Although, it is generally held that the levothyroxine (LT4) dose tends to decrease with age, this theory remains controversial. Our objective was to assess whether the LT4 dose required to achieve euthyroid status varies according to age, body weight (BW), sex, menopausal status, or antibody status.
Materials and methodsA cross-sectional study was performed from the retrospective review of the charts of patients with a previous diagnosis of primary hypothyroidism in treatment with LT4 and in a euthyroid state. Sex, age, actual body weight (ABW), TSH, and LT4 dose were recorded. Patients were grouped according to age ranges (18–44, 45–65, and over 65 years). A euthyroid state was defined as a serum TSH within the range of 0.4–4μIU/ml. A multiple linear regression model was performed to assess the LT4 dose and age, gender, antibody status, and ABW.
ResultsA total of 882 charts of patients were reviewed. 586 patients met the inclusion criteria. The median age was 55 years. There was no correlation between the LT4 dose and age. A positive correlation was observed between the LT4 dose and ABW, but not with the ideal BW. Linear regression analysis showed that positivity antibody and ABW have a significant effect on the LT4 dose. Comparison of the LT4 dose between the different age groups showed no difference.
ConclusionOur study demonstrates that the dose of LT4 necessary to achieve euthyroidism is influenced by ABW and the presence of antibodies. Age and menopause did not influence the required daily dose of LT4.
Existe un concepto de que la dosis de levotiroxina (LT4) tiende a disminuir con la edad. Sin embargo, hay controversia al respecto. Nuestro objetivo fue evaluar si la dosis de LT4 requerida para alcanzar el estado eutiroideo varía según la edad, el peso corporal, el sexo, el estado de la menopausia y el estado de los anticuerpos.
Materiales y métodosSe realizó un estudio transversal a partir de la revisión retrospectiva de historias clínicas de pacientes con diagnóstico previo de hipotiroidismo primario en el tratamiento con LT4 y en estado eutiroideo. Se registraron sexo, edad, peso corporal actual (PCA), TSH y dosis de LT4. El estado eutiroideo se definió como una TSH sérica dentro del rango de 0,4-4 μUI/mL. Se realizó un modelo de regresión lineal múltiple para evaluar la dosis de LT4 y la edad, el sexo, el estado de los anticuerpos y el PCA.
ResultadosSe revisaron un total de 882 cuadros de pacientes. Quinientos ochenta y seis pacientes cumplieron los criterios de inclusión. La mediana de edad fue de 55 años. No hubo correlación entre la dosis de LT4 y la edad. Se observó una correlación positiva entre la dosis de LT4 y el PCA, pero no con el PC ideal. El análisis de regresión lineal demostró que los anticuerpos positivos y el PCA tienen un efecto significativo sobre la dosis de LT4. La comparación de la dosis de LT4 entre los diferentes grupos de edad no arrojó diferencias.
ConclusiónNuestro estudio demuestra que la dosis de LT4 necesaria para lograr el eutiroidismo está influenciada por el PCA y la presencia de anticuerpos. La edad y la menopausia no influyeron en la dosis diaria requerida de LT4.
Hypothyroidism is a common condition resulting from deficiency of thyroid hormones.1,2 The prevalence of hypothyroidism varies according to the region. Some studies also suggest the incidence of hypothyroidism is higher in older age groups, starting at about 60 years of age, or at least that hypothyroidism is being treated more frequently in older age group.3
It is now well established that while tetraiodothyronine (T4) is the major secretory product of the thyroid gland, thyroid hormone action in peripheral tissues is due to the effects of triiodothyronin (T3) binding to its nuclear receptor, defining T4 as a pro-hormone for T3. Levothyroxine (LT4) has been considered the standard of care for treatment of hypothyroidism for many years, and is recommended as the preparation of choice due to its efficacy in resolving the symptoms of hypothyroidism, long-term experience of its benefits, favorable side effect profile, ease of administration, good intestinal absorption, long serum half-life, and low cost. Based on body weight, hypothyroid patients with minimal endogenous thyroid function require LT4 doses of 1.6–1.8μg/kg/day of actual body weight,4–6 although some studies estimate higher doses of 2.0–2.1μg/kg/day for some patient groups.7,8 Two studies have shown that ideal body weight is a better predictor of LT4 dose than actual body weight,9,10 thus suggesting that LT4 dose requirement may depend on lean body mass.
