To evaluate the association between the type of information source and the level of knowledge about diabetes mellitus in patients with type 2 diabetes.
MethodologyA cross-sectional study was conducted at a reference diabetes and hypertension center in Lima, Peru, during 2014. Level of knowledge was measured using the Diabetes Knowledge Questionnaire-24 and 12 information sources. Patients with 75% correct answers were considered to have a good knowledge. Adjusted odds ratios were calculated.
ResultsOf the total 464 patients enrolled, 52.2% were females, and 20.3% used the Internet as information source. Mean knowledge was 12.9±4.8, and only 17.0% had a good knowledge, which was associated with information on diabetes obtained from the Internet (OR=2.03, 95% CI 1.32–3.14), and also from other patients (OR=1.99, 95% CI 1.20–3.31). Good knowledge was also associated with postgraduate education (OR=3.66, 95% CI 1.21–11.09), disease duration longer than 12 years (OR=1.91, 95% CI 1.22–3.01), and age older than 70 years (OR=0.39, 95% CI 0.21–0.72).
ConclusionSearch for information in the Internet was positively associated to a good level of knowledge. It is suggested to teach patients with diabetes to seek information on the Internet and, on the other hand, to develop virtual spaces for interaction of patients with diabetes.
Evaluar si existe asociación entre el tipo de fuente de información y el nivel de conocimiento sobre la diabetes mellitus en pacientes con diabetes tipo 2.
MetodologíaEstudio transversal realizado en el Centro de Atención Integral de Diabetes e Hipertensión en Lima, Perú, en el año 2014. Se midió el nivel de conocimientos con el Diabetes Knowledge Questionnaire-24 y el uso de 12 fuentes de información. Se consideró que tenían buen conocimiento aquellos con un 75% de las respuestas correctas. Se calcularon las razones de prevalencia ajustadas.
ResultadosSe incluyeron 464 pacientes con diabetes, el 52,2% fueron mujeres y el 20,3% usaron Internet como fuente de información. La media de conocimientos fue de 12,9±4,8; solo un 17,0% obtuvo un conocimiento bueno, y estuvo asociado con obtener información de diabetes de Internet (RP=2,03, IC 95% 1,32–3,14), y también de otros pacientes (RP=1,99, IC 95% 1,20–3,31). Asimismo, se relacionó con tener un posgrado (RP=3,66, IC 95% 1,21–11,09), tener más de 12 años de diagnóstico (RP=1,91, IC 95% 1,22–3,01) y una edad mayor a 70 años (RP=0,39, IC 95% 0,21–0,72).
ConclusiónLa búsqueda de información en Internet está asociada positivamente a un buen nivel de conocimientos. Se propone enseñar a los pacientes con diabetes a buscar información en Internet y, por otro lado, desarrollar espacios virtuales para la interacción de los pacientes con esta dolencia.
Diabetes mellitus is a metabolic disorder that has become a public health problem worldwide because of the increasing number of people who suffer from it. As in any chronic disease, education is essential for good monitoring. Various studies have shown that diabetes education is considered one of the mainstays for achieving good metabolic control. Such education is intended to educate patients regarding the disease and to promote the maintenance of skills that will allow them to lead an optimal daily life.1 It is thus intended to avoid and/or delay the various health complications caused by this disease, to improve the quality of life of patients, and to decrease the high hospital costs involved.2
In Peru, the level of diabetes awareness on the part of sufferers of the disease has been assessed at public hospitals by physicians and researchers in diabetes control in order to determine whether their efforts were effective in imparting such awareness. They found fair, low, or deficient understanding,3,4 However, this was measured with their own tools and with no evidence of prior validation.5
The Diabetes Knowledge Questionnaire (DKQ-24) is a summary of the original 60-item questionnaire6 which was translated into Spanish and adapted to the Hispanic population living in the United States.5 It has been used in several studies in Latin America in countries such as Mexico, Costa Rica, and Guatemala, so ensuring its acceptability and understanding on the part of the great majority of surveyed people.5,7,8
The source from which information about the disease is obtained is associated with preventive and therapeutic types of behavior.9 The information source is able to motivate and maintain the interest of patients with diabetes so that they take an active part in their treatment and satisfactory results are achieved. New information and communication technologies (electronic and audiovisual devices such as mobile telephones and computers) are being incorporated into the practice of health because of their potential to improve access to health care, information exchange, and patient management both individually and for advanced age groups.10
The influence of information sources on diabetes education and knowledge of the disease by patients who suffer from it is as yet little known.11 In addition, both the lack of patient-focused objectives and problems in monitoring the results12 result in an incomplete or otherwise unsatisfactory development of educational programs and, as a result, in deficient knowledge by patients. The purpose of this study was, therefore, to ascertain if a relationship exists between information sources and the level of knowledge of patients with diabetes. It is hoped that our results will support the design of training programs and educational interventions, encourage the greater presence of such educational programs and improve them and that these programs will in turn be able to decrease potential complications and thus increase the quality of life of patients with diabetes.
Patients and methodsStudy designAn analytical, cross-sectional study was conducted during the second half of 2014 at the public Center for the Integral Care of Diabetes and Hypertension (EsSalud) in Lima, Peru.
