To analyze the effects of a home-based physical exercise program on quality of life, metabolic control, and anthropometric and biochemical parameters in people over 60 years of age with type 2 diabetes mellitus.
MethodsEighty-four Spanish patients aged over 60 years were finally randomized to participate in a home-based, combined physical exercise program (aerobic and anaerobic exercises) or to receive conventional treatment for diabetes. At 6 months, effects on quality of life (EuroQoL questionnaire), HbA1c, fasting glucose, hypoglycemic events, weight, BMI, waist circumference, blood pressure, and biochemical parameters were assessed.
ResultsMean age of study participants was 66.7 (8.0) years. Patients in the exercise group showed an improved quality of life at 6 months based on EuroQol: 0.48 (0.38) vs 0.66 (0.35) and analogic scale 67.97 (18.92) vs 76.26 (20.14). An improved glycemic control was also seen: HbA1c 6.35 vs 6.0% and fasting glucose 151.2 (36.7) vs 137.6 (23.5) mg/dL, as well as a weight reduction by 1.7kg. Hypoglycemic events did not increase. No benefits were seen in the control group. Ten subjects withdrew from the study before 6 months.
ConclusionsA home-based physical exercise program improves quality of life, glycemic control, and weight in type 2 diabetic patients older than 60 years.
Analizar los efectos de un programa ambulatorio de ejercicio físico (PEFA) sobre la calidad de vida, el control metabólico y variables antropométricas y bioquímicas en diabéticos tipo 2 mayores de 60 años.
Pacientes y métodosOchenta y cuatro pacientes mayores de 60 años fueron finalmente randomizados a realizar un programa ambulatorio de ejercicio físico combinado (aeróbico y anaeróbico) o a recibir tratamiento convencional para su diabetes, incluyendo dieta y ejercicio. A los seis meses, se evaluó el efecto sobre la calidad de vida (test EuroQol), HbA1c, glucemia en ayunas, frecuencia de hipoglucemias, peso, IMC, perímetro cintura, presión arterial y otros parámetros bioquímicos.
ResultadosLa edad media de los pacientes que participaron en el estudio fue de 66,7 (8,0) años. Los pacientes incluidos en el grupo de ejercicio mejoraron su calidad de vida a los 6 meses: EuroQol 0,67 (0,37) vs 0,76 (0,26) y escala analógica 67,97 (18,92) vs 76,26 (20,14). Además se demostró una mejoría del control metabólico con HbA1c 6,35 vs 6,0%, glucosa en ayunas 151,2 (36,7) vs 137,6 (23,5) mg/dL y una reducción de peso de 1,7kg. Ninguno de estos beneficios se observó en el grupo control. No se demostró un incremento en la prevalencia de hipoglucemias. 10 pacientes abandonaron el estudio antes de los 6 meses.
ConclusionesUn programa ambulatorio de ejercicio físico mejora la calidad de vida, el control metabólico y el peso en sujetos mayores de 60 años con diabetes mellitus tipo 2.
Type 2 diabetes mellitus (DM) is a group of metabolic disorders mainly caused by insulin resistance and progressive beta cell impairment leading to deficient insulin secretion. The resulting hypoglycemia leads to chronic microvascular and macrovascular complications. Type 2 diabetes is associated with other vascular risk factors such as hypertension and dyslipidemia, and is highly related to obesity, sedentary lifestyles, and population ageing.1 Treatment is based on adequate diet, physical activity, and various drugs.2 Although the benefits of physical activity may be limited by different factors (including genetic factors, age, weight, and exercise type and duration3), physical exercise has been shown to improve quality of life (because it facilitates sleep and improves sleep quality) and mood (as it decreases anxiety, increases a sense of wellbeing, and facilitates stress management).4 In particular, in people with diabetes physical exercise improves glycemic control (by increasing sensitivity to insulin action), has a favorable impact on weight, and increases muscle mass.5–7 All of these effects may improve fragility in elderly people.
In our environment, patients are not used to performing daily physical activity. This situation is even more marked in the elderly population and leads to an intensification of drug treatment, with the associated problems of drug interactions and potential adverse reactions in such patients.8
Aerobic or resistance physical exercise training provides the greatest benefits to diabetic patients. It is recommended that it be accompanied by strength training to develop the muscles and to avoid weakness and loss of strength and muscle tone.9–11
There are different validated tools for measuring quality of life in the elderly Spanish population with type 2 DM, such as EuroQol 5-D, the SF-36 questionnaire, and the Sickness Impact Profile test. EuroQol (EQ-5D) is a reliable and valid tool, very sensitive to different conditions.12,13 Our group has used this quality of life questionnaire in similar studies.14 It is also easy to administer to elderly people because it is not difficult to complete.
