Measurement of thyroid-stimulating hormone (TSH) is the most helpful test for the diagnosis and monitoring of primary hypothyroidism.1 However, it may sometimes provide conflicting and confusing results.
We report the case of a 45-year-old woman who underwent work-up for elevated TSH levels. Tests performed for asthenia and mild fatigue for the previous few months found a TSH level (chemoluminescence assay [IMA], AccessDXI 800 BECKMAN COULTER® [Fast hTSH]) of 142μIU/mL (0.34–5.6) and a free thyroxine (FT4) level of 7.76pg/mL (5.8–16.4). Subclinical primary hypothyroidism was suspected, and replacement therapy was started with levothyroxine (L-T4) 50μg/day. Repeat tests at six months showed a TSH level of 129μIU/mL and a FT4 level of 9.89pg/mL, with no changes in subjective symptoms reported by the patient. The dose of L-T4 was increased to 100μg/day, and three weeks later, TSH and FT4 levels were 115μIU/mL and 14.09pg/mL respectively.
No significant findings were made in the physical examination. The patient had a weight of 62kg and a height of 163cm, and thyroid palpation was normal. Neck ultrasound examination showed two non-suspicious nodules less than 1cm in size, and antithyroid autoantibodies were negative. Results of all other routine laboratory tests were normal, except for cholesterol levels: total cholesterol 268mg/dL, HDL-C 38mg/dL, and LDL-C 201mg/dL.
Based on an initial suspicion of L-T4 underdosage, the dose was increased to 125μg/day. Six weeks later, TSH and FT4 levels were above the normal reference limit: 72μIU/mL and 17.0pg/mL respectively. When asked about treatment compliance, both the patient and her family reported adequate intake and adherence.
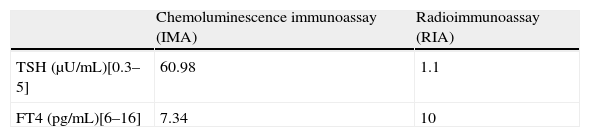
Since FT4 had gradually increased, while TSH levels continued to be much higher than normal, the differential diagnosis was expanded. Complete tests of hypothalamic-pituitary function were requested, and TSH was measured by radioimmunoassay (RIA), a procedure different from the one previously used. Test results included: TSH, 0.08μIU/mL (0.4–5); FT4, 18pg/mL (6–17); total T3, 106ng/dL (90–175); prolactin, 368μU/mL (100–410); LH, 20mU/L; FSH, 38mU/L; estradiol, 34pg/mL; ACTH, 27pg/mL (9–54); and basal cortisol, 87ng/mL (65–210). The discrepancy in TSH measurement was confirmed when a sample taken on the same day was processed using both procedures, IMA and RIA (Table 1A).
