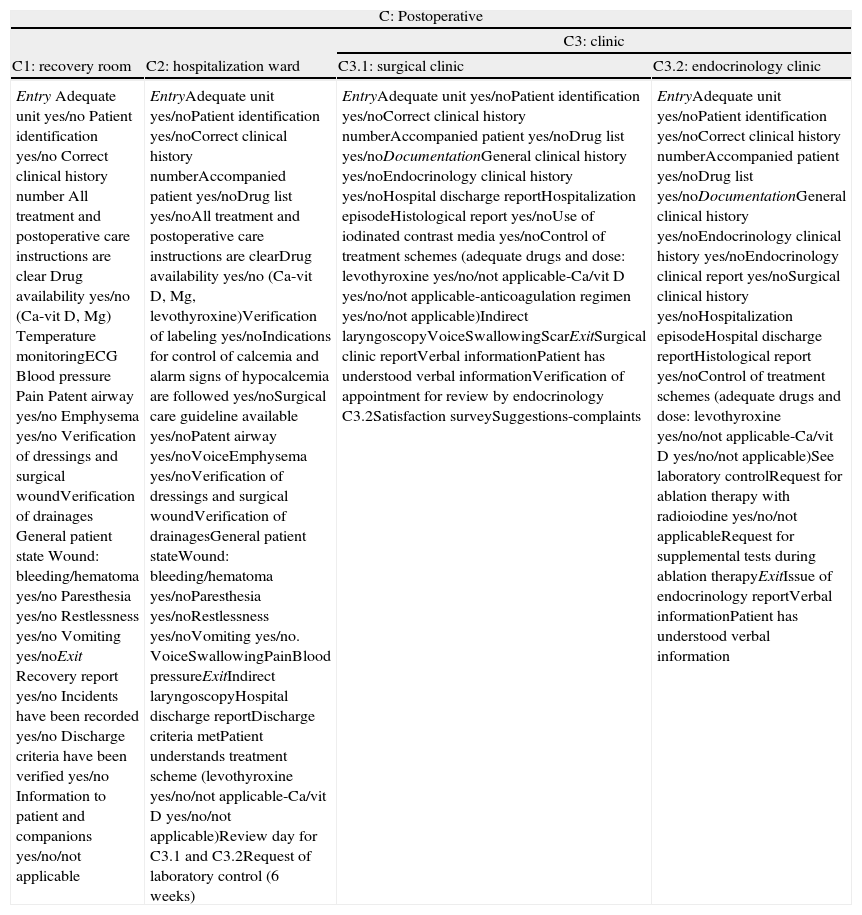
ResultsCLs are shown in Tables 2–4.
Checklists in thyroidectomy. Perioperative stage (A).
| A: preoperative | |||
| A1: outpatient clinic | |||
| A1.1: endocrinology clinic | A1.2: surgical clinic | A1.3: preanesthesia clinic | A2: ward admission |
| EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberEntry document yes/noPatient accompanied yes/noComorbidity (see below [Table 4])Drug list yes/noLaboratory tests yes/no-Ca/P level yes/no-vitamin D level yes/no-Mg level yes/no-tumor markers yes/no/not applicable)Documented imaging studies yes/no (ultrasonography yes/no/not applicable-CT yes/no/not applicable-MRI yes/no/not applicable)Other yes/no/not applicableExitEndocrinology clinical history yes/noPatient information yes/noEndocrinology clinical report yes/noReferral form to A1.2 yes/noDiagnosis yes/noSurgical procedure indicated yes/no | EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberAccompanied patient yes/noComorbidity (see below [Table 4])Drug list yes/noLaboratory tests yes/no-Ca/P level yes/no-vitamin D level yes/no-Mg level yes/no-tumor markers yes/no/not applicable)Documented imaging studies yes/no (ultrasonography yes/no/not applicable-CT yes/no/not applicable-MRI yes/no/not applicable)Other yes/no/not applicableDocumentation:General clinical history yes/noEndocrinology clinical history yes/noEndocrinology report yes/noReferral form from A1.1 yes/noIodinated contrast media in prior 6 months yes/noDrug allergies yes/noAnticoagulants/antiaggregants yes/noCoagulopathies yes/noProsthesis yes/noPrior local surgery yes/noIndirect laryngoscopy yes/noPrior voice disease yes/noAirway evaluation yes/noNeck mobility evaluation yes/noExitSurgical clinical history yes/noPatient information yes/noSurgical clinical report yes/noInformed consent yes/noIndications on comorbidity yes/no/not applicableReferral form to A1.3Procedure proposed from A1.1 yes/noProgrammed procedure yes/noLaterality yes/no | EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberEntry form from A1.2 yes/noAccompanied patient yes/noComorbidity (see below [Table 4])Drug list yes/noLaboratory tests yes/no (thyroid profile yes/no-Ca/P level yes/no-vitamin D level yes/no-Mg level yes/no-electrolytes-proteins–hepatic and renal profile)DocumentationGeneral clinical history yes/noEndocrinology clinical history yes/noEndocrinology clinical report yes/noSurgical clinical history yes/noSurgical clinical report yes/noExitEuthyroid yes/noECG-cardiological assessment yes/noPrior anesthetic incidents yes/noASA gradeAirway risk evaluation yes/noDifficult airway yes/noAnesthesiology clinical history yes/noAnesthesiology clinical report yes/noPatient information yes/noInformed consent yes/noIndications on comorbidity yes/no/not applicable | EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberAdmission form yes/noAccompanied patient yes/noDrug list yes/noDocumentationGeneral clinical history yes/noEndocrinology clinical history yes/noEndocrinology clinical report yes/noSurgical clinical history yes/noAnesthesiology clinical history yes/noInformed consent for surgery yes/noAnesthesiology informed consent yes/noPreanesthetic indications and treatment yes/no/not applicableDrugs discontinued yes/noDrugs continued yes/noAnticoagulation regimen yes/no/not applicableProphylaxis for DVTE yes/no/not applicableExitVital signs yes/noNursing historyEuthyroid yes/no |
Checklists in thyroidectomy. Operative stage (B).