The objective of this study was to compare, using the EQ-5D, the impact of an outpatient physical exercise program on quality of life in a subject population over 60 years with type 2 DM. As secondary objectives, metabolic control of diabetes, blood pressure (BP), lipid profile, and anthropometric parameters (weight, body mass index [BMI], and waist perimeter) were analyzed.
Patients and methodsA prospective, randomized, comparative, parallel cohort, interventional study using a 24-week physical activity program was conducted. Patients were recruited from June 2007 to October 2008. Patients enrolled into the intervention cohort followed the standard treatment for diabetes and also a specific 24-week physical activity program. The control cohort included subjects receiving standard treatment for diabetes only.
Study populationPatients were selected by a clinical interview at the health center outpatient clinic and a telephone call after a list of patients diagnosed with type 2 DM had been compiled from the Abucasis database of the Region of Valencia. Consecutive probability sampling was performed, followed by the randomization of each patient into one of the two cohorts.
Eighty-four participants were selected and distributed into 2 groups. One group received standard treatment and was given the usual dietary and exercise counseling, while the other group performed in addition a home-based physical education program (HPEP) with a total planned duration of 6 months. Standard dietary recommendations were made by nursing staff, and a diet including 1500–2000kcal/day divided into 5 meals [55% carbohydrates, 30% fat (containing less than 10% saturated fat), and 15% protein] was also provided in writing. A standard physical exercise regime consisting of 45min of moderate physical (particularly aerobic) activity at least 5 days a week was verbally recommended by the research team.
The inclusion criteria were as follows:
- 1.
Type 2 diabetes mellitus treated with diet and oral antidiabetics.
- 2.
Age >60 years
- 3.
Subjects who, based on their medically assessed health status and physical characteristics, were able to perform a physical training program designed by qualified professionals.
- 4.
Patients who had signed the informed consent after receiving information about the study objective.
Exclusion criteria were as follows:
- 1.
Treatment with diet or insulin administration alone.
- 2.
Known vascular complications of diabetes, such as coronary artery disease, stroke, nephropathy, retinopathy, and polyneuropathy which, in the investigator's judgment, may have compromised the physical integrity of the patient.
- 3.
Other chronic diseases restricting physical activity.
- 4.
Grade 2 or higher arterial hypertension (>160/100mmHg).
- 5.
Smokers.
The following measurements were performed:
- 1.
Quality of life testing. This was based on a validated tool, the Health-Related Quality of Life (HRQL) questionnaire. This analyzes 5 dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension was rated with one of three severity levels: 1 (no problems), 2 (some problem), and 3 (severe problem). The Spanish EuroQol group transforms the 243 possible combinations or states into a score ranging from 0 (no problems: a score of 1 in all 5 dimensions) to 1 (severe: a score of 3 in all 5 dimensions). A visual analogue scale consisting of a 20-cm long vertical line with marks from 0 (the worst imaginable health state) to 100 (the best imaginable health state) was also provided for. On the day of the interview the patients marked on the scale the levels which they considered best represented their overall state of health.
- 2.
Blood glucose control: the parameters tested included
- -
Glycosylated hemoglobin (HbA1c), measured by high performance liquid chromatography (HPLC).
- -
Basal blood glucose (mg/(dL) after fasting for 12h.
- -
Frequency of hypoglycemia, defined in terms of symptoms related to hypoglycemia as perceived by the patient after carbohydrate intake and by a capillary blood glucose level of 55mg/dL or less.
- -
- 3.
Blood pressure.
- 4.
Anthropometric parameters: weight in kg, BMI in kg/m2, and waist circumference in cm.
- 5.
Lipid profile: total, LDL, and HDL cholesterol and triglycerides.
- 6.
Insulin resistance based on the HOMA-IR (homeostasis model assessment of insulin resistance).
- 7.
Prior physical exercise: subjects who performed more than 150min of physical activity per week were considered to be taking exercise before the start of the program.
The same visiting timetable was used both for subjects doing the exercise program and for control subjects. A total of 8 visits were performed. Patients attended the clinic for 3 visits (at baseline, at 3 months, and at 6 months for the final visit) where blood sampling, ECG, measurement of anthropometric parameters, BP, heart rate, and measurement of quality of life were performed. There were 3 telephone visits to remind patients of the exercise program. The remaining two visits were with nursing staff to assess diet and exercise compliance.
