Papillary thyroid carcinoma has been defined as a malignant epithelial tumor that shows evidence of follicular differentiation and is characterized by papilla formation and/or a set of characteristic nuclear changes.1 Papillary carcinoma is the most common thyroid neoplasm and accounts for 50–90% of differentiated follicular cell thyroid carcinomas.2 Most of them are diagnosed between 30 and 50 years of age, and they predominantly occur in females. Approximately one third of patients have clinically evident adenopathies at presentation. Only 1–7% of patients have distant metastases at the time of diagnosis. Approximately 15% of patients experience recurrent disease, and an even lower proportion (5%) have a fatal prognosis.3
We report the case of a 51-year-old male patient with a history of respiratory tract infection who was diagnosed with pulmonary tuberculosis at 28 years (for which the patient adequately completed treatment) and with left pneumothorax 15 years earlier, and who was an active smoker of 60 cigarettes daily.
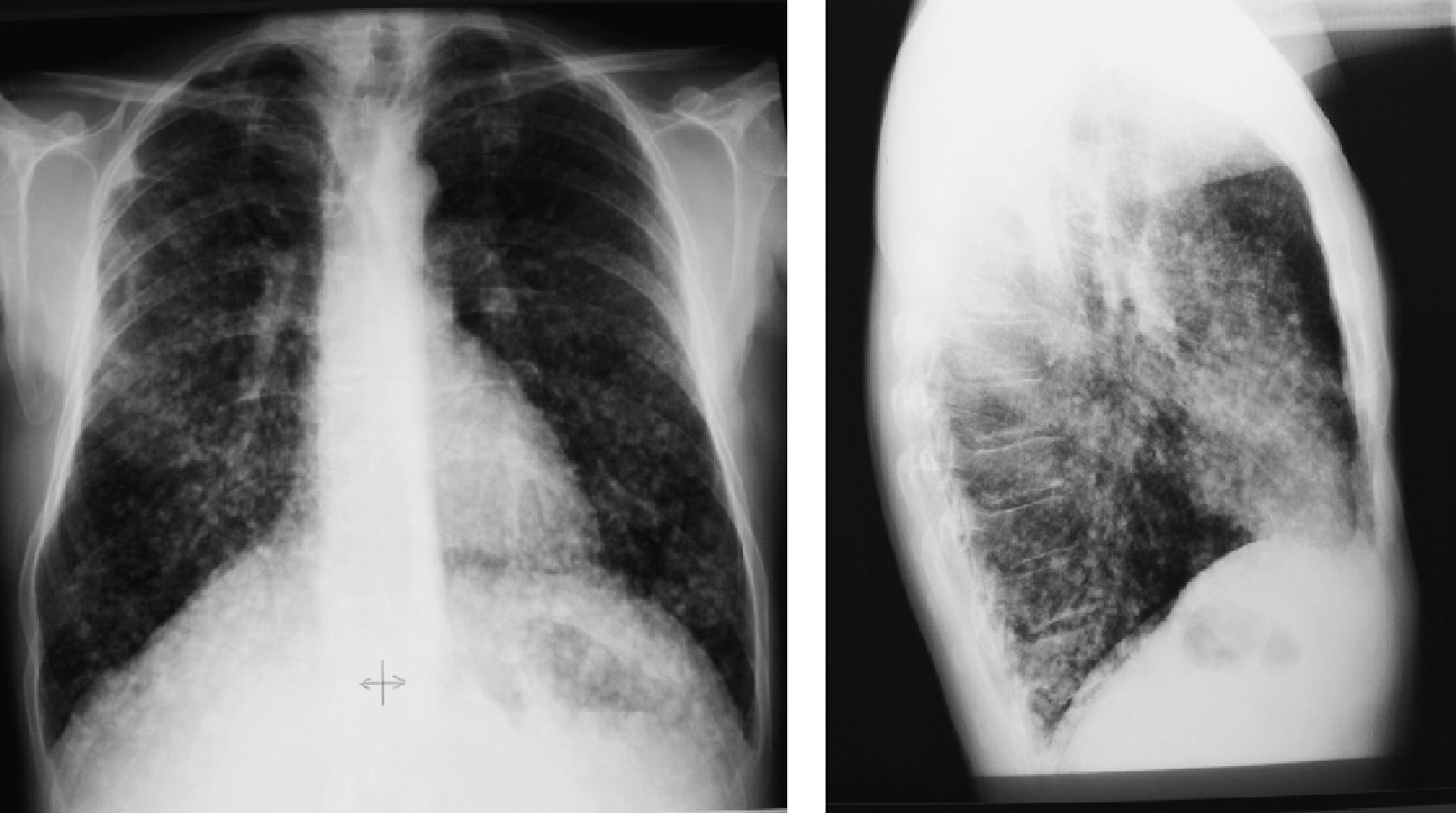
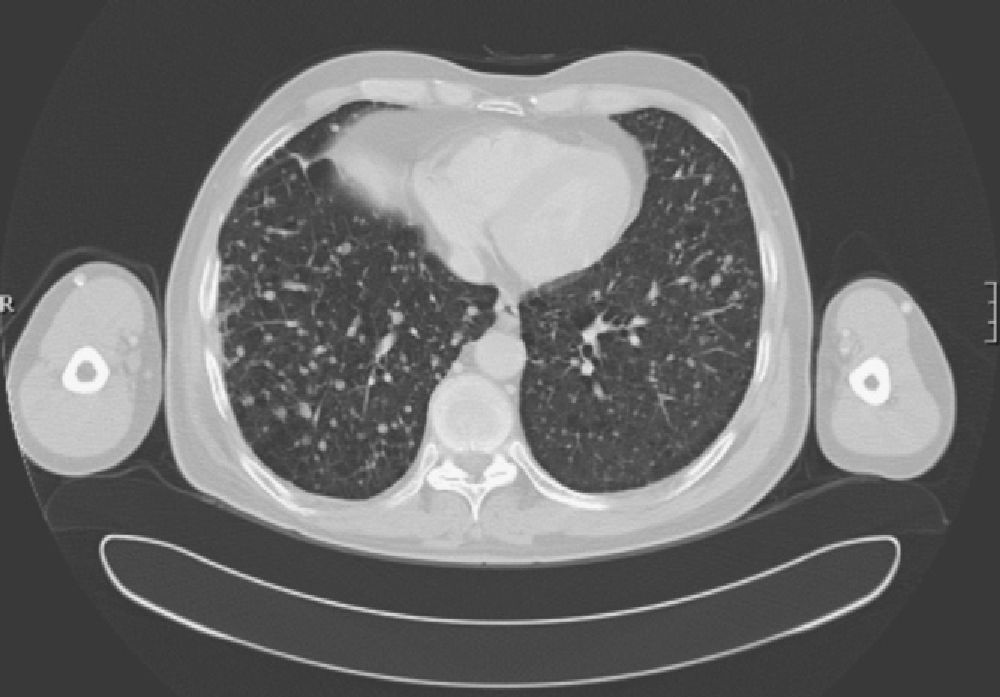
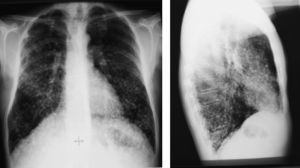
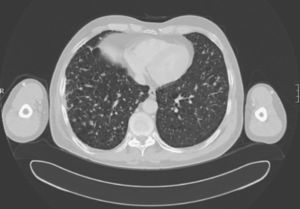
He was admitted to the infectious diseases department of the hospital for joint and muscle pain during the previous year. In the physical examination, an adenopathy approximately 3cm in diameter was palpated in the right side of the neck. Chest X-rays revealed multiple lung nodules. Given the patient's history, miliary tuberculosis was suspected. A complete work-up consisting of chemistry, bacilloscopy, and bronchial aspirate was negative for infection. A chest X-ray upon admission showed bilateral pulmonary nodules, mainly at the lung bases, and a condensation image each at the upper right and left lobes. A chest CT revealed a spiked nodule at the posterior segment of the upper right lobe, as well as a second nodule at the posterior segment of the left lobe. Multiple bilateral pulmonary nodules were seen in the middle and lower fields. There were also nodules in the right side of the neck, in the area adjacent to the sternocleidomastoid muscle.
PET/CT showed radiotracer uptake by the two nodules described in the CT report, located at the posterior segment of both upper lobes. None of the other nodules showed uptake.
Based on the results of the different tests, an active tuberculous infection was considered unlikely. A neoplastic condition was therefore suspected, and puncture of the upper left nodule, transbronchial biopsy of the right middle lobe, and puncture of the dominant cervical adenopathy were requested.
Pathological examination of the pulmonary nodule revealed the presence of cells of large cell lung cancer. However, the results of transbronchial biopsy and adenopathy puncture were consistent with metastases from an as yet undiagnosed papillary thyroid carcinoma.