TSH serves as a surrogate marker of euthyroidism. It is assumed to be an integrated measure of how the individual pituitary–thyroid axis responds to prevailing free thyroxine (fT4) levels. Achieving a serum TSH that is within the normal age adjusted reference interval is desirable for all patients.5
The etiology of a patient's hypothyroidism affects his dose of LT4 probably reflecting the amount of residual functional thyroid tissue.6 There is a general concept that LT4 replacement dose tend to decrease with age, but this could be influenced by actual body weight, lean body weight, sex, or menopausal state.11,12 However, there is controversy in the literature.
Our objective was to assess whether the LT4 dose required to achieve euthyroid status varies according to age, body weight, sex, menopausal status, and antibody status.
Materials and methodsStudy designA cross-sectional study was performed from the retrospective review of charts of adult patients over 18 years of age from four Endocrinology services in the cities of Rosario and Casilda (Argentina) during the period of time between January 2017 and December 2019. Approval from the teaching and ethics committee was obtained before the study began.
SubjectsAll patients older than 18 years, of both sexes, with previous diagnosis of primary hypothyroidism in treatment with LT4, non-thyroidectomized, in euthyroid state and with a stable dose of LT4 during the last six months were included.
Patients with primary hypothyroidism who were not euthyroid, hypothyroidism after thyroidectomy, pregnant or lactating women, patients with a history of thyroid cancer, central hypothyroidism, follow-up and/or irregular treatment were excluded from the study. Patients under treatment amiodarone, lithium, proton pump inhibitors, iodine, iron or calcium supplements, patients with severe chronic diseases (congestive heart failure, NYHA III-IV congestive heart disease, hypercapnia and/or hypoxemia lung disease, chronic kidney disease), pituitary disease and/or malabsorptive gastrointestinal diseases (celiac disease, inflammatory bowel disease, lactose intolerance, bariatric surgery) were also excluded from the analysis.
Data collectionSex, age, actual body weight (ABW) (kg), height (cm), body mass index (BMI), LT4 dose (expressed in μg/day), age of menopause in women, previous hyperthyroidism and radioiodine therapy were recorded. The ideal body weight (IBW) was calculated based on the patient's height using the Devine formula: for women over 152cm, 45kg plus 2.3kg for each additional 2.5cm; for women less than 152cm, 45kg minus 2.3kg for each additional 2.5cm below 152cm; for men over 152cm plus 2.7kg for each additional 2.5cm. The degree of overweight was calculated using the ratio of ABW and IBW.
TSH and thyroid autoantibody status [thyroid peroxidase antibodies (TPOAb) or antithyroglobulin antibody (TgAb)] were recorded. Because some patients had more than one TSH value available during the study period, it was decided to choose the last determination with stable dose of LT4. TSH assays used by the clinical laboratories employed a third-generation ultra-sensitive immunochemiluminometric assay with a sensitivity of 0.01μIU/ml (reference ranges approximately 0.4–4.2μIU/ml).
Euthyroid state was defined as a serum TSH within the range of 0.4–4μIU/ml. The daily dose of LT4 was evaluated based on the ABW and IBW. Patients were grouped according to age ranges in 18–44 years, 45–65 years and over 65 years.
Statistical analysisStatistical software R version 3.6.3 was used. The normality of continuous variables was determined using the Shapiro–Wilk test. The homogeneity of the variances was determined using the Bartlett test. Numerical variables were compared using non-parametric tests (Mann–Whitney for the comparison of two groups and Kruskal–Wallis, post hoc Holm, for the comparison of more than two groups) and the results were expressed as median and interquartile range. Correlations analyses were made with the Spearman correlation coefficient. A multiple linear regression model was performed to assess the daily dose of LT4 and age, gender, antibody status, and BW. Gender was classified into three distinct groups: men, premenopausal women, and menopausal women. Differences were considered significant if p<0.05.
ResultsA total of 882 charts of patients were reviewed. Of this total, 586 patients (533 women and 53 men) met the inclusion criteria. The median age was 55 years (41–67). Of the 533 women, 228 were of reproductive age and 305 were post-menopausal. The status of TPOAb and/or TgAb was verified in 329 patients (194 patients with positive antibodies and 136 patients with negative antibodies). Only 7 (1.19%) patients received radioiodine therapy.