| B: operative stage | ||
| B1: entry. Before induction of anesthesia | B2: surgical pause Before skin incision | B3: exit. Before patient leaves operating room |
| Patient has confirmedHis/her identitySurgical siteProcedureConsentSite marking/not applicableAnesthesia safety control has been completedPulse oxymeter placed and activeHas the patient known allergies? No/yesDifficult airway/risk of aspiration?No/yes, and instruments and equipment/help availableRisk of bleeding>500mL (7mL/kg in children?No/yes, and intravenous access and adequate fluids available | Confirm that all team members have introduced themselves by name and roleSurgeon, anesthetist, and nurse verbally confirm:Patient identitySurgical siteProcedurePrevention of critical events:Surgeon reviews: critical or unforeseen steps, operating time, and expected blood lossThe anesthesia team reviews: if patient has some specific problemThe nursing team reviews: if sterility has been confirmed (with results of indicators) and doubts or problems related to instruments and equipment existHas antibiotic prophylaxis been administered in the past 60min? Yes/not applicableCan essential diagnostic images be visualized? Yes/not applicable | Nurse verbally confirms with the team:The name of the procedure performedThat counts of instruments, gauzes, and needles are correct (or not applicable)Sample labeling (including patient name)If problems related to instrumentation and equipment are pendingSurgeon, anesthetist, and nurse review the main aspects of patient recovery and treatmentExitPatent airway yes/noVerification of dressings and surgical woundVerification of drainagesSurgical procedure report yes/noAnesthesiology report yes/noPostoperative control sheets of Ca and PTH are availableAll treatment and postoperative care instructions have been written down |
| Complete documentation yes/noHemostasis system available yes/noNeuromonitoring system available yes/noCompliance with fasting yes/noDenture, prosthesis, or metallic objects yes/noPreanesthetic indications and treatment yes/no | Patient temperature monitoringNeuromuscular relaxation monitoringVerification of laterality (L1)Verification of hemostatic system yes/noVerification of neuromonitoring system yes/noFinal verification of vagus nerve signal | |
Checklists in thyroidectomy. Postoperative stage (C).
| C: Postoperative | |||
| C3: clinic | |||
| C1: recovery room | C2: hospitalization ward | C3.1: surgical clinic | C3.2: endocrinology clinic |
| EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberAll treatment and postoperative care instructions are clearDrug availability yes/no (Ca-vit D, Mg)Temperature monitoringECGBlood pressurePainPatent airway yes/noEmphysema yes/noVerification of dressings and surgical woundVerification of drainagesGeneral patient stateWound: bleeding/hematoma yes/noParesthesia yes/noRestlessness yes/noVomiting yes/noExitRecovery report yes/noIncidents have been recorded yes/noDischarge criteria have been verified yes/noInformation to patient and companions yes/no/not applicable | EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberAccompanied patient yes/noDrug list yes/noAll treatment and postoperative care instructions are clearDrug availability yes/no (Ca-vit D, Mg, levothyroxine)Verification of labeling yes/noIndications for control of calcemia and alarm signs of hypocalcemia are followed yes/noSurgical care guideline available yes/noPatent airway yes/noVoiceEmphysema yes/noVerification of dressings and surgical woundVerification of drainagesGeneral patient stateWound: bleeding/hematoma yes/noParesthesia yes/noRestlessness yes/noVomiting yes/no. VoiceSwallowingPainBlood pressureExitIndirect laryngoscopyHospital discharge reportDischarge criteria metPatient understands treatment scheme (levothyroxine yes/no/not applicable-Ca/vit D yes/no/not applicable)Review day for C3.1 and C3.2Request of laboratory control (6 weeks) | EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberAccompanied patient yes/noDrug list yes/noDocumentationGeneral clinical history yes/noEndocrinology clinical history yes/noHospital discharge reportHospitalization episodeHistological report yes/noUse of iodinated contrast media yes/noControl of treatment schemes (adequate drugs and dose: levothyroxine yes/no/not applicable-Ca/vit D yes/no/not applicable-anticoagulation regimen yes/no/not applicable)Indirect laryngoscopyVoiceSwallowingScarExitSurgical clinic reportVerbal informationPatient has understood verbal informationVerification of appointment for review by endocrinology C3.2Satisfaction surveySuggestions-complaints | EntryAdequate unit yes/noPatient identification yes/noCorrect clinical history numberAccompanied patient yes/noDrug list yes/noDocumentationGeneral clinical history yes/noEndocrinology clinical history yes/noEndocrinology clinical report yes/noSurgical clinical history yes/noHospitalization episodeHospital discharge reportHistological report yes/noControl of treatment schemes (adequate drugs and dose: levothyroxine yes/no/not applicable-Ca/vit D yes/no/not applicable)See laboratory controlRequest for ablation therapy with radioiodine yes/no/not applicableRequest for supplemental tests during ablation therapyExitIssue of endocrinology reportVerbal informationPatient has understood verbal information |
Listings allow for detecting omissions by recall (mnemonics) based on reiteration of points that should be checked.27
Checkpoints are planned at each stage in the process (endocrinology clinic before and after surgery; surgical clinic before and after thyroidectomy; anesthesiology clinic before surgery; operating room; recovery room and hospitalization ward before and after surgery) and are verified by the corresponding specialist at each stage.