Thyroid ultrasound examination revealed a partly calcified tumor, 29×13×14mm in diameter, occupying the lower half of the right thyroid nodule, and multiple metastatic adenopathies.
To sum up, this patient had lesions consistent with nodal and pulmonary metastases from an undiagnosed papillary carcinoma, and two pulmonary images which suggested synchronous primary lung neoplasms.
Elective surgery of both dominant pulmonary nodules and the thyroid tumor in a second stage was performed. Biopsy of both lung specimens confirmed synchronous, intermediately differentiated primary carcinomas sparing the surgical resection margins. There were no adenopathies. The tumor was thyroglobulin-negative (T2 N0 M0, stage II). A subsequent total thyroidectomy found a right posterior thyroid nodule that had invaded the recurrent and the right perichondrium. The superior mediastinal lymph nodes involved and lymph nodes of the right recurrent and right internal jugular chains were excised. Bilateral central lymph node dissection and functional dissection of the right lateral cervical lymph nodes were performed. A pathological examination revealed a multifocal, mixed papillary and follicular non-encapsulated thyroid carcinoma with infiltrating margins that had invaded the thyroid capsule, soft tissue, and perithyroid lymphatic and blood vessels, and metastasized to multiple mediastinal and right jugular lymph nodes (T4a N1b M1, stage IV C).
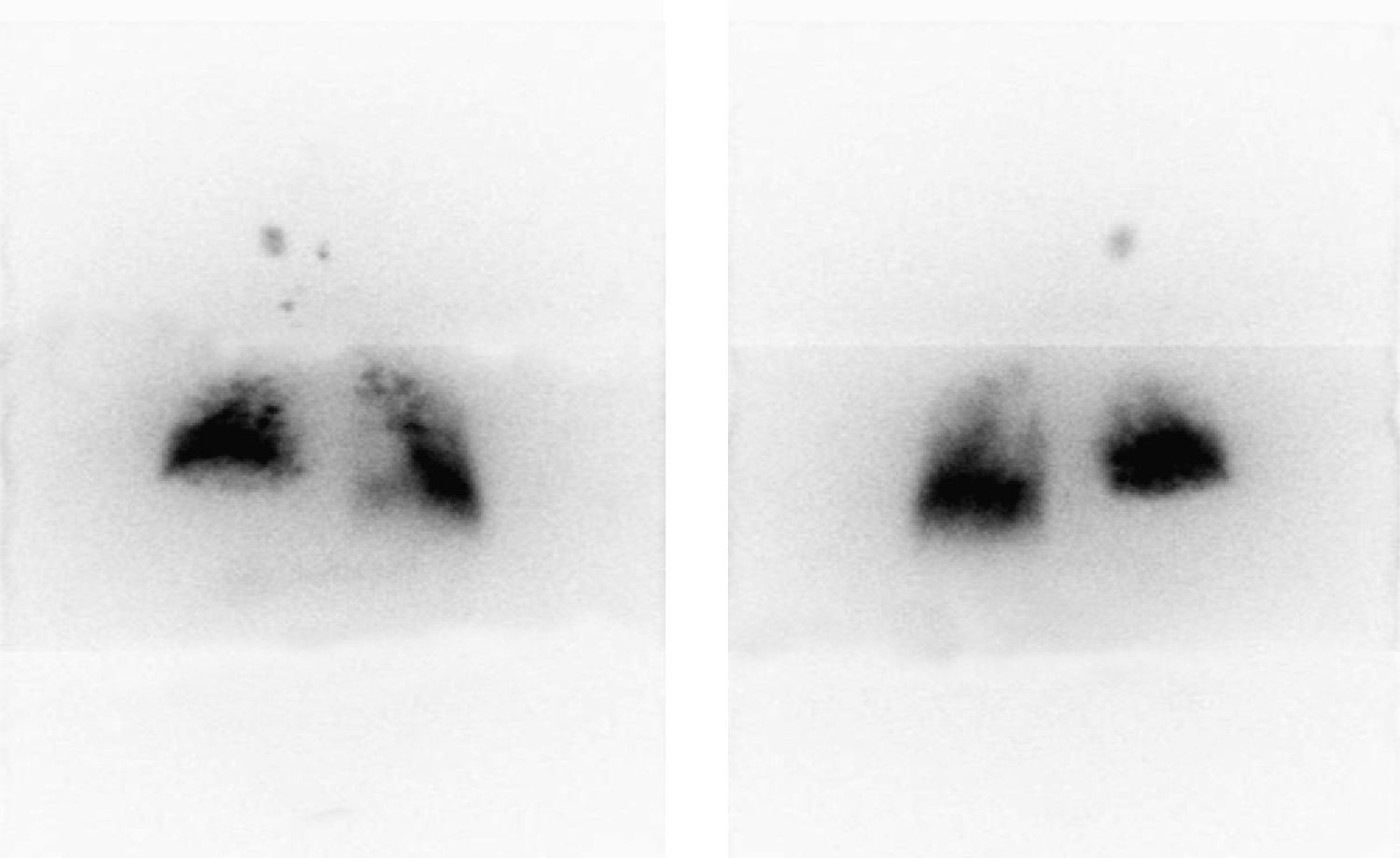
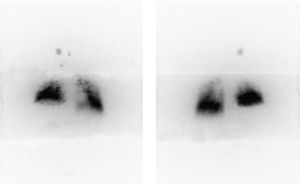
A whole body scan with 123I after stimulation with recombinant TSH disclosed bilateral thyroid remnants, a metastatic adenopathy in the right side of the neck, and generalized, predominantly basal, metastatic lung disease (Fig. 1). Thyroglobulin levels of 4830ng/mL with negative antithyroglobulin antibodies were found.
Because of his multiple conditions, which involved surgery for two synchronous lung tumors and with severe centrilobular emphysema and extensive metastatic lung involvement from his thyroid tumor, the patient was evaluated by the department of physics and radioprotection, which contraindicated the use of 131I because of the risk of acute pneumonitis, with subsequent respiratory failure that would be life-threatening.
After discussion with the oncological department six months after surgery, palliative chemotherapy with the antiangiogenic drug sorafenib, a tyrosine kinase inhibitor, was decided upon. The patient did not tolerate regular cycles due to the occurrence of hand-foot syndrome. Subsequent controls with chest X-rays (Fig. 3) and CT scans every six months (Fig. 4) showed no nodule changes or decreases in thyroglobulin levels. The last value found on suppressant therapy was 1,921ng/mL with negative antithyroglobulin antibodies.