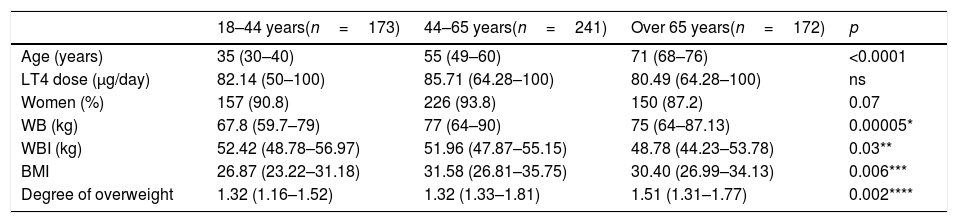
Table 1 shows age, LT4 dose (μg/day) and anthropometric variables according to age range groups.
LT4 dose and anthropometric variables. Kruskal–Wallis.
| 18–44 years(n=173) | 44–65 years(n=241) | Over 65 years(n=172) | p | |
|---|---|---|---|---|
| Age (years) | 35 (30–40) | 55 (49–60) | 71 (68–76) | <0.0001 |
| LT4 dose (μg/day) | 82.14 (50–100) | 85.71 (64.28–100) | 80.49 (64.28–100) | ns |
| Women (%) | 157 (90.8) | 226 (93.8) | 150 (87.2) | 0.07 |
| WB (kg) | 67.8 (59.7–79) | 77 (64–90) | 75 (64–87.13) | 0.00005* |
| WBI (kg) | 52.42 (48.78–56.97) | 51.96 (47.87–55.15) | 48.78 (44.23–53.78) | 0.03** |
| BMI | 26.87 (23.22–31.18) | 31.58 (26.81–35.75) | 30.40 (26.99–34.13) | 0.006*** |
| Degree of overweight | 1.32 (1.16–1.52) | 1.32 (1.33–1.81) | 1.51 (1.31–1.77) | 0.002**** |