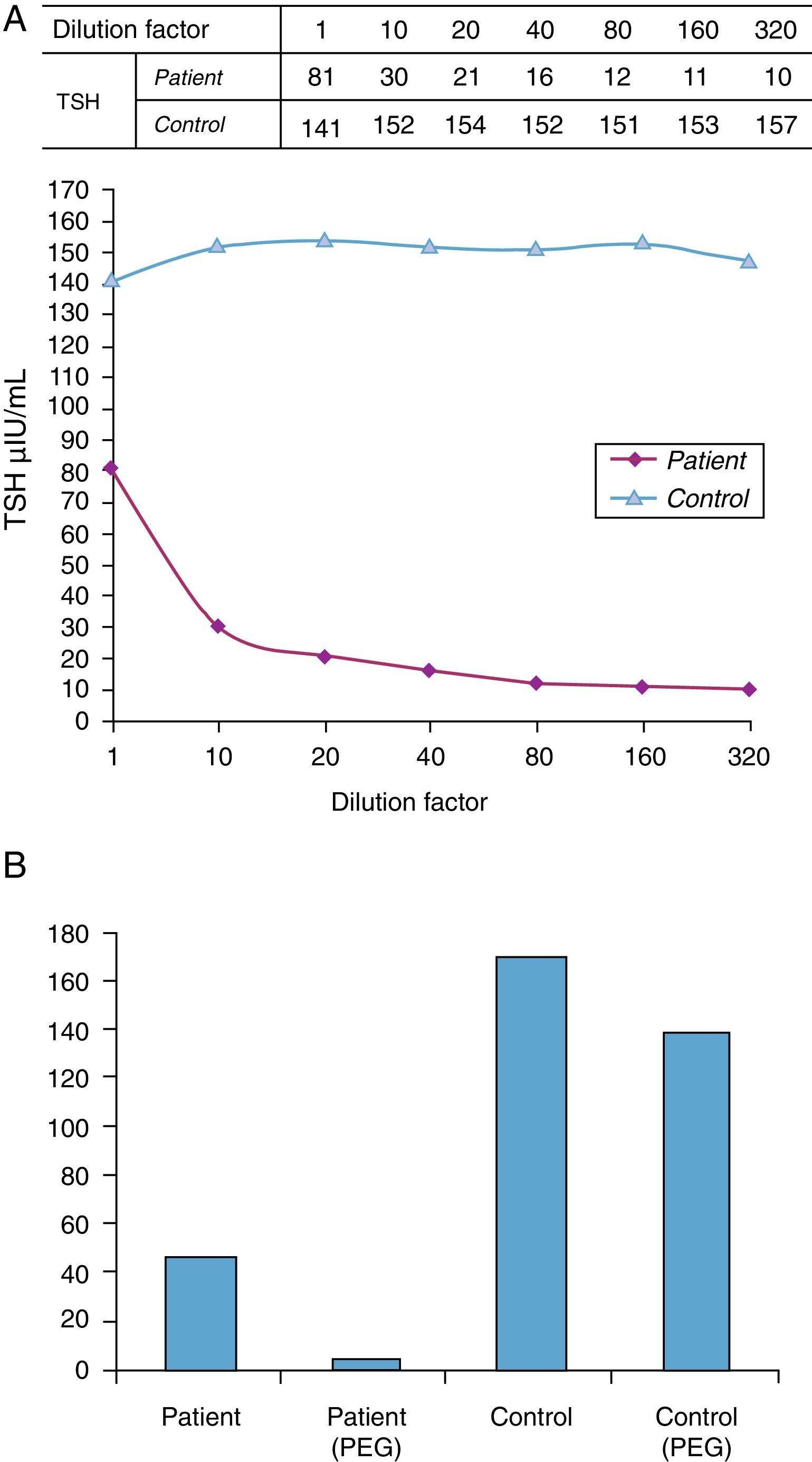
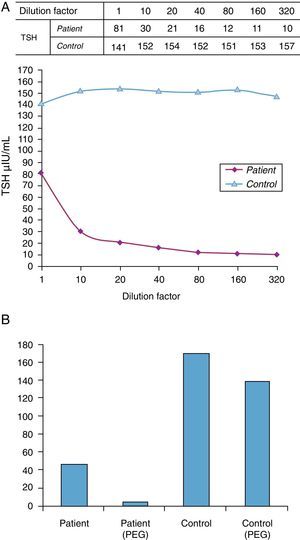
Such apparently paradoxical results led to the tests recommended by the National Academy of Clinical Biochemistry (NACB) Laboratory Medicine Practice Guidelines being performed to assess the potential interference with immunochemical measurements.2 Serial dilutions first showed a lack of parallelism with a control sample (Fig. 1A). A subsequent test on the same sample with a method from another manufacturer (Cemtauro BAYER®) reported a TSH level of 3.2μIU/mL (0.3–5), which represented a difference greater than 50% as compared to the previous result. Finally, a polyethylene glycol (PEG) precipitation test was done. This is a nonspecific procedure that allows for proteins to be separated by decreasing their solubility until they precipitate. When PEG is applied to serum, precipitation is quite specific for immunoglobulins and their complexes, and all forms of interference by antibodies may therefore be identified. Percent recovery after precipitation with PEG was only 7%, which suggested the existence of an interferent (Fig. 1B).
(A) Linearity test using serial dilutions. The behavior of the analyte in the sample is compared to that of the analyte in another sample. Lack of parallelism between the two samples may be due to the presence of an interferent. (B) Precipitation test with polyethylene glycol (PEG). Percent recovery was 85% in the control and 7% in the patient.
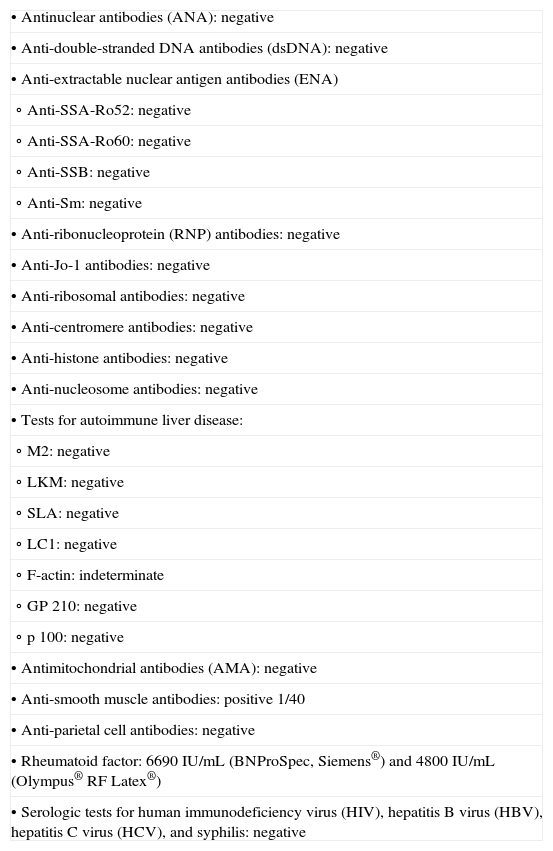
Based on these results and in order to identify the interferent, serologic and autoimmunity tests were performed in the patient (Table 1B). A rheumatoid factor level of 6690IU/mL (normal, <20) was found, despite the fact that the patient had no sign or symptom suggesting a rheumatological condition.