Population and sampleSample size was estimated using the difference between proportions formula: it was calculated that 31% of patients exposed to one type of information would have a high level of knowledge, as compared to 19% of those in the group not exposed to such information (data based on a pilot study). Assuming a 95% confidence interval and an 80% power, it was estimated that 440 subjects would be required. A higher number of subjects were recruited to take account of refusals and inadequately completed surveys. Patients with type 2 diabetes mellitus diagnosed at least six months before, above 18 years of age, with no mental or visual disturbances, and able to read and write were recruited. The participants were consecutively recruited on the days and times selected for data collection.
MeasurementsThe response variable was determined from the DKQ-24, translated into Spanish and adapted to the Hispanic population living in the United States,5 with three response options for each question: yes, no, don’t know. The score ranged from 0 to 24, and the higher the score, the greater the knowledge. Good knowledge was defined as more than 75% correct answers (18 or more), according to the literature consulted.13,14 A Cronbach's alpha of 0.84 was obtained in this study.
For the exposure variable, the use of 12 information sources was measured, with subjects being asked through which source their information about diabetes was obtained, each type of source being indicated by the answer ‘yes’ or ‘no’. The sources proposed were healthcare professionals, leaflets, television, radio, Internet, newspapers/journals, relatives, friends, other patients, talks about diabetes, club or group of patients with diabetes, dietitian. These sources were identified through prior studies and tested in a pilot study conducted in January 2014. Other variables of interest included in the analysis were age (<60 years, 61–70 years, >70 years), sex (male or female), educational level (no formal/primary, secondary, technical, university, postgraduate education), family history (relatives with diabetes, parents with diabetes), years since diagnosis (0–4, 5–12, >12), high blood pressure (yes/no), and type of treatment (diet, exercise, oral antidiabetics, insulin). The questionnaires were self-administered. Finally, the population was characterized through the collection of weight, height, abdominal circumference, and fasting blood glucose, cholesterol, and triglyceride levels from the clinical records.
Ethical issuesThe study was approved by the ethics committee of the Peruvian University of Applied Sciences (CEI/228-04-14) and the Rebagliati Care Network of EsSalud (648-GRAR-ESSALUD-2014). The study objective was explained to each participant, after which their signed written informed consent was obtained. Participants were also requested to authorize our access to their clinical records in order to collect the above mentioned data.
Data analysisA double entry database was created using Microsoft® Excel 2010 software, and was exported to STATA® version 13.0 software after quality control. For descriptive analysis, relative frequencies were used for categorical variables, and the median and interquartile range were used for numerical variables after verifying that they were not normally distributed using a Shapiro–Wilk test. The variables of age and years since diagnosis were categorized using tertiles.