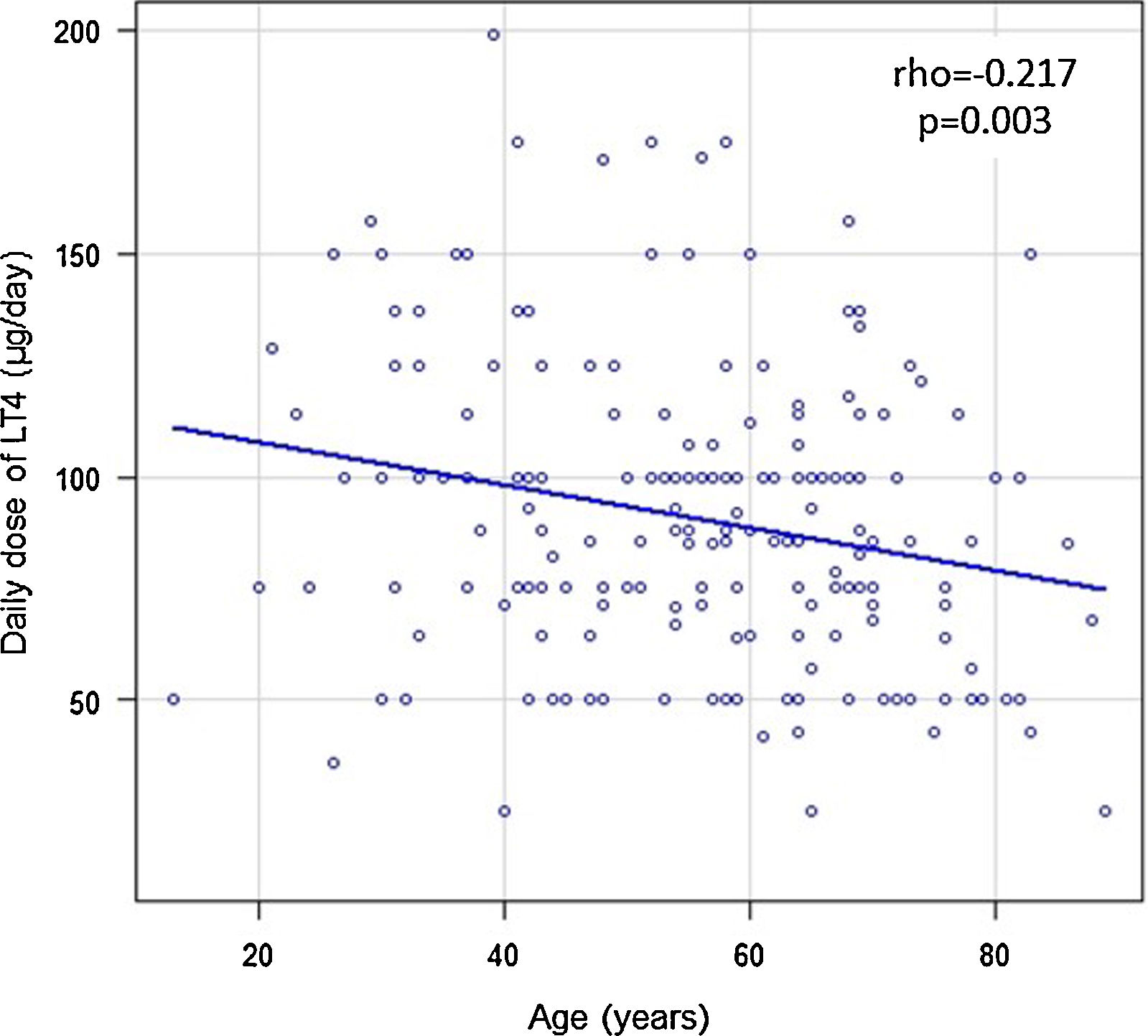
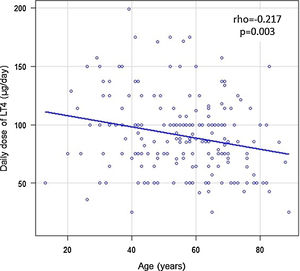
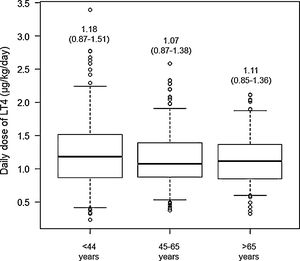
A correlation analysis was performed between the ABW and age of the people, showing a positive correlation (rho=0.118, p=0.004). A positive correlation was also observed between the degree of overweight and age (rho=0.182, p=0.014). There was no correlation between the daily dose of LT4 (μg/day) and age (rho=0.016, p=0.69) in the overall analysis of the patients, but a negative correlation was observed between the daily dose of LT4 (μg/day) and age in those patients with Hashimoto's thyroiditis (Fig. 1).
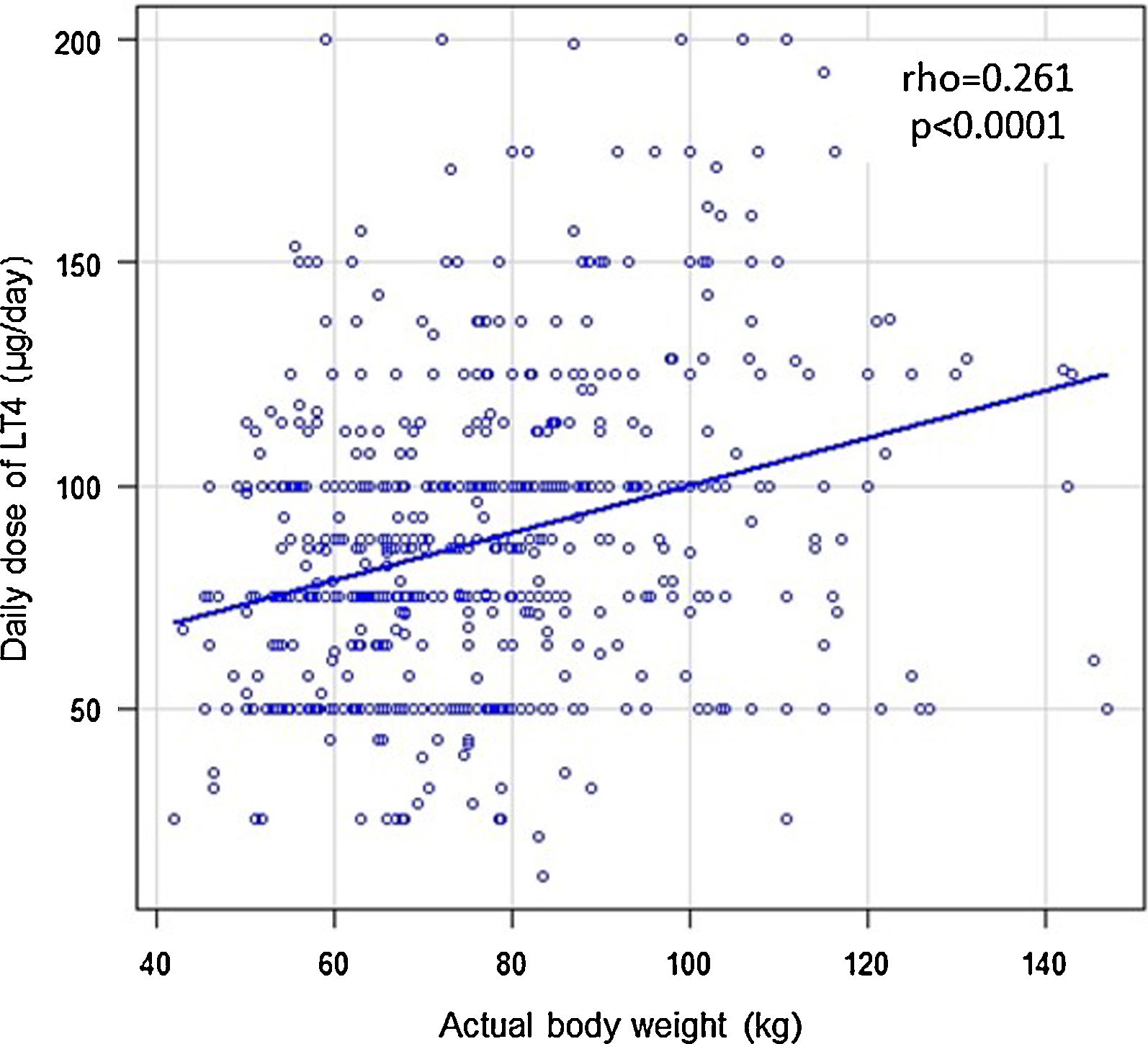
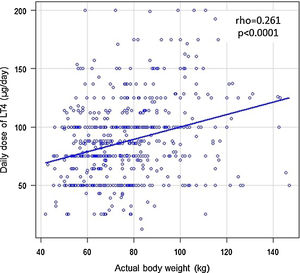