Serologic and autoimmunity testing of the patient.
| • Antinuclear antibodies (ANA): negative |
| • Anti-double-stranded DNA antibodies (dsDNA): negative |
| • Anti-extractable nuclear antigen antibodies (ENA) |
| ∘ Anti-SSA-Ro52: negative |
| ∘ Anti-SSA-Ro60: negative |
| ∘ Anti-SSB: negative |
| ∘ Anti-Sm: negative |
| • Anti-ribonucleoprotein (RNP) antibodies: negative |
| • Anti-Jo-1 antibodies: negative |
| • Anti-ribosomal antibodies: negative |
| • Anti-centromere antibodies: negative |
| • Anti-histone antibodies: negative |
| • Anti-nucleosome antibodies: negative |
| • Tests for autoimmune liver disease: |
| ∘ M2: negative |
| ∘ LKM: negative |
| ∘ SLA: negative |
| ∘ LC1: negative |
| ∘ F-actin: indeterminate |
| ∘ GP 210: negative |
| ∘ p 100: negative |
| • Antimitochondrial antibodies (AMA): negative |
| • Anti-smooth muscle antibodies: positive 1/40 |
| • Anti-parietal cell antibodies: negative |
| • Rheumatoid factor: 6690IU/mL (BNProSpec, Siemens®) and 4800IU/mL (Olympus® RF Latex®) |
| • Serologic tests for human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), and syphilis: negative |
The dose of L-T4 was adjusted to 50μg/day, and one month later the patient showed an analytical euthyroid state (TSH 3.8μU/mL by RIA, although the value found by IMA was 81.66μU/mL, and FT4 7.79pg/mL) and clinical improvement.
When high TSH levels are found, the most common diagnosis is primary hypothyroidism, which is initially considered to be subclinical if FT4 levels are still within normal limits.1,3 If test results are confirmed, replacement therapy should be started with L-T4, with dose adjustment based on the progressive normalization of TSH after some weeks.4
If TSH elevation continues despite replacement therapy, potential interference with hormone absorption such as, for example, the concomitant intake of other drugs or intestinal malabsorption should be considered, and adequate treatment compliance should be verified.4 Specifically, acute L-T4 intake by a noncompliant patient before a clinical visit will increase FT4, but will not normalize the serum TSH level. In the reported case, the patient and her relatives reported adequate compliance, and interference with absorption was not considered because FT4 increased as replacement therapy was increased.
Another apparently paradoxical cause of dissociation between FT4 and TSH is the syndrome of inappropriate TSH secretion, comprising two conditions: TSH secretion by a pituitary adenoma and non-neoplastic TSH hypersecretion due to a resistance to thyroid hormones. Both conditions were unlikely in our case, because FT4 elevation occurred when replacement therapy was started, not from the beginning. Moreover, these clinical conditions are not usually associated with such marked TSH elevations.5,6
An additional factor to be ruled out was the existence of laboratory artifacts due to the presence of interferents7 or macro-TSH.8 Tests currently used to measure TSH are highly sensitive and specific, but if heterophile antibodies or rheumatoid factors exist, bridges may be formed between capture and signaling antibodies, generating a false signal that causes an inappropriately high analyte value.9 This is more evident in immunometric tests, and the manufacturers of reagents have therefore used various procedures to circumvent the problem, with variable results.10
In most cases, interference is due to heterophile antibodies, which may show a prevalence of 0.2–15% in the general population.11 However, to our knowledge, only one case of interference by rheumatoid factor has been reported.12 This autoantibody may be present in both healthy subjects and patients with rheumatological disease, but since it is not routinely measured, it is difficult to identify it as being responsible for the interference with TSH measurement13 and its incidence cannot be clearly established. Because of the high frequency of rheumatoid factor and other heterophile antibodies in the general population, interferences with TSH measurement are likely to be more common than expected.
It is therefore advisable to consider potential interference by rheumatoid factor or other heterophile antibodies in patients with discordances between TSH/FT4 and clinical signs. This possibility must be taken into account because, despite improved immunometric tests, it remains an unsolved problem. In these cases, measurement of TSH by an alternative method may be helpful in diagnosis, thus avoiding unnecessary repeat tests and preventing inadequate treatment approaches which are not free from side effects.
Please cite this article as: Ramos-Leví AM, et al. Cuando la analítica desconcierta: interferencia en la determinación de tirotropina debido a factor reumatoide. Endocrinol Nutr. 2013;60:342–5.