The physical activity program lasted 24 weeks and had 2 main objectives: (a) to improve strength, and (b) to improve aerobic capacity.
Physical activity programStrength training requires at least 2 days per week, while cardiovascular or aerobic training requires at least 1 day per week. Strength training consisted of different circuits involving big muscle groups in which work intensity gradually increased from 75% to 95% of the repetition maximum in 40s. For aerobic sessions, various types of both outdoor and indoor activities were combined, including orienteering hikes, dancing, games, and so on. The program was explained verbally and in writing to patients by physical education graduates once they had been found to meet the inclusion and exclusion criteria and after performance of a resistance and strength test.
Program adherence: participants were categorized into 3 groups based on subjective assessment of their degree of exercise compliance (scored from 0 to 10). Compliance was rated as low, medium, or high depending on whether the score was 0–3, 4–6 or 7–10 respectively.
Statistical analysisSince a 30% drop-out rate from the physical exercise program was expected, it was estimated that 35 patients by group would be sufficient to document differences in quality of life before and after physical exercise with a one-sided error alpha of 0.05 and to be able to apply parametric statistics.
SPSS v.14.0 software was used for statistical analysis. A descriptive analysis was made of the frequencies of qualitative variables using proportions with a 95% confidence interval, and of quantitative variables using centralization (mean and median) and scatter (standard deviation and range) measures. The association between variables was studied using a Chi-square test for categorical variables and a Student's t test for continuous variables. A value of p<0.05 was considered statistically significant.
Good clinical practice standards were followed, and approval was obtained from the ethics and research committees of the Consorcio Hospital General Universitario de Valencia.
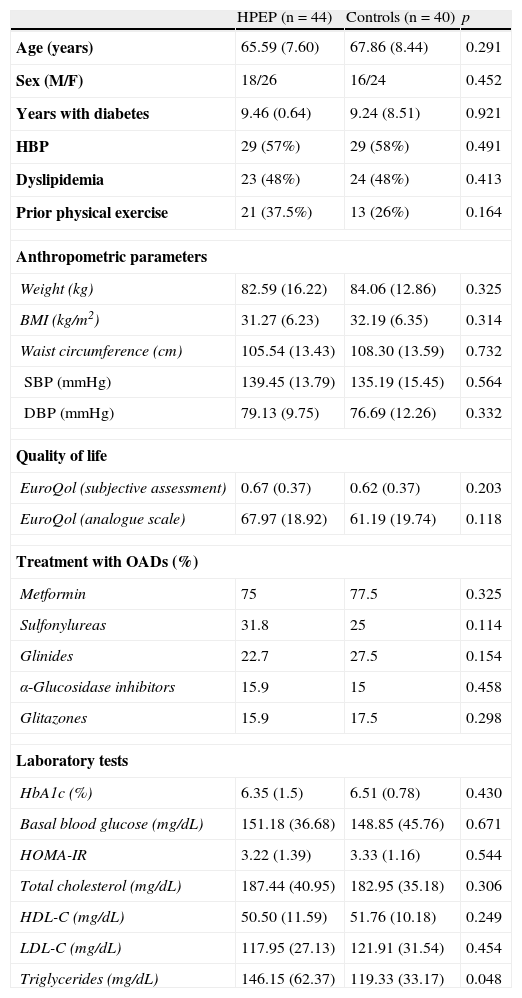
ResultsA total of 84 diabetic patients were recruited. Fourteen of these patients did not start the program for different reasons. Finally, 44 patients were assigned to the HPEP and 40 patients to the control group. Both groups showed similar clinical characteristics (Table 1).
Baseline characteristics of the study population. Quantitative variables are given as mean (SD). Frequency variables are given as percentages (%) after patient numbers. HPEP: home-based physical exercise program. BMI: body mass index. SBP: systolic blood pressure. DBP: diastolic blood pressure. HOMA-IR: homeostasis model assessment of insulin resistance.