To assess whether the LT4 dose needed to achieve euthyroidism is more convenient to express as a function of ABW or IBW, a correlation analysis was performed. A positive correlation was observed between the absolute daily dose of LT4 and ABW (Fig. 2) but not with the IBW (rho=0.0587, p=0.432). These findings were maintained in the subgroup of patients older than 65 years (daily dose of LT4∼ABW: rho=0.335, p<0.0001; daily dose of LT4∼IBW: rho=0.224, p=0.11).
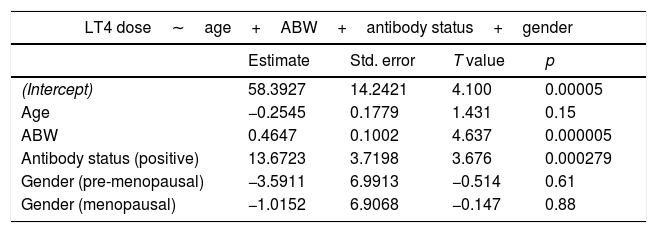
Multiple linear regression analysis was performed to assess the daily dose of LT4 (μg/day) based on age, antibody status, gender, and ABW. The effect of the presence of positive antibodies and the ABW was shown to be statistically significant (Table 2).
LT4 dose according to gender, antibodies, ABW and age. Multiple linear regression.
