Rosai-Dorfman disease (RDD) or sinus histiocytosis with massive lymphadenopathy, is a rare disease of unknown origin histologically characterized by the infiltration of abundant lymphocyte-containing histiocytes (emperipolesis) within the lymph nodes.1 Forty percent of patients may have signs outside the lymph nodes, of which skin involvement is the most common. Its location within the thyroid gland is unusual, with only 9 cases reported to date.2–5
We report the case of a 58-year-old woman admitted in October 2010 to the department of neurology for clinical manifestations suggesting stroke, including unstable gait, generalized weakness, left hemiparesis, right deviation of conjugate gaze, and decreased consciousness. Following initial improvement in the first week of admission, the patient experienced acute confusion, being unable to recognize her relatives. The patient had a history of primary hypothyroidism and received replacement therapy with levothyroxine 50μg/day starting in September 2010. Upon admission, thyroid gland test results were as follows: TSH 5.51mIU/mL (reference range 0.55–4.78mIU/mL); free T4 14.38pmol/L (10–20pmol/L); peroxidase antibodies>1000IU/mL (0–35IU/mL); and thyroglobulin antibodies 61.9IU/mL (0–40IU/mL). Both blood immunological testing (ANA, anti-DNA, ENA, anticardiolipin, and ECA) and HIV and RPR proved negative. Thyroid gland ultrasound revealed a hypoechogenic nodule measuring 22mm×20mm in size located in the left thyroid lobe, together with another nodule measuring 11mm located in the right lobe, and multiple bilateral lateral neck adenopathies—the largest measuring 17mm in size—without evidence of malignancy. During admission, an ischemic vascular process was ruled out based on CT and MRI of the brain, which only showed an altered signal in the supratentorial white matter consistent with nonspecific leukopathy, with no signs of acute ischemic disease. The electroencephalogram showed a nonspecific decrease in electrical activity. Cerebrospinal fluid tests revealed a slight increase in protein levels, while the other parameters and the culture were negative. Thyroid antibodies were not measured. Treatment was started with prednisone 50mg/day, followed by a good clinical and radiological response. Based on the foregoing, and after other possible etiologies had been eliminated, the case was tentatively diagnosed as autoimmune corticosteroid-responsive encephalitis associated with autoimmune thyroiditis or Hashimoto's encephalopathy, despite the fact that this disease entity is highly controversial in the medical literature.
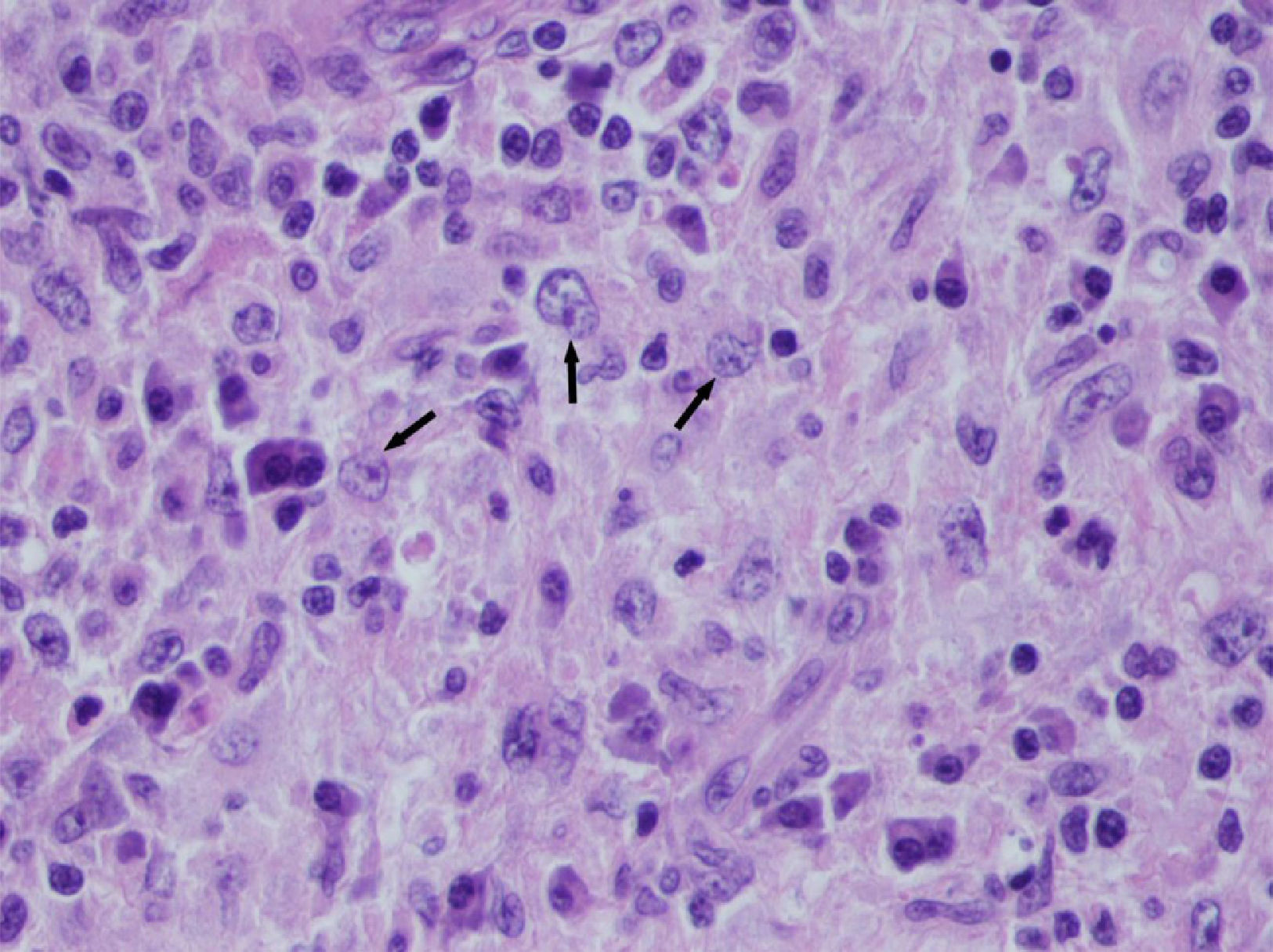
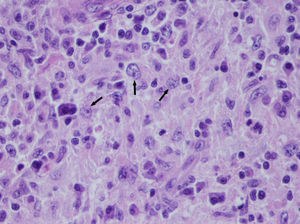
Outpatient endocrine monitoring was started, consisting of thyroid laboratory tests, neck ultrasonography, and two successive fine needle aspirations (FNAs) of the dominant nodule. The cytological findings were consistent with Hashimoto's chronic lymphocytic thyroiditis. After thyroid function was normalized with 75μg/day of sodium levothyroxine, the patient showed a progressive increase in size of the thyroid nodules. In February 2014 she developed compressive symptoms and intense pain on mobilizing the neck. Ultrasound exploration at this time showed an increase in thyroid size at the expense of a nodule in the left lobe measuring over 5cm in diameter, with a significant bilateral increase in size of the lateral neck adenopathies already noted on the occasion of the previous exploration. A repeat FNA showed signs of granulomatous lymphadenitis. A differential diagnostic study of granulomatous peripheral adenopathies was carried out by Internal Medicine using bacterial and viral serological tests (PPD and PCR for tuberculosis, HIV, HCV, HBV, CMV, Toxoplasma gondii, Treponema pallidum, Chlamydia trachomatis, Yersinia spp. and Bartonella quintana), tumor markers and autoimmune markers—all of which proved negative. In