| HPEP (n=44) | Controls (n=40) | p | |
| Age (years) | 65.59 (7.60) | 67.86 (8.44) | 0.291 |
| Sex (M/F) | 18/26 | 16/24 | 0.452 |
| Years with diabetes | 9.46 (0.64) | 9.24 (8.51) | 0.921 |
| HBP | 29 (57%) | 29 (58%) | 0.491 |
| Dyslipidemia | 23 (48%) | 24 (48%) | 0.413 |
| Prior physical exercise | 21 (37.5%) | 13 (26%) | 0.164 |
| Anthropometric parameters | |||
| Weight (kg) | 82.59 (16.22) | 84.06 (12.86) | 0.325 |
| BMI (kg/m2) | 31.27 (6.23) | 32.19 (6.35) | 0.314 |
| Waist circumference (cm) | 105.54 (13.43) | 108.30 (13.59) | 0.732 |
| SBP (mmHg) | 139.45 (13.79) | 135.19 (15.45) | 0.564 |
| DBP (mmHg) | 79.13 (9.75) | 76.69 (12.26) | 0.332 |
| Quality of life | |||
| EuroQol (subjective assessment) | 0.67 (0.37) | 0.62 (0.37) | 0.203 |
| EuroQol (analogue scale) | 67.97 (18.92) | 61.19 (19.74) | 0.118 |
| Treatment with OADs (%) | |||
| Metformin | 75 | 77.5 | 0.325 |
| Sulfonylureas | 31.8 | 25 | 0.114 |
| Glinides | 22.7 | 27.5 | 0.154 |
| α-Glucosidase inhibitors | 15.9 | 15 | 0.458 |
| Glitazones | 15.9 | 17.5 | 0.298 |
| Laboratory tests | |||
| HbA1c (%) | 6.35 (1.5) | 6.51 (0.78) | 0.430 |
| Basal blood glucose (mg/dL) | 151.18 (36.68) | 148.85 (45.76) | 0.671 |
| HOMA-IR | 3.22 (1.39) | 3.33 (1.16) | 0.544 |
| Total cholesterol (mg/dL) | 187.44 (40.95) | 182.95 (35.18) | 0.306 |
| HDL-C (mg/dL) | 50.50 (11.59) | 51.76 (10.18) | 0.249 |
| LDL-C (mg/dL) | 117.95 (27.13) | 121.91 (31.54) | 0.454 |