The frequency of a high level of knowledge in the DQK-24 (>75% correct answers) was described, and its association with the use of each information source, as well as other sociodemographic variables, was assessed using a Ch-squared test. For numerical variables, a Mann–Whitney-U test was used.
The magnitude of the association between each individual information source was assessed using crude and adjusted prevalence ratios (PR) with their 95% confidence intervals (95% CIs) in Poisson regression models with fixed variance, adjusted for demographic variables with a value of p<0.20 in the bivariate analysis (sex, age, educational level, parents with diabetes, insulin use, and years since diagnosis).
A new model was finally applied to identify the factors associated with a high level of knowledge, all the information and demographic variables were included in a single model, and they were ruled out through a backward stepwise model until the final model was achieved. A value of p<0.05 was considered statistically significant.
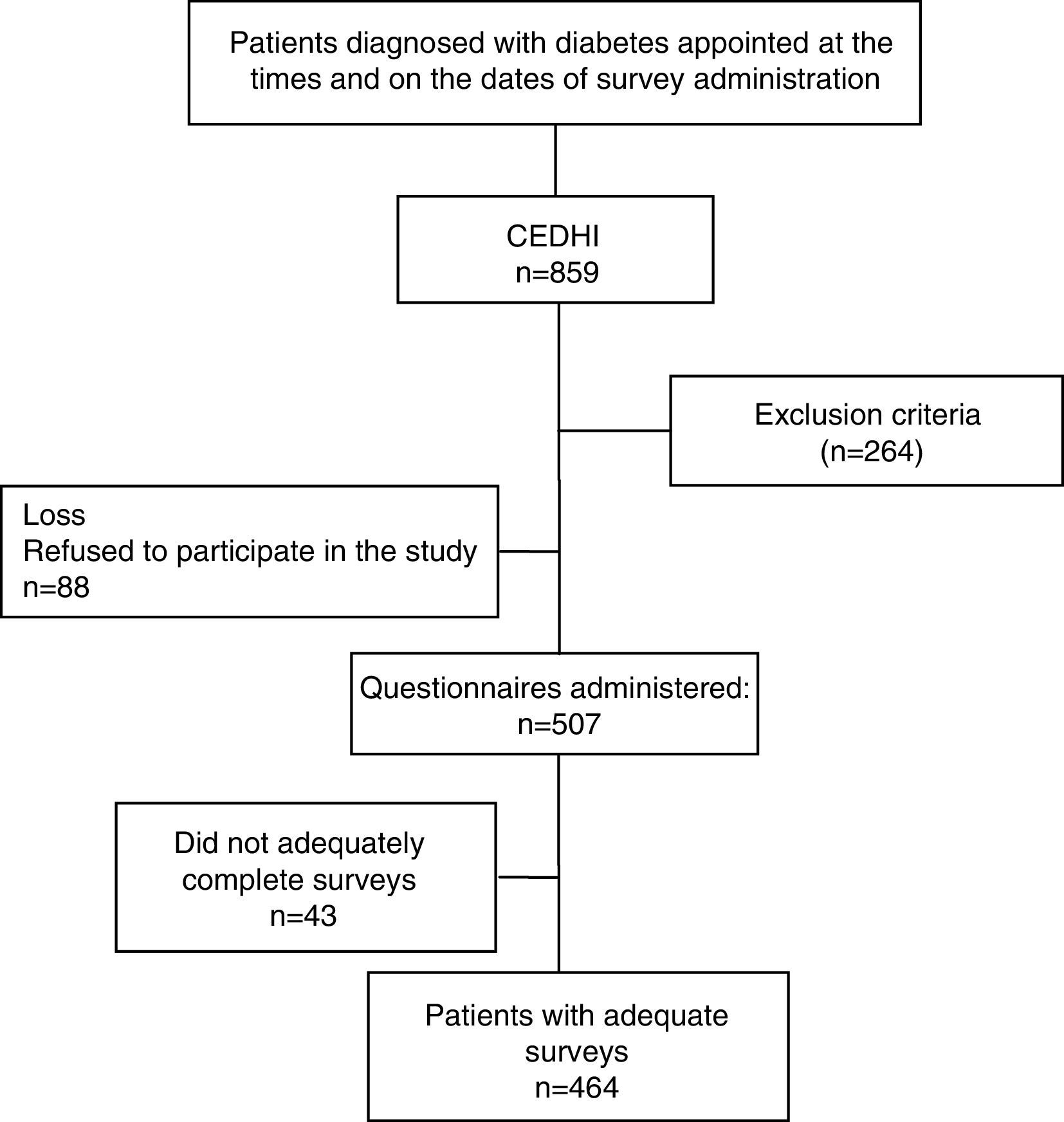
ResultsOf the 859 patients with diagnosed diabetes, selected on the dates and times at which the survey was administered, 595 met our inclusion criteria. Eighty-eight patients refused to participate in the study, and 43 were excluded because not all the variables of interest were available. The final study sample therefore consisted of 464 patients (Fig. 1).
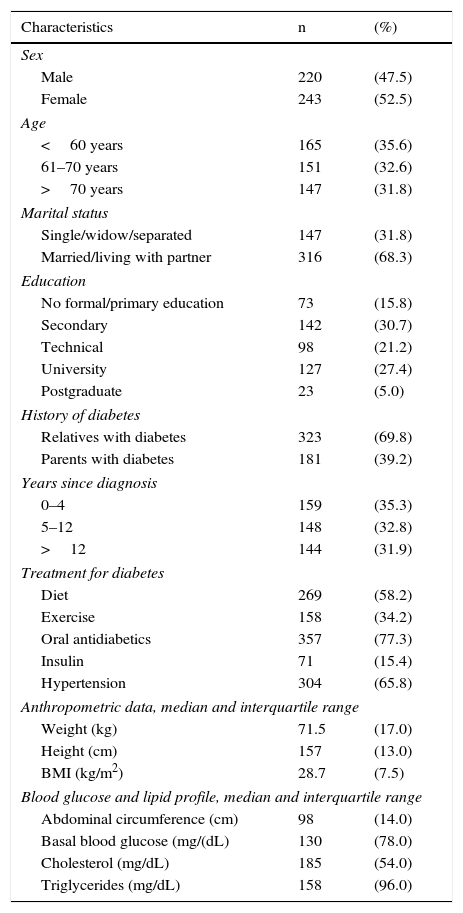
The mean age of the participants was 64.3±11.2 years, 68.3% were married or had a partner, and one third (32.4%) reported university or postgraduate education. The median time since diagnosis was 10.2±9.3 years. Diabetes was treated with oral antidiabetics in 77.3% of patients, while only 15.4% received insulin (Table 1).
Characteristics of patients with diabetes attending the Center for the Integral Care of Diabetes and Hypertension, EsSalud, Lima (Peru), 2014 (n=464).
| Characteristics | n | (%) |
|---|---|---|
| Sex | ||
| Male | 220 | (47.5) |
| Female | 243 | (52.5) |
| Age | ||
| <60 years | 165 | (35.6) |
| 61–70 years | 151 | (32.6) |
| >70 years | 147 | (31.8) |
| Marital status | ||
| Single/widow/separated | 147 | (31.8) |
| Married/living with partner | 316 | (68.3) |
| Education | ||
| No formal/primary education | 73 | (15.8) |
| Secondary | 142 | (30.7) |
| Technical | 98 | (21.2) |
| University | 127 | (27.4) |
| Postgraduate | 23 | (5.0) |
| History of diabetes | ||
| Relatives with diabetes | 323 | (69.8) |
| Parents with diabetes | 181 | (39.2) |
| Years since diagnosis | ||
| 0–4 | 159 | (35.3) |
| 5–12 | 148 | (32.8) |
| >12 | 144 | (31.9) |
| Treatment for diabetes | ||
| Diet | 269 | (58.2) |
| Exercise | 158 | (34.2) |
| Oral antidiabetics | 357 | (77.3) |
| Insulin | 71 | (15.4) |
| Hypertension | 304 | (65.8) |
| Anthropometric data, median and interquartile range | ||
| Weight (kg) | 71.5 | (17.0) |
| Height (cm) | 157 | (13.0) |
| BMI (kg/m2) | 28.7 | (7.5) |
| Blood glucose and lipid profile, median and interquartile range | ||
| Abdominal circumference (cm) | 98 | (14.0) |
| Basal blood glucose (mg/(dL) | 130 | (78.0) |
| Cholesterol (mg/dL) | 185 | (54.0) |
| Triglycerides (mg/dL) | 158 | (96.0) |
The mean level of knowledge according to DKQ-24 was 12.9±4.8, with a median of 13 and an interquartile range of 6. Only 17.0% had a good level of knowledge (≥75% correct answers).