| LT4 dose∼age+ABW+antibody status+gender | ||||
|---|---|---|---|---|
| Estimate | Std. error | T value | p | |
| (Intercept) | 58.3927 | 14.2421 | 4.100 | 0.00005 |
| Age | −0.2545 | 0.1779 | 1.431 | 0.15 |
| ABW | 0.4647 | 0.1002 | 4.637 | 0.000005 |
| Antibody status (positive) | 13.6723 | 3.7198 | 3.676 | 0.000279 |
| Gender (pre-menopausal) | −3.5911 | 6.9913 | −0.514 | 0.61 |
| Gender (menopausal) | −1.0152 | 6.9068 | −0.147 | 0.88 |
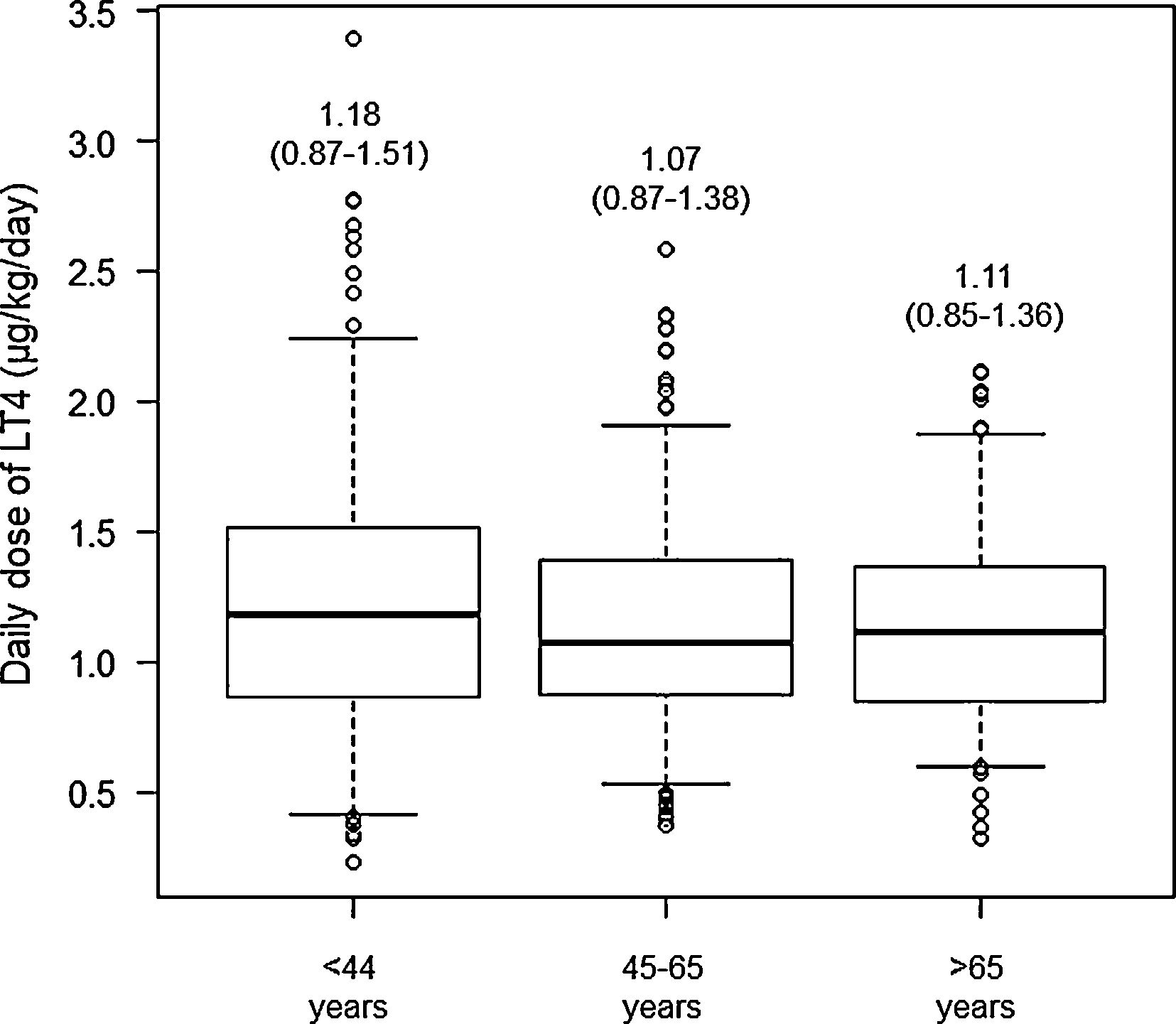
The comparison of the daily dose of LT4 as ABW (μg/kg/day) between the age groups did not show differences (p=0.424) (Fig. 3). No difference in the daily dose of LT4 as ABW was evidenced according to menopausal status [pre-menopausal 1.16μg/kg/day (0.81–1.47) versus menopausal 1.13μg/kg/day (0.91–1.38), p=0.4], nor between women and men [0.97μg/kg/day (0.79–1.45)].