| Triglycerides (mg/dL) | 146.15 (62.37) | 119.33 (33.17) | 0.048 |
Ten patients withdrew during the study, 4 from the HPEP group and 6 from the control group.
According to their subjective assessment, participants performed HPEP 3.71 (2.32) days per week (95% CI 1.24–3.30), with a mean of 43.81 (14.70)min daily (95% CI 16.26–41.96). Mean exercise adherence, assessed from 1 to 10, was clearly higher in the HPEP group, 6.32 (2.81) as compared to the control group, 2.21 (2.38), p<0.05. As regards subjective assessment of diet compliance (also scored from 1 to 10), a slightly better compliance was seen in the HPEP group, 6.65 (3.01) as compared to 5.93 (2.88) in the control group (p 0.047).
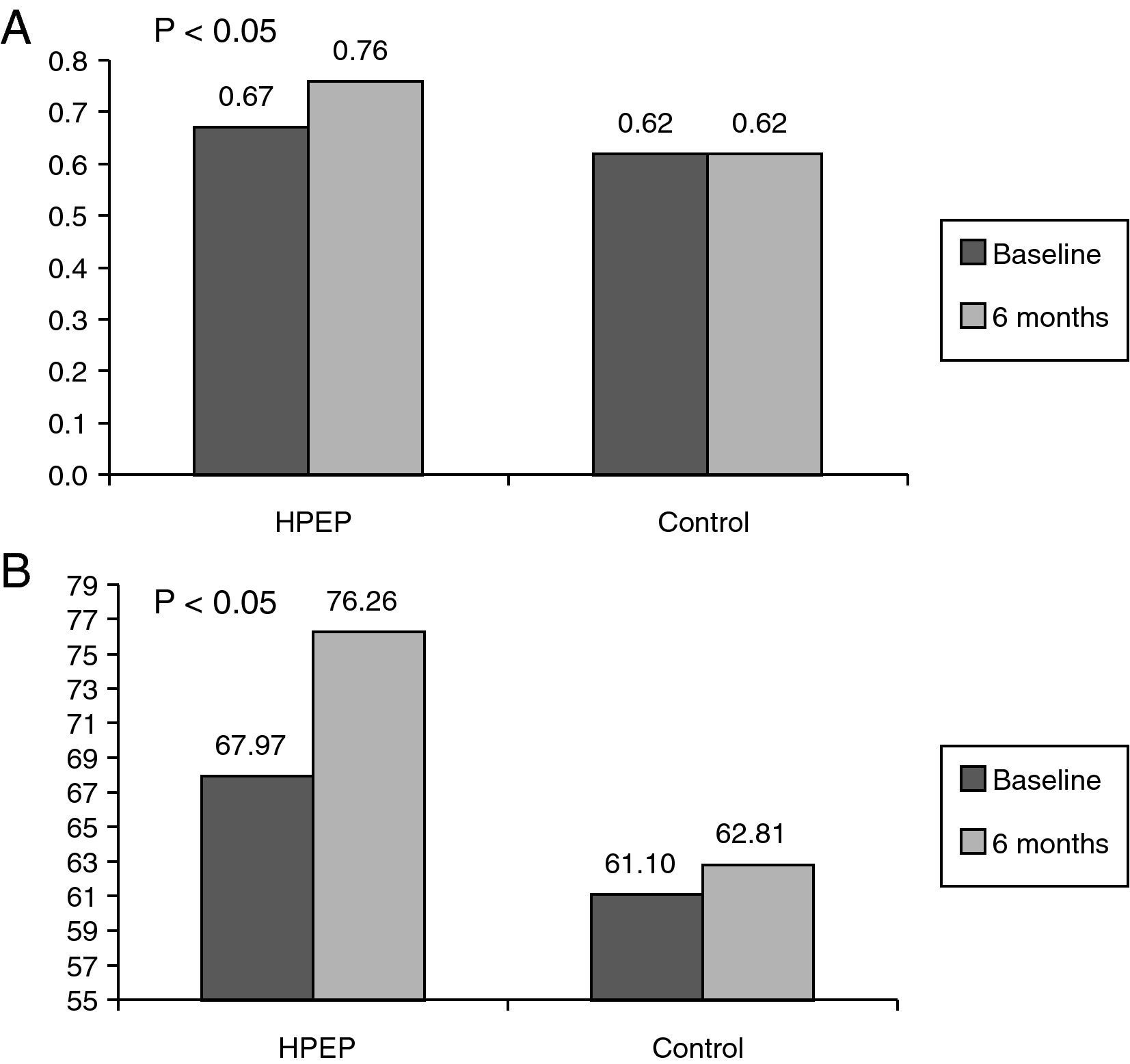
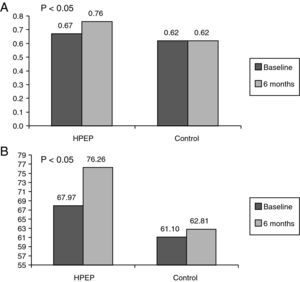
Quality of life improved in the HPEP group (baseline vs 6 months): EuroQol 0.67 (0.37) vs 0.76 (0.26) (p<0.030; 95% CI −0.263 to −0.08). No changes occurred in the control group regarding quality of life, as measured by EuroQol: 0.62 (0.37) vs 0.62 (0.31); p=0.925 (95% CI −0.087 to 0.096) (Fig. 1A). The EuroQol analogue scale also showed a significant improvement in the HPEP group at study end. Thus, the HPEP group showed scores of 67.97 (18.92) at the baseline visit vs 76.26 (20.14) at 6 months (p=0.045), as compared to 61.19 (19.74) vs 62.81 (17.89) respectively in the control group (p=ns) (Fig. 1B).