Only 1–7% of patients with papillary thyroid carcinoma have distant metastases at diagnosis.3 Clinical symptoms of lung involvement are not common. The involvement pattern may range from macronodular to diffuse infiltrates. The latter pattern, when undetected in the chest X-ray, is usually diagnosed using a 123I whole body scan, and may be confirmed with a spiral CT. Almost all patients have high serum thyroglobulin levels despite the fact that lung metastases are not visible in X-rays. In our patient, lung micrometastases were visualized from the start, but were not initially interpreted as such. Clinical records corresponding to the patient's previous stay at the hospital for tuberculosis were requested. Chest X-rays were then reviewed (Figs. 2 and 3) and were seen to be similar to the current X-ray films, taken 23 years later. Thus, the patient already had at that time the metastatic micronodular lung infiltrate, which in the setting of clinical respiratory signs was interpreted as an infectious process, while these new findings suggested, although it could not be categorically stated, that it was a metastatic lung disease of a thyroid origin. The very slow development in this case of a tumor that had remained silent for years should be noted. It should be stressed that the patient had not consulted a specialist during this time.
Treatment with 131I for 6–12 months was advised for micrometastases, in the knowledge that that complete remission could be achieved with doses higher than 200mCi.4
Lung macrometastases are also treated with 131I if they are shown to take up the radioactive agent. In this case, it was possible to decrease thyroglobulin levels and size. However, it should be noted that complete remission is rarely achieved.5
Complications of treatment with high doses of 131I include pneumonitis and pulmonary fibrosis. If these are suspected, lung function should be assessed and may limit treatment continuation.6
If lung metastases do not take up 131I, chemotherapy (cisplatin, doxorubicin) may be given, with its attendant risk of toxicity and low response.7 Partial remission is achieved in 15% of patients.
Treatment with antiangiogenic agents such as tyrosine kinase inhibitors (axitimib, motesanib, and sorafenib) is under investigation, but they have many side effects, including arterial hypertension, diarrhea, fatigue, skin erythema and rash, and weight loss.8–12
Please cite this article as: Cabrejas Gómez MdC, et al. Carcinoma papilar de larga evolución. Endocrinol Nutr. 2012;59:69–83.