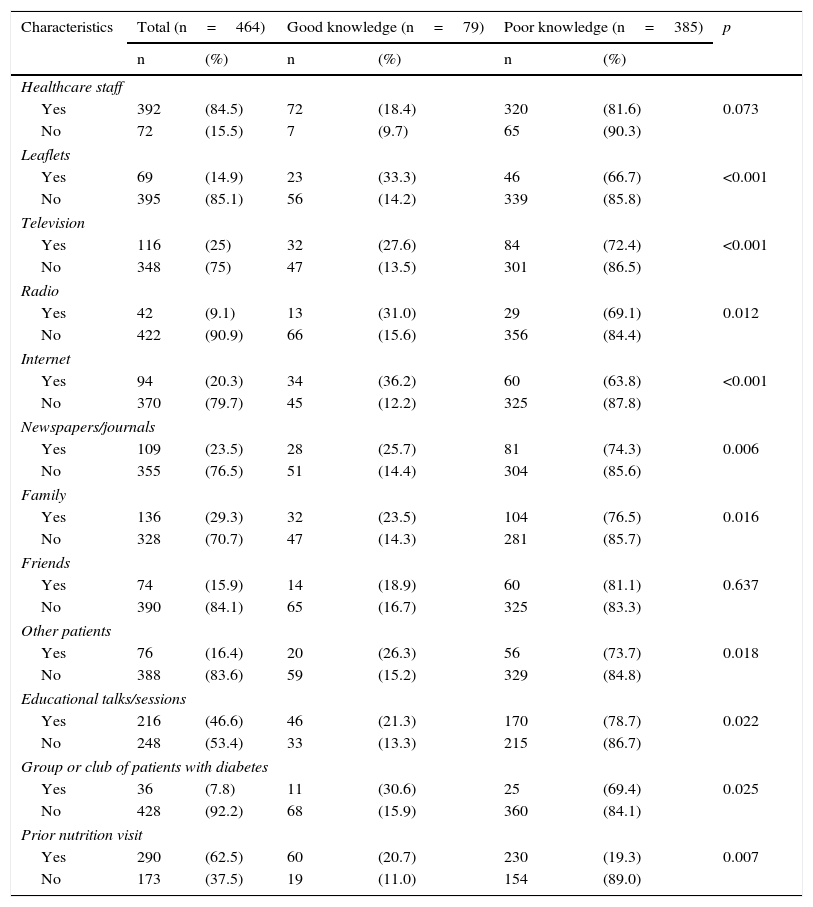
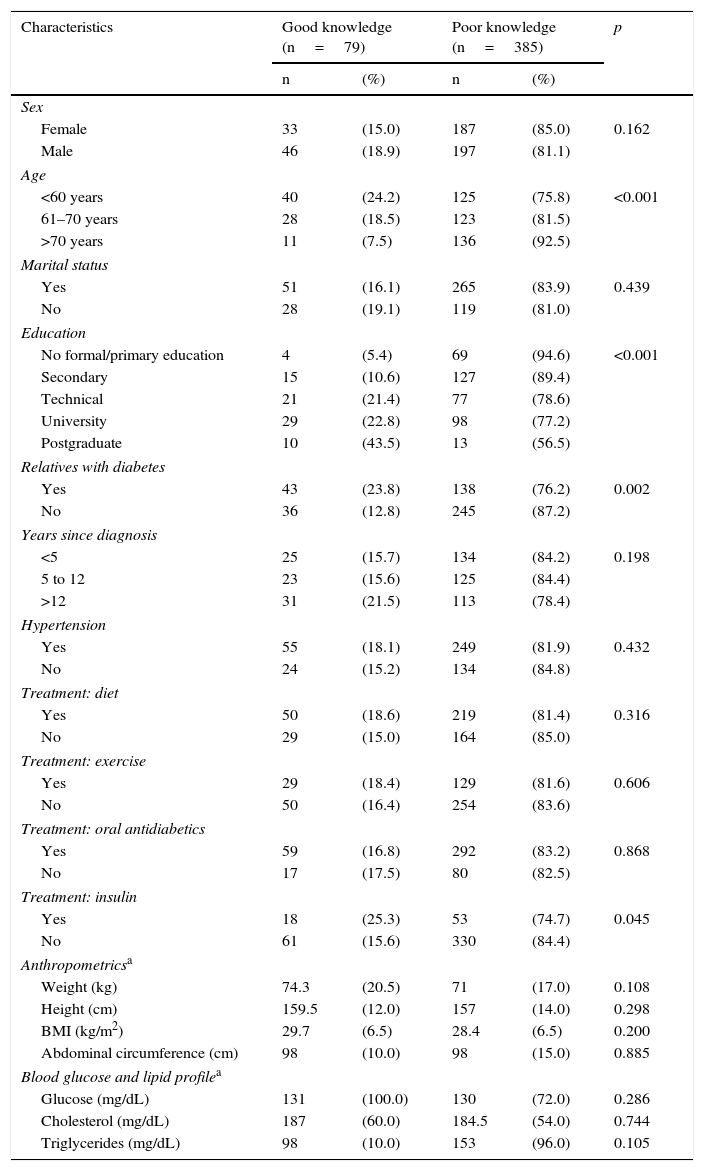
The most commonly used information sources were healthcare professionals (84.5%), prior consultation with a dietitian (62.5%), talks or educational sessions on diabetes (46.6%), relatives (29.3%), newspapers/journals (23.5%), television (25.0%), Internet (20.3%), and other patients (16.4%) (Table 2). No association was found in the bivariate analysis between level of knowledge and having friends or healthcare staff as a source of information (p>0.05), while an association was found with all other information sources. With regard to the characteristics of the population, an association was found with age, educational level, a family history of diabetes, and insulin therapy (Table 3).