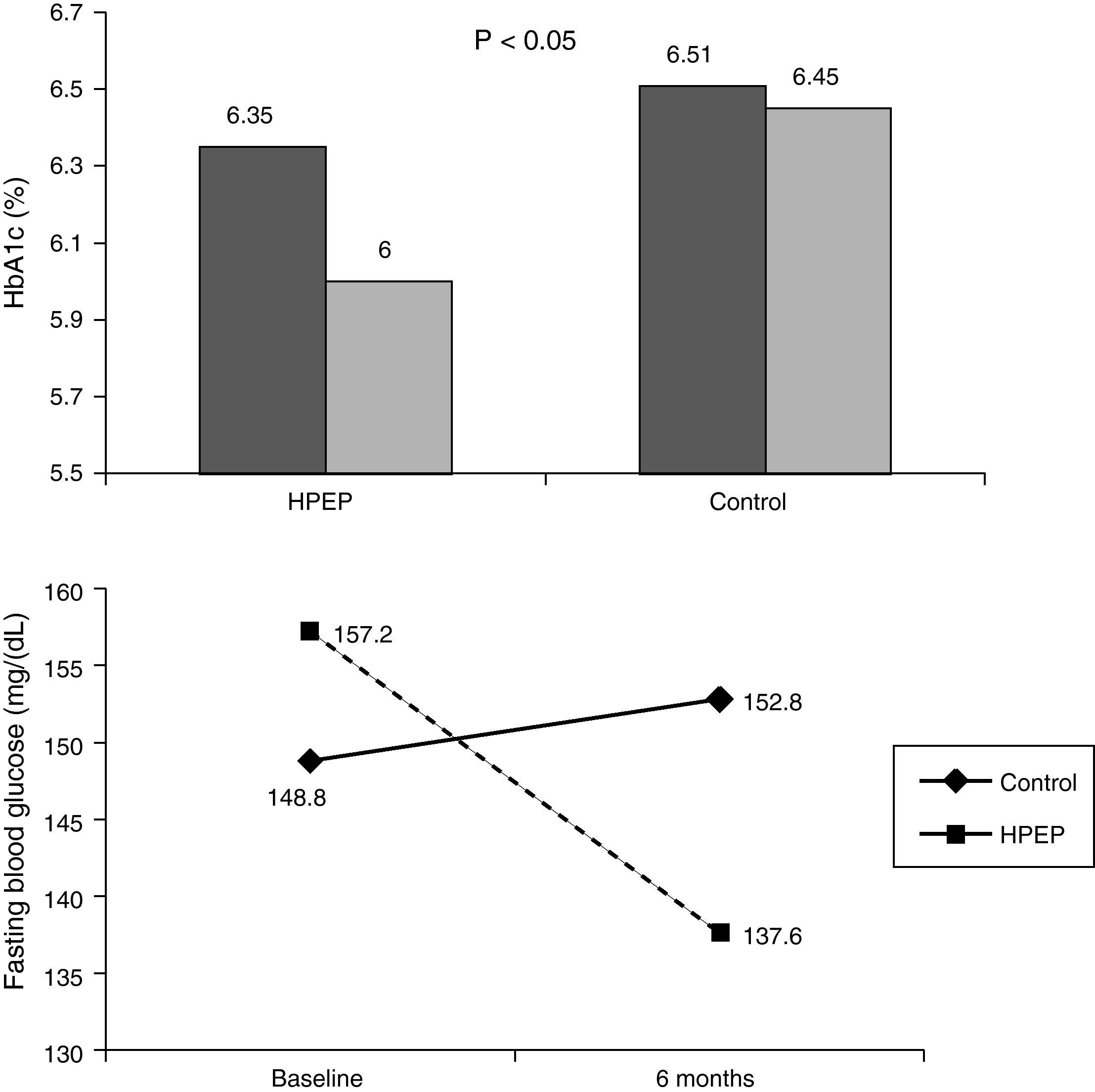
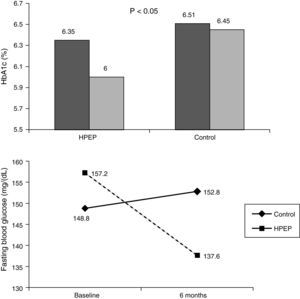
With regard to the metabolic control of diabetes, patients in the HPEP group showed improved HbA1c levels: 6.35 (1.5) at baseline vs 6.00 (0.83) at 6 months (p=0.008). No changes were found in the control group: 6.51 (0.78) vs 6.45 (1.49) (p=ns) (Fig. 2A). Comparison of HbA1c at 6 months between the groups was significant (p=0.042), with a mean of 0.3% (0.3) in favor of the control group.
Basal blood glucose levels also improved in the HPEP group: 151.18 (36.68) mg/dL at the baseline visit vs 137.63 (25.81) at 6 months (p=0.002). Basal blood glucose did not change in the control group: 148.85 (45.76) vs 152.76 (38.22) at 6 months (p=ns) (Fig. 2B). Patients in the HPEP group experienced 3.81 (0.42) hypoglycemic events, as compared to 3.42 (0.51) events in the control group (p=ns).