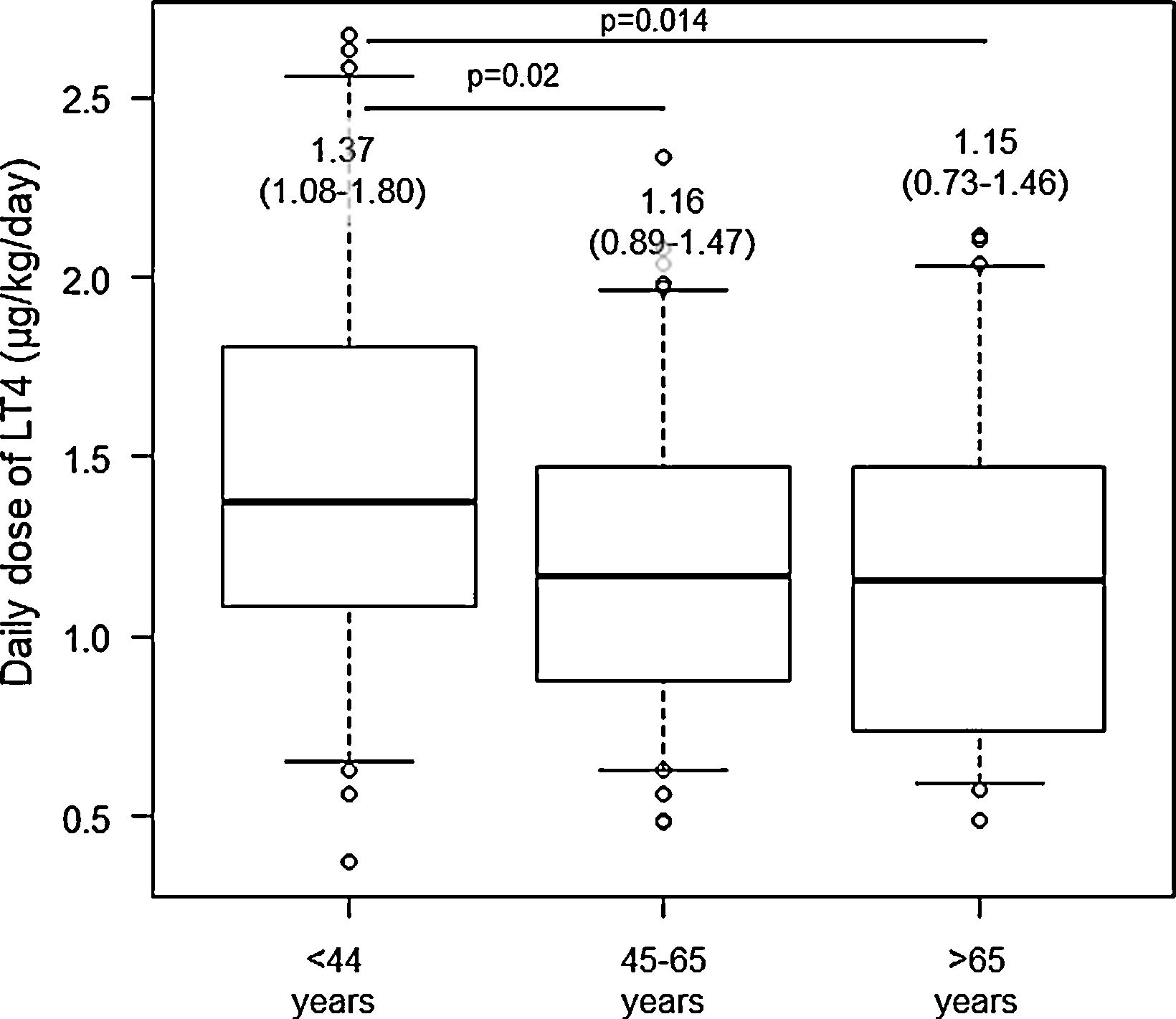
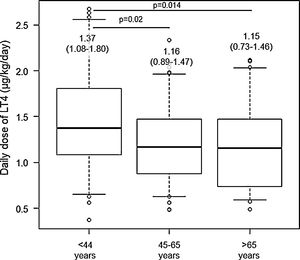
The daily dose of LT4 as ABW (μg/kg/day) was compared according to the state of the antibodies and it was shown that patients with Hashimoto's thyroiditis needed a higher dose [positive antibodies 1.2μg/kg/day (0.86–1.54) versus negative antibodies 1.03μg/kg/day (0.77–1.31), p=0.003]. LT4 dose as ABW was compared according to age groups among patients with Hashimoto's thyroiditis and it was shown that patients in the age range of less than 44 years needed a higher dose to achieve euthyroidism compared to patients between 45 and 65 years and over 65 years (Fig. 4).