Item correspond to factors contributing to the potential occurrence of perioperative incidents in thyroidectomies related to the patient, control of symptoms and signs, technological equipment, management, organization, and communication (information and documentation).
DiscussionPatient safety is the sum of management and technological factors at different levels with multiple connections.5 It is based on a culture of safety aimed at detecting and analyzing incident, search for the root causes in the systems, prepare guidelines to prevent recurrence, and devise prevention plans based on continuous improvement of processes and staff involvement, helping overcome barriers for implementation of changes.12
Adverse events are related to all stages in the care process, and their consequences are seen in patients (death, sequelae, complications) and in the process (hospital stay, readmissions, additional treatments) and increase costs.10 Causes (contributing factors) may be immediate (patient, team, environment) or root causes (management, organization, regulation).7
Patient care specialization implies more units and staff, which may make communication difficult26 Oral communication between professionals appears to be the best way to transfer patients, but the current design of care provision systems does not allow for it.26
Each type of failure may have multiple causes, including lack of CLs, computerized systems, or cognitive aids.27,30 CLs facilitate communication in patient transfers in the process stages, allow for standardized evaluation and transmission of updated information about patient state, decrease confusion, incorporate repetition and re-reading steps, and restrict exchange to the information needed to provide safe care to the patients.26
CLs are cognitive aids with an essential role in management of errors which are rarely included for publication.27
CLs serve to verify and identify the critical risk points related to the potential occurrence of safety incidents.12,27
The Work group of the clinical practice guidelines for safety of surgical patients recommends use of CLs in any surgical procedure to improve safety of surgery and decrease preventable complications with a strong grade of recommendation.16
However, use of CLs has a moderate efficacy to promote changes leading to more effective measures, such as organizational measures and process automatization/computerization.7 On the other hand, excess CLs may complicate the process by overburdening professional activity (the so-called “checklist fatigue”).27
No specific tools have been developed for interdisciplinary communication in thyroid surgery. The American Thyroid Association prepared a listing of information including all essential perioperative data that should be available to the professionals involved, and recommended transmission of information through electronic sheets with a synoptic and narrative report.28
The methodology used to develop the CLs presented added to the recommended methods for designing CLs29 the HFMEA method8,9 for identification and classification of the safety incidents and potential failures which were the basis of items included. This methodology combines the literature review with concept-sharing by experts for CL design.27,29 CLs facilitate routine verification of aspects that may contribute to cause critical (severe or frequent) or difficult to detect failures. Non-compliance helps professionals re-evaluate whether or not the process may continue to the next stage.
While application of CLs is not always directly correlated to significant improvements in patient care or error reduction, there are no data suggesting that CLs contribute to adverse event occurrence, and they do contribute to adherence to best practices and reduction of omission errors.27
To assess the results of CL implementation in thyroid surgery, we propose using indicators that measure patient safety issues (safety incidents, repeat surgery) and administrative aspects (hospital stay, surgical suspension rate, readmission rates and complaints).7–10
In conclusion, it should be emphasized that CLs allow for repeated verification at different checkpoints of the thyroidectomy process of data related to factors contributing to the occurrence of failures in each stage of the care process.
Conflicts of interestThere are no conflicts of interest.
We thank Dr. Carlos Ochoa Sangrador, head of the research support unit, Pedro Felipe Rodríguez de la Concepción (library), and Beatriz Pardal Peláez for manuscript review.
Please cite this article as: Pardal-Refoyo JL, Cuello-Azcárate JJ, Santiago-Peña LF. Diseño de una lista de verificación en la gestión de riesgos en tiroidectomía. Endocrinol Nutr. 2014;61:445-454.