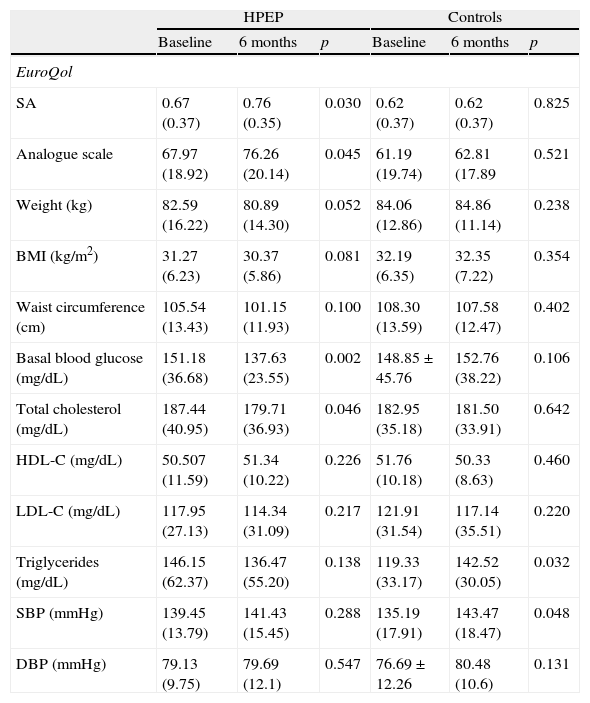
A 1.7kg body weight increase was found in the HPEP group at study end: 82.59 (16.22) as compared to 80.98 (14.30) kg (p=0.052; 95% CI 1.0–2.38), while weight increased 0.8kg in the control group: 84.06 (12.86) vs 84.86 (11.14) kg (p=ns; 95% CI −0.43 to 1.53). Thus, total weight difference between the HPEP and control groups was 2.5 (0.41) kg (95% CI 1.08–3.53), a significant difference (p=0.038). The HPEP group also showed reductions in BMI and waist circumference (Table 2). Thus, at 6 months, the difference between the HPEP and control groups was 1.1 (0.32) kg/m2 (95% CI 0.93–2.22) for BMI and 4.9 (1.48) cm (95% CI 0.73–6.66) for waist circumference.
Changes in the HPEP and control groups from baseline to 6 months.
| HPEP | Controls | |||||
| Baseline | 6 months | p | Baseline | 6 months | p | |
| EuroQol | ||||||
| SA | 0.67 (0.37) | 0.76 (0.35) | 0.030 | 0.62 (0.37) | 0.62 (0.37) | 0.825 |
| Analogue scale | 67.97 (18.92) | 76.26 (20.14) | 0.045 | 61.19 (19.74) | 62.81 (17.89 | 0.521 |
| Weight (kg) | 82.59 (16.22) | 80.89 (14.30) | 0.052 | 84.06 (12.86) | 84.86 (11.14) | 0.238 |
| BMI (kg/m2) | 31.27 (6.23) | 30.37 (5.86) | 0.081 | 32.19 (6.35) | 32.35 (7.22) | 0.354 |
| Waist circumference (cm) | 105.54 (13.43) | 101.15 (11.93) | 0.100 | 108.30 (13.59) | 107.58 (12.47) | 0.402 |
| Basal blood glucose (mg/dL) | 151.18 (36.68) | 137.63 (23.55) | 0.002 | 148.85±45.76 | 152.76 (38.22) | 0.106 |
| Total cholesterol (mg/dL) | 187.44 (40.95) | 179.71 (36.93) | 0.046 | 182.95 (35.18) | 181.50 (33.91) | 0.642 |
| HDL-C (mg/dL) | 50.507 (11.59) | 51.34 (10.22) | 0.226 | 51.76 (10.18) | 50.33 (8.63) | 0.460 |
| LDL-C (mg/dL) | 117.95 (27.13) | 114.34 (31.09) | 0.217 | 121.91 (31.54) | 117.14 (35.51) | 0.220 |
| Triglycerides (mg/dL) | 146.15 (62.37) | 136.47 (55.20) | 0.138 | 119.33 (33.17) | 142.52 (30.05) | 0.032 |
| SBP (mmHg) | 139.45 (13.79) | 141.43 (15.45) | 0.288 | 135.19 (17.91) | 143.47 (18.47) | 0.048 |
| DBP (mmHg) | 79.13 (9.75) | 79.69 (12.1) | 0.547 | 76.69±12.26 | 80.48 (10.6) | 0.131 |
HPEP: home-based physical exercise program; SA: subjective assessment of health state using EuroQol; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure.
There were no differences in BP levels in the HPEP group (baseline vs 6 months): systolic BP (SBP) 139.45±13.79 vs 141.43 (15.45) and diastolic BP (DBP) 79.13±9.75 vs 79.69 (12.1), while the control group showed increased SBP levels: 135.19±17.91 vs 143.47 (18.47) (p=0.008) and no changes in DBP 76.69±12.26 vs 80.48 (10.6).
Table 2 shows the results of variables tested at study start and at 6 months.
