Non-pancreatic gastrointestinal neuroendocrine tumors (NETs) include a wide group of diseases mainly located in the ileum and appendix and usually with no clinical signs of hormone hypersecretion. At least 140 cases have been reported in the ampulla of Vater, whose symptoms usually derive from ampullar obstruction and include abdominal pain, pancreatitis, jaundice, or gastrointestinal bleeding.
Locoregional nodal metastatic involvement, unrelated to tumor size and not leading to a poorer prognosis, is found in half of these tumors at diagnosis.
Cervical nodal involvement by occult intra-abdominal neoplasms (Troisier's sign), particularly gastric or pancreatic adenocarcinomas, has been known for longer than a century. We report an ampullar NET in which the first sign was a metastatic cervical adenopathy.
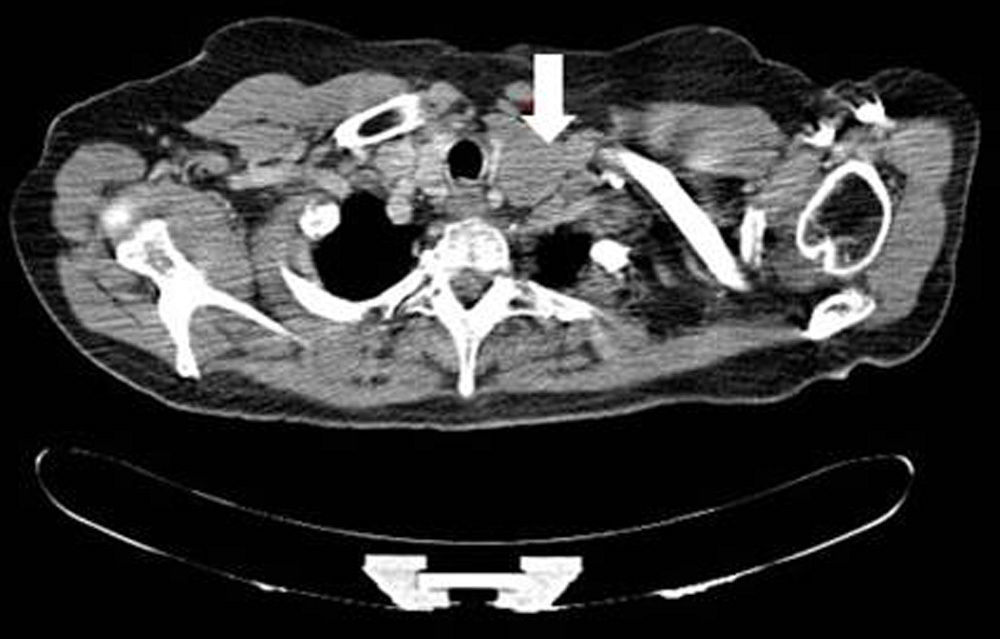
A 59-year-old woman attended the clinic for a palpable mass in the left side of the neck with no other symptoms. A computed tomography (CT) of the neck showed a 4-cm adenopathy in the left side of the neck that compressed the left thyroid lobe (Fig. 1). Biopsy showed a lymph node infiltrated by a well differentiated NET with immunohistochemistry (IHC) positive for chromogranin A (CgA) and synaptophysin and negative for calcitonin. Thyroid ultrasonography showed no changes.
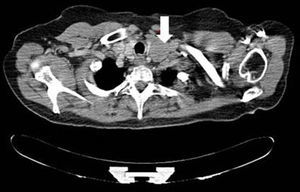
Laboratory tests showed normal serum levels of neuroendocrine tumor markers (CgA, gastrin, PP, somatostatin, glucagon, and calcitonin), and elevated transaminase and alkaline phosphatase levels (AST 75U/L, NR<32; ALT 82U/L, NR<32; γGT 1167U/L, NR<33; FA 279U/L, NR<36) and normal bilirubin. Abdominal CT revealed a dilated bile duct (15mm) with prominent papilla, with no tumor or luminal occupation and pancreatic duct dilation (Fig. 2). An endoscopic ultrasonography showed a hypoechoic mass in the duodenal ampulla with periportal adenopathies up to 24mm in size. Tumor biopsy and adenopathies showed a NET.