Association between information sources and a good level of knowledge regarding diabetes in patients attending the Center for the Integral Care of Diabetes and Hypertension, EsSalud, Lima (Peru), 2014.
| Characteristics | Total (n=464) | Good knowledge (n=79) | Poor knowledge (n=385) | p | |||
|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | ||
| Healthcare staff | |||||||
| Yes | 392 | (84.5) | 72 | (18.4) | 320 | (81.6) | 0.073 |
| No | 72 | (15.5) | 7 | (9.7) | 65 | (90.3) | |
| Leaflets | |||||||
| Yes | 69 | (14.9) | 23 | (33.3) | 46 | (66.7) | <0.001 |
| No | 395 | (85.1) | 56 | (14.2) | 339 | (85.8) | |
| Television | |||||||
| Yes | 116 | (25) | 32 | (27.6) | 84 | (72.4) | <0.001 |
| No | 348 | (75) | 47 | (13.5) | 301 | (86.5) | |
| Radio | |||||||
| Yes | 42 | (9.1) | 13 | (31.0) | 29 | (69.1) | 0.012 |
| No | 422 | (90.9) | 66 | (15.6) | 356 | (84.4) | |
| Internet | |||||||
| Yes | 94 | (20.3) | 34 | (36.2) | 60 | (63.8) | <0.001 |
| No | 370 | (79.7) | 45 | (12.2) | 325 | (87.8) | |
| Newspapers/journals | |||||||
| Yes | 109 | (23.5) | 28 | (25.7) | 81 | (74.3) | 0.006 |
| No | 355 | (76.5) | 51 | (14.4) | 304 | (85.6) | |
| Family | |||||||
| Yes | 136 | (29.3) | 32 | (23.5) | 104 | (76.5) | 0.016 |
| No | 328 | (70.7) | 47 | (14.3) | 281 | (85.7) | |
| Friends | |||||||
| Yes | 74 | (15.9) | 14 | (18.9) | 60 | (81.1) | 0.637 |
| No | 390 | (84.1) | 65 | (16.7) | 325 | (83.3) | |
| Other patients | |||||||
| Yes | 76 | (16.4) | 20 | (26.3) | 56 | (73.7) | 0.018 |
| No | 388 | (83.6) | 59 | (15.2) | 329 | (84.8) | |
| Educational talks/sessions | |||||||
| Yes | 216 | (46.6) | 46 | (21.3) | 170 | (78.7) | 0.022 |
| No | 248 | (53.4) | 33 | (13.3) | 215 | (86.7) | |
| Group or club of patients with diabetes | |||||||
| Yes | 36 | (7.8) | 11 | (30.6) | 25 | (69.4) | 0.025 |
| No | 428 | (92.2) | 68 | (15.9) | 360 | (84.1) | |
| Prior nutrition visit | |||||||
| Yes | 290 | (62.5) | 60 | (20.7) | 230 | (19.3) | 0.007 |
| No | 173 | (37.5) | 19 | (11.0) | 154 | (89.0) | |
Association between population characteristics and level of knowledge regarding diabetes in patients attending the Center for the Integral Care of Diabetes and Hypertension, EsSalud, Lima (Peru), 2014.
| Characteristics | Good knowledge (n=79) | Poor knowledge (n=385) | p | ||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Sex | |||||
| Female | 33 | (15.0) | 187 | (85.0) | 0.162 |
| Male | 46 | (18.9) | 197 | (81.1) | |
| Age | |||||
| <60 years | 40 | (24.2) | 125 | (75.8) | <0.001 |
| 61–70 years | 28 | (18.5) | 123 | (81.5) | |
| >70 years | 11 | (7.5) | 136 | (92.5) | |
| Marital status | |||||
| Yes | 51 | (16.1) | 265 | (83.9) | 0.439 |
| No | 28 | (19.1) | 119 | (81.0) | |
| Education | |||||
| No formal/primary education | 4 | (5.4) | 69 | (94.6) | <0.001 |
| Secondary | 15 | (10.6) | 127 | (89.4) | |
| Technical | 21 | (21.4) | 77 | (78.6) | |
| University | 29 | (22.8) | 98 | (77.2) | |
| Postgraduate | 10 | (43.5) | 13 | (56.5) | |
| Relatives with diabetes | |||||
| Yes | 43 | (23.8) | 138 | (76.2) | 0.002 |