DiscussionThis study shows that a home-base physical exercise program may improve quality of life, metabolic control, and some anthropometric parameters in subjects over 60 years of age with type 2 DM.
Results of physical activity programs have already shown their benefits in patients with type 2 diabetes. Ambulatory programs, which allow patients to make their own exercise plan, have also confirmed these benefits.15
Quality of life improves with the routine practice of exercise. This has also been shown in patients with type 2 DM or glucose intolerance in different studies and by using any quality of life questionnaire and any physical activity program.6,17,18 In our study, quality of life was assessed using validated and standardized methods which allow for comparing results with similar studies and even with other populations. Studies conducted on an elderly population without diabetes using less structured and less intensive programs have also shown benefits regarding quality of life.16 We think that 6 months is an adequate time for analyzing differences in quality of life, but the real challenge would be to show that both physical activity and quality of life improvements are maintained over time.
As in other studies, limitations of our quality of life results may include interference by metabolic improvement or added motivation due to the research team (teachers, nurses, and physicians) transmitting to patients an enthusiasm for doing exercise. Our study also showed a better compliance with diet in the HPEP group, which could have interfered with the metabolic and anthropometric results.
We selected a combined exercise program because in our view, and in agreement with multiple guidelines, the combination of strength and resistance provides greater benefits, by increasing muscle mass, optimizing oxygen consumption, and improving glycemic control.19 Our group had experience with this type of program, with which similar results were achieved in a population of obese postmenopausal women.14
This study was able to show a modest reduction in HbA1c levels. A review of randomized, controlled trials including a meta-analysis of such trials showed mean reductions in HbA1c by 1.4% and in basal blood glucose by 22mg/dL 6 months after the start of physical exercise,20 but other studies reported no improvement in metabolic control.21–23 Our study achieved a slight but significant decrease in HbA1c, but it should be noted that patients had excellent baseline levels of HbA1c. A smaller (14mg/dL) but significant decrease was found in basal blood glucose.
Mean time since onset of diabetes (9 years), mean HbA1c levels, and an absence of complications and insulin treatment suggested that this was a population with a relatively good control over time. Frequency of hypoglycemic events was similar between the groups and relatively low for HbA1c values. No changes were made in hypoglycemic treatment, and it is likely that both comprehensive diabetes education and close monitoring prevented hypoglycemic events. Nevertheless, it may be concluded that controlled physical activity did not increase the risk of hyperglycemia.
The weight difference between the HPEP and control groups at study end increased by 2.5kg as the result of both a weight decrease by 1.7kg in the HPEP group and a weight increase by 0.8kg in the control group. BMI and waist circumference also decreased, but these reductions were not statistically significant. These data have also been reported in similar studies.20
As regards lipid profile, decreases in total cholesterol and triglycerides should be stressed. While a weight loss of 1kg decreases cholesterol and triglyceride levels by 2–5mg/dL and 14mg/dL respectively,24 physical activity itself appeared to be an independent factor in our study. Differences in LDL cholesterol as compared to the control group did not reach statistical significance, but it should be noted that mean levels at study start, close to 115mg/dL, were not too high. The HPEP group showed no reduction in blood pressure levels, which remained stable. BP slightly increased at 6 months in the control group, a change for which no explanation is available. At any rate, it should be noted that those were patients who were already taking several lipid lowering and antihypertensive drugs before the start of the study. Minor changes made at the 3-month visit in the antihypertensive treatment of uncontrolled patients may have influenced BP levels, but reporting such changes is outside the main objective of this study.
Program adherence was acceptable. Although the exercise compliance score subjectively reported by patients was not particularly high (6.21/10), the drop-out rate was reasonable as compared to other studies which have reported an 80% patient retention at the end of the program as very good,25,26 and may even be considered as good as compared to studies conducted in obese patients. Most patients who dropped out from the program did so for family reasons or due to difficulties in attending program learning sessions.
There is no doubt that telephone calls and the interest shown by physicians and nurses, as well as by physical education professionals, were very important factors for maintaining adherence. Specifically, telephone calls have been shown to be helpful for improving aspects of treatment adherence in diabetes.27
In conclusion, this study showed that a home-based physical exercise program improves quality of life, blood glucose control, and weight in elderly patients with type 2 DM, and supports the significance of physical exercise in the treatment of diabetes.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Ferrer-García JC, et al. Beneficios de un programa ambulatorio de ejercicio físico en sujetos mayores con diabetes mellitus tipo 2. Endocrinol Nutr. 2011;58:387-94.