DiscussionLT4 has been considered the standard of care for the treatment of hypothyroidism for many years. This treatment is efficacious when administered orally, has a long serum half-life that permits daily administration, and results in resolution of the signs and symptoms of hypothyroidism in the majority of patients. LT4 replacement therapy in primary hypothyroidism has three main goals: provide resolution of the patients’ symptoms and hypothyroid signs, including biological and physiologic markers of hypothyroidism, achieve normalization of serum TSH with improvement in thyroid hormone concentrations, and avoid overtreatment, especially in the elderly.1
Santini et al. studied the relationship between the total daily dose of LT4 and body composition by simple linear regression.9 There was a significant positive correlation between the LT4 dose and total BW. However, the association was much stronger when the LT4 dose was correlated with lean body mass than with fat mass, both measured by dual energy X-ray absorptiometry. Moreover, the gender-related variations of LT4 requirement appear dependent on differences in total BW, with lean mass content having the highest impact. However, our analysis found that the dose of LT4 required to achieve euthyroid status correlates better with ABW, rather than IBW.
It has been suggested that decreased lean body mass or alterations in body composition and/or changes associated with menopause are associated with lower LT4 requirement associated with age.9,10,13,14 However, in our study it was observed that the daily dose of LT4 necessary to achieve euthyroidism does not change according to age.
However, regarding to the effect of age on LT4 requirement, analyses have not always incorporated adjustments for both the BW and sex of patients. One study that adjusted LT4 dose for BW demonstrated that older patients required a lower LT4 dose.7 Therefore, we performed a multiple linear regression analysis considering the age, ABW, gender, and antibody status. We observed that the dose necessary to achieve the euthyroid state is related to the presence of antibodies and ABW, but is not influenced by age, sex, or menopausal status. Furthermore, we did not find differences in the daily dose of LT4 expressed as a function of ABW according to age groups or gender (men, pre-menopausal or menopausal). This contrasts with several studies that show a lower requirement in postmenopausal women and men11,12 and agrees with reports that show that age does not affect the dose of LT4.15
Patients with Hashimoto's thyroiditis required a higher dose to achieve euthyroid state (1.2μg/kg/day versus 1.03μg/kg/day). This is in line with a previous study that demonstrated that weight-based LT4 dose in patients with atrophic thyroiditis (1.26±0.07μg/kg/day) was lower than in patients with Hashimoto's thyroiditis (1.59±0.07μg/kg/day) or hypothyroidism after of radioiodine therapy (1.56±0.05μg/kg/day).8 Likewise, only in the subgroup of patients with Hashimoto's thyroiditis were shown a negative correlation between age and LT4 dose and a higher LT4 requirement based on ABW in the group of patients younger than 44 years. This finding could correspond to previous studies that demonstrated a requirement of 25% less LT4 in adults older than 65 years7; however, in our study, only patients younger than 44 years required a higher dose, with no differences between patients 44 and 65 years and older than 65 years.
The limitations of our study are based on its retrospective nature. This type of design does not allow us to define the presence of symptoms compatible with hypothyroidism independently of a TSH within the normal range, to control the LT4 intake time or to use a centralized laboratory for all determinations. Furthermore, we considered the euthyroid state only according to the TSH level and did not include peripheral hormones (free T4, total T4, and T3) in the analysis. Recently, Lacámara et al. described a novel clinical phenotype of alteration of thyroid hormone metabolism that involves the activation of T4 to T3 and an increase in rT3, compatible with resistance to exogenous thyroxine (RETH).16 These patients are characterized by unresponsiveness levels of TSH despite receiving a high dose of LT4, predisposing to a state of iatrogenic thyrotoxicosis. Although we cannot rule out this clinical scenario, our study only included patients with normal TSH levels. Another limitation is the use of a mathematical formula to estimate the IBW and, consequently, the lean body mass. However, complementary studies to estimate body composition, such as dual energy X-ray absorptiometry cannot be routinely used in medical practice. Similarly, previous studies comparing LT4 dose based on ABW and IBW used formulas similar to Devine's. Finally, our study shows that the dose of LT4 necessary to achieve euthyroidism, even in patients with Hashimoto's thyroiditis, is lower than that reported in previous studies.1 However, this comparison is not part of the objectives of the present study, and future analyzes are required to corroborate this finding.
ConclusionOur study demonstrated that the dose of LT4 needed to achieve euthyroidism correlated more adequately with ABW rather than IBW. Likewise, the dose of LT4 is only influenced by BW and the presence of antibodies. Only in the subgroup of patients with Hashimoto's thyroiditis was a higher LT4 requirement observed in those younger than 44 years.
Conflict of interestThe authors declare no conflicts of interest.