| No | 36 | (12.8) | 245 | (87.2) | |
| Years since diagnosis | |||||
| <5 | 25 | (15.7) | 134 | (84.2) | 0.198 |
| 5 to 12 | 23 | (15.6) | 125 | (84.4) | |
| >12 | 31 | (21.5) | 113 | (78.4) | |
| Hypertension | |||||
| Yes | 55 | (18.1) | 249 | (81.9) | 0.432 |
| No | 24 | (15.2) | 134 | (84.8) | |
| Treatment: diet | |||||
| Yes | 50 | (18.6) | 219 | (81.4) | 0.316 |
| No | 29 | (15.0) | 164 | (85.0) | |
| Treatment: exercise | |||||
| Yes | 29 | (18.4) | 129 | (81.6) | 0.606 |
| No | 50 | (16.4) | 254 | (83.6) | |
| Treatment: oral antidiabetics | |||||
| Yes | 59 | (16.8) | 292 | (83.2) | 0.868 |
| No | 17 | (17.5) | 80 | (82.5) | |
| Treatment: insulin | |||||
| Yes | 18 | (25.3) | 53 | (74.7) | 0.045 |
| No | 61 | (15.6) | 330 | (84.4) | |
| Anthropometricsa | |||||
| Weight (kg) | 74.3 | (20.5) | 71 | (17.0) | 0.108 |
| Height (cm) | 159.5 | (12.0) | 157 | (14.0) | 0.298 |
| BMI (kg/m2) | 29.7 | (6.5) | 28.4 | (6.5) | 0.200 |
| Abdominal circumference (cm) | 98 | (10.0) | 98 | (15.0) | 0.885 |
| Blood glucose and lipid profilea | |||||
| Glucose (mg/dL) | 131 | (100.0) | 130 | (72.0) | 0.286 |
| Cholesterol (mg/dL) | 187 | (60.0) | 184.5 | (54.0) | 0.744 |
| Triglycerides (mg/dL) | 98 | (10.0) | 153 | (96.0) | 0.105 |
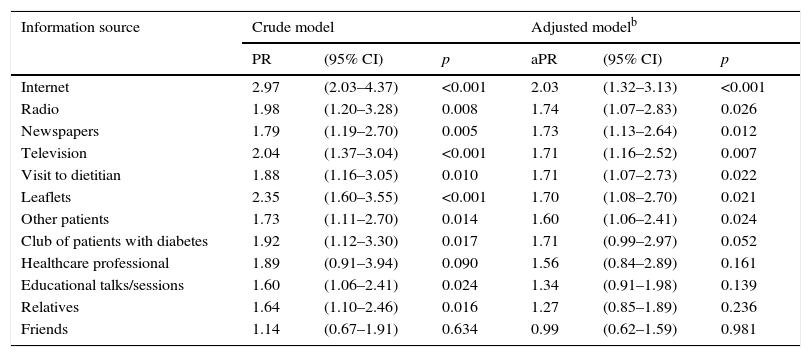
The magnitude of the individual association of each information source with a knowledge of diabetes at both crude and adjusted (by demographic variables) levels may be seen in Table 4, which shows that obtaining information about diabetes through the Internet, radio, newspapers, television, dietitians, educational materials, and other patients was associated with a greater knowledge of diabetes (p<0.05).
Association between each information sourced and the level of knowledge regarding diabetes in crude and adjusted models, Center for the Integral Care of Diabetes and Hypertension, EsSalud, Lima (Peru), 2014 (n=464).a
| Information source | Crude model | Adjusted modelb | ||||
|---|---|---|---|---|---|---|
| PR | (95% CI) | p | aPR | (95% CI) | p | |
| Internet | 2.97 | (2.03–4.37) | <0.001 | 2.03 | (1.32–3.13) | <0.001 |
| Radio | 1.98 | (1.20–3.28) | 0.008 | 1.74 | (1.07–2.83) | 0.026 |
| Newspapers | 1.79 | (1.19–2.70) | 0.005 | 1.73 | (1.13–2.64) | 0.012 |
| Television | 2.04 | (1.37–3.04) | <0.001 | 1.71 | (1.16–2.52) | 0.007 |
| Visit to dietitian | 1.88 | (1.16–3.05) | 0.010 | 1.71 | (1.07–2.73) | 0.022 |
| Leaflets | 2.35 | (1.60–3.55) | <0.001 | 1.70 | (1.08–2.70) | 0.021 |
| Other patients | 1.73 | (1.11–2.70) | 0.014 | 1.60 | (1.06–2.41) | 0.024 |
| Club of patients with diabetes | 1.92 | (1.12–3.30) | 0.017 | 1.71 | (0.99–2.97) | 0.052 |
| Healthcare professional | 1.89 | (0.91–3.94) | 0.090 | 1.56 | (0.84–2.89) | 0.161 |
| Educational talks/sessions | 1.60 | (1.06–2.41) | 0.024 | 1.34 | (0.91–1.98) | 0.139 |
| Relatives | 1.64 | (1.10–2.46) | 0.016 | 1.27 | (0.85–1.89) | 0.236 |
| Friends | 1.14 | (0.67–1.91) | 0.634 | 0.99 | (0.62–1.59) | 0.981 |
95% CI: 95% confidence interval; PR: prevalence ratio; aPR: adjusted prevalence ratio.