A cephalic pancreatoduodenectomy (Whipple operation) with regional lymph node resection showed a neuroendocrine tumor 1.7×1.4cm in size that invaded the duodenal mucosa and pancreas, with peripancreatic, preaortic, and mesenteric lymphatic and nodal involvement (17/23). Microscopically, the condition characterized by proliferation of small rounded cells with a solid pattern and 2 mitoses/10 high power fields. IHC found a low cell proliferation index (Ki67<2%) with positive neuroendocrine markers (CgA, synaptophysin); other hormones were not tested by IHC due to technical problems. One month later, a left functional cervical dissection showed 9/41 lymph nodes involved, up to 4.5cm in size.
A postoperative 111-octreotide scan showed nodal uptake at peripancreatic and superior mediastinal level, with bone involvement in the 7th costovertebral joint, confirmed by bone scan.
Patient continues to be symptom-free after two years, with gradual elevation of serum CgA level (NR×3) in the last year, lesion stabilization in T7 and occurrence of a new lesion in L5, with adenopathy enlargement. No treatment has been started yet.
The Troisier sign refers to left lateral neck adenopathies occurring as the initial sign of an intra-abdominal malignant tumor due to lymphatic dissemination through the thoracic duct. Ampullar NETs are exceptional tumors, with less than 140 cases reported, accounting for less than 2% of malignant tumors in the ampulla and 0.3% of gastrointestinal NETs.1–3 We have found no reported case with this presentation.
NET incidence and prevalence rates have increased in recent years, probably because of improved diagnostic procedures.1,4 Mean age at diagnosis of ampullar NETs is 58 years, and tumors are more prevalent in males.1,4 Twenty-five percent of cases are related to von Recklinghausen syndrome.2,4,5
The most common signs and symptoms of ampullar NETs are jaundice (60%), abdominal pain (40%), and pancreatitis (6%), with weight loss and gastrointestinal bleeding occurring less commonly.2,4,6 Carcinoid syndrome is uncommon, except in the presence of liver metastases.2
The 2010 histopathological staging of the World Health Organization is the most adequate classification for prognosis of these tumors,1 and recent studies suggest an association between greater biological aggressiveness of the tumor and possibility of distant metastases with higher Ki-67 index.2
Non-specific neuroendocrine tumor cell markers (chromogranin A, specific neuronal enolase, and synaptophysin) are positive in almost all ampullar NETs studied (92%, 100%, and 100% respectively). As regards specific hormone production markers, not tested in our patient, the most common is somatostatin (58–67%), followed by insulin (25%), serotonin (17%), and CCK (17%).1,2,5
The diagnostic procedure of choice for locating primary tumor is endoscopic retrograde cholangiopancreatography (ERCP). ERCP and endoscopic ultrasonography (EUS) allow for assessing the possibility of infiltration into the bile ducts. EUS has high sensitivity for small tumors or local angioinvasion. CT and MRI have little sensitivity for diagnosis of primary lesion, being useful for showing metastases in the liver, mainly in the early arterial phase,7 or in the mesentery; depending on clinical signs and course, other imaging tests such as bone scan, octreoscan, PET, or MIBG should be performed.1–3
Standard treatment consists of cephalic pancreatoduodenectomy (Whipple operation). Endoscopic ampullectomy may be a viable option for treating selected cases with highly differentiated carcinomas confined to the mucosa without vascular or lymphatic invasion.2,6
In the reported series, tumor size did not correlate to tumor potential to metastasize to lymph nodes.1,2,4–6 Coexistence of locoregional nodal metastases (50% at diagnosis) has shown no impact on disease-free survival or on perineural or venous involvement. Factors correlated to poorer prognosis include local tumor extension (serosa, pancreas, retroperitoneum, and other adjacent tumors), size>2cm, and high mitotic grade (G3).1,2,4–6
Five- and 10-year survival rates are 82% and 71% respectively, but lower for high grade tumors (15% at 5 and 10 years). The recurrence rate is 40–50%, and metastases mainly occur in the liver.1,2,8
The reported case is interesting because of a number of unusual characteristics. This was a rare presentation, at an advanced stage, of an uncommon tumor with a silent course until self-detection of the adenopathy. Despite the fact that the tumor was less than 2cm in size and had a Ki-67 less than 2%, there was widespread nodal and bone metastatic involvement with no evidence of liver involvement, which is most common in dissemination of these tumors.
Please cite this article as: Calles LA, Iglesias Eider Etxeberría N, Goñi F, Paja M. Adenopatía cervical como presentación de ampuloma neuroendocrino. Endocrinol Nutr. 2014;61:493-495.