view of the lack of a specific diagnosis, an adenopathy was removed for histological study, which revealed granulomatous lymphadenopathy with microabscesses. Nine months later, a new ultrasound of the neck showed a sustained enlargement of the entire thyroid gland, of a nodular appearance, with a bilateral increase in size of the lateral neck adenopathies. Thyroidectomy and lymphadenectomy were indicated. A pathological examination of the surgical specimen found a thyroid gland in which the parenchyma had been almost totally replaced by a histiocytic infiltrate. The histiocytes had large nuclei and cytoplasm, with the presence of intact lymphocytes within the cytoplasm (emperipolesis) (Fig. 1). The histological diagnosis was consistent with nodal and thyroid involvement by RDD, together with Hashimoto's thyroiditis in the scant remaining thyroid gland tissue. The extension study was completed with a physical examination of the lymphatic territories and thoracoabdominal CT, performed during admission and showing no changes outside the neck region.
RDD or sinus histiocytosis with massive lymphadenopathy is an uncommon form of histiocytosis of unknown origin. Histiocytosis has an incidence of 1–3 cases per million inhabitants, and RDD is one of its least common subtypes. Histiocytes are immune system cells that include macrophages and dendritic cells, among others. The pathophysiology of this condition consists of progressive histiocyte occupation of the lymph node sinusoids, with the resultant loss of the normal lymph node architecture. In addition to lymphocytes, other cells such as erythrocytes and plasma cells can also be found within the cytoplasm of the histiocytes—a phenomenon referred to as emperipolesis.6 Although lymphocyte phagocytosis is not a specific feature, it is a constant phenomenon of considerable diagnostic importance. Emperipolesis may also be found in other conditions such as malignant melanoma, Hodgkin's disease, and other types of histiocytosis. Immunohistochemical studies are required to establish a differential diagnosis. In RDD, the histiocytes are seen to be positive for CD68 and S100. Negative epithelial markers such as CAM 5.2 make it possible to rule out carcinoma metastasis, while a negative result for CD1a and langerin excludes Langerhans histiocytosis. In our case, the immunohistochemical findings were consistent with the described diagnosis.
A retrospective evaluation of the initial samples (FNA and neck lymph node biopsy) showed that they were inadequate to establish a correct diagnosis because of the scant material available and the absence of emperipolesis.
The incidence of endocrine gland involvement in RDD is low, though cases have been described involving the adrenal glands,7 the hypophysis,8 the pancreas9 and the thyroid gland. The final diagnosis is always made based on histological and immunohistochemical findings. Moreover, patients with RDD should have an extension study performed to rule out the involvement of other lymph node territories or tissues, because these findings may modify the management strategy. There is no agreement as to what constitutes adequate treatment because of the scant available scientific evidence, itself attributable to the low incidence of the disease. In a review published in 2014, Dalia et al., having considered the most widely used therapeutic measures, developed a management algorithm.1 Watchful waiting is usually advised in asymptomatic patients, with surgical resection in those with localized disease, and the administration of glucocorticoids or immunosuppressants in patients with systemic or disseminated disease as the most frequent treatment options.
Please cite this article as: Palmas Candia F, Porras Ledantes JA, Raventós Estellé A, Simón Muela I, Vendrell Ortega J, Näf Cortés S. Afectación tiroidea por enfermedad de Rosai-Dorfman. Endocrinol Diabetes Nutr. 2017;64:280–281.