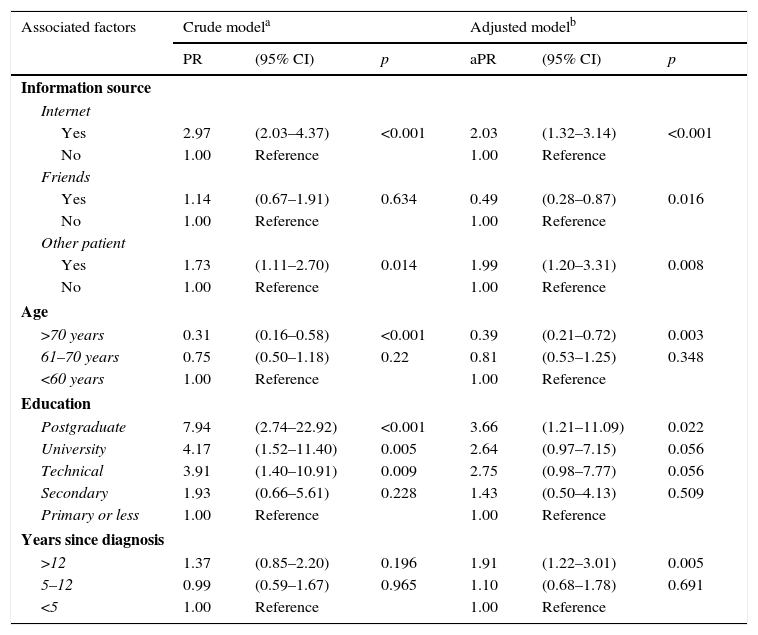
Finally, factors associated with a good level of knowledge of diabetes were identified by using a model initially including all measured variables, which were removed one by one until the optimal model was achieved (Table 5). People who obtained information about diabetes through the Internet (PR=2.03; 95% CI 1.32–3.14) or from other patients (PR=199; 95% CI 1.20–3.31) were the most likely to have a good level of knowledge regarding diabetes, while the opposite occurred with those who asked friends for information (PR=0.49; 95% CI 0.28–0.87). On the other hand, people with postgraduate education (PR=3.66; 95% CI 1.21–11.09) and disease duration longer than 12 years (PR=1.91; 95% CI 1.22–3.01) were more likely to have a good level of knowledge, while patients older than 70 years (PR=0.39; 95% CI 0.21–0.72) were likely to be less well-informed.
Factors associated with a good level of knowledge of diabetes in patients with this disease attending the Center for the Integral Care of Diabetes and Hypertension, EsSalud, Lima (Peru), 2014.
| Associated factors | Crude modela | Adjusted modelb | ||||
|---|---|---|---|---|---|---|
| PR | (95% CI) | p | aPR | (95% CI) | p | |
| Information source | ||||||
| Internet | ||||||
| Yes | 2.97 | (2.03–4.37) | <0.001 | 2.03 | (1.32–3.14) | <0.001 |
| No | 1.00 | Reference | 1.00 | Reference | ||
| Friends | ||||||
| Yes | 1.14 | (0.67–1.91) | 0.634 | 0.49 | (0.28–0.87) | 0.016 |
| No | 1.00 | Reference | 1.00 | Reference | ||
| Other patient | ||||||
| Yes | 1.73 | (1.11–2.70) | 0.014 | 1.99 | (1.20–3.31) | 0.008 |
| No | 1.00 | Reference | 1.00 | Reference | ||
| Age | ||||||
| >70 years | 0.31 | (0.16–0.58) | <0.001 | 0.39 | (0.21–0.72) | 0.003 |
| 61–70 years | 0.75 | (0.50–1.18) | 0.22 | 0.81 | (0.53–1.25) | 0.348 |
| <60 years | 1.00 | Reference | 1.00 | Reference | ||
| Education | ||||||
| Postgraduate | 7.94 | (2.74–22.92) | <0.001 | 3.66 | (1.21–11.09) | 0.022 |
| University | 4.17 | (1.52–11.40) | 0.005 | 2.64 | (0.97–7.15) | 0.056 |
| Technical | 3.91 | (1.40–10.91) | 0.009 | 2.75 | (0.98–7.77) | 0.056 |
| Secondary | 1.93 | (0.66–5.61) | 0.228 | 1.43 | (0.50–4.13) | 0.509 |
| Primary or less | 1.00 | Reference | 1.00 | Reference | ||
| Years since diagnosis | ||||||
| >12 | 1.37 | (0.85–2.20) | 0.196 | 1.91 | (1.22–3.01) | 0.005 |
| 5–12 | 0.99 | (0.59–1.67) | 0.965 | 1.10 | (0.68–1.78) | 0.691 |
| <5 | 1.00 | Reference | 1.00 | Reference | ||
95% CI: 95% confidence interval; PR: prevalence ratio; aPR: adjusted prevalence ratio.
Most participants (83%) had a poor level of knowledge, with only a little over half the questions being adequately answered on average. The mean knowledge score was 12.9±4.8, not very different from the results of other studies conducted on patients with characteristics similar to our study sample. In Jalisco, patients from urban areas had a mean knowledge score of 13.65±3.2814; the mean recorded in another study in the same province was 13.09±3.44.14
Results different to these have also been reported. Thus, the mean knowledge score in a study conducted in 40 patients with diabetes from the southeastern United States, was 6.27±3.03,15 and the score reported in a sample of 30 patients with diabetes from a podiatric clinic in the United States was 18.53±0.78.16 The reason for this latter result could have been that the patients were attending a specialized clinic, and could therefore have obtained a better education in diabetes complications. Our study confirmed this possibility, as patients with longer disease duration had greater knowledge.
On the other hand, the study allowed for a general overview of the information sources to which patients attending the Center for the Integral Care of Diabetes and Hypertension had access. Of those information sources, defined as those sources from which the surveyed patients obtained their knowledge of the disease, the ones particularly associated with a good level of knowledge were the Internet and other patients. Another study showed that receiving information about health from healthcare professionals, friends, family, newspapers, journals, and the Internet was positively associated with knowledge regarding diabetes. The use of television as a source of health information showed mixed results,17,18 while in this study it was not associated with a good level of knowledge after adjustment for Internet use had been made.
The Internet really has revolutionized the search for medical information. Thus, a European study conducted in seven countries showed that the number of adult Internet users who searched health information had increased by 22.6% in males and by 9.8% in females.19 Patients with diabetes in the United States download information online on conditions, treatment options, practical strategies for disease management in their daily life, and disease promotion. However, this information may be erroneous or from unreliable sources.20 A study conducted at a national hospital in Peru found that the use of information technologies (mobile phones or computers) is limited, but is perceived positively as a support for the education of patients with diabetes.21 An additional study showed that elderly subjects who use new technologies have a greater sense of empowerment regarding their disease and greater self-efficacy and well-being as compared to those who do not use them.22
Similarly, another study concluded that younger elderly subjects (aged 60–70 years) are strongly motivated to use the Internet, which should result in the coming decade to current stereotypes regarding the use of technologies by this age group becoming outdated. However, the fact that the design of websites is not adapted to the physical and mental problems associated with aging remains a barrier to access.10,23
The study found an inverse association between information obtained from friends and the level of knowledge, which suggests the importance of strategies in diabetes education for patients and their immediate social environment, so that treatment adherence by patients is supported and relatives and friends are educated in disease prevention.10
Information sources not associated with a good level of knowledge, such as healthcare professionals, diabetes education sessions, and radio, were also found. Healthcare professionals have a predominant role in patient education, but education is not possible in clinical practice because of the overwhelming number of patients, the short time available for care at the clinic, and the long intervals between patient visits, which may lead to the appropriate treatment either not being begun or once begun, not or not adequately followed up, i.e. so-called clinical inertia.24,25 There are then two possible scenarios: a first scenario where clinical inertia, combined with lack of time, may prevent professionals from providing the information and training needed, and a second scenario where the information given by professionals during educational sessions merely goes over old ground and so does not contribute to an increase in knowledge, in which case more participative educational sessions or talks should be organized to provide valuable times and spaces for genuine patient education and the prevention of future complications.
Educational sessions on diabetes have been shown to improve treatment adherence26; however, most patients with diabetes never have access to or never attend formal diabetes education due to communication and other failures in health systems or to behavioral barriers.27 As a result, only a limited number of patients have access. It is also important to determine the number of education sessions attended by patients, because low attendance only leads to inadequate knowledge.
The study allowed us to divide the participants into two groups: those who actively searched for information, and those who received information passively. For the first group, who had a greater level of knowledge, the Internet represented an important information source for the management of diabetes, while the second group was characterized by having press, television, and leaflets as passive information sources28 and, consequently, a lower level of knowledge. This emphasizes the importance of implementing strategies for increasing patient awareness of diabetes by encouraging them to look for reliable sources of information on the Internet using both computers and mobile phones, and to update further information as it becomes available.23
Finally, adequate knowledge of diabetes was associated with higher educational levels, a family history of diabetes, older age, and longer time since diagnosis. Our findings agree with those of prior studies.4,12,29,30
The study has limitations. First, it was a cross-sectional study, so that only an association could be found, but not a causality; it may however be used to generate new studies. Second, all patients belonged to EsSalud and were therefore people with a relatively high education level and middle class socioeconomic status, and it is, therefore, very likely that the overall level of knowledge in the Peruvian population is considerably lower. Finally, information sources were evaluated in general, but not over time. It was thus not possible to assess the impact of each source on knowledge. Additional studies are needed. Despite this, we think that the results achieved may be used to support future efforts to improve the knowledge of patients with diabetes and their relatives regarding the disease.
Increased use of the Internet as an educational tool would allow for the provision and more adequate use of healthcare resources, and visit time could be more effective, as clinical meetings with patients with diabetes could be used for taking decisions regarding those websites that best meet the needs of the patient.18,21
The role of new technologies is seen as an expanding area of knowledge18; because of this, people do not only use computers as a means of acquiring updated information, but increasingly use smart phone applications, social networks, or other virtual and mobile platforms to access information related to health.10 Thus, in order to improve the tranmission of knowledge to patients with diabetes, it is urgent to use greater technological resources that may be accessed virtually and/or through mobile devices, to change the structure of clinical visits and educational sessions, and to do this with the collaboration of health systems.
In conclusion, patients with diabetes who attend the Center for the Integral Care of Diabetes and Hypertension have a low level of knowledge regarding diabetes mellitus. Searching for information on the Internet and information provided by other patients were found to be positively associated with a good level of knowledge. Other factors associated with the level of knowledge were age, time since diagnosis, and educational level.
These results suggest the need to teach patients with diabetes how to search for adequate and reliable information that may support their choices and the management of their disease. Professionals in health systems should also be made aware of the great importance of using the Internet and other easily accessed technological resources as a learning strategy, so providing interactive spaces where patients with diabetes may obtain fully reliable answers to their questions.
FundingThis study was self-funded.
Authors’ contributionKC, JAJ, and PMT designed the study; KC, JAJ, and MT conducted the study; PMT performed data analysis; KC and JAJ wrote the manuscript; PMT and MT made critical contributions to the content, and all authors approved the final version of the study.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Cántaro K, Jara JA, Taboada M, Mayta-Tristán P. Asociación entre las fuentes de información y el nivel de conocimientos sobre diabetes en pacientes diabéticos tipo 2. Endocrinol Nutr. 2016;63:202–211.