Iodine deficiency is a public health problem, and iodine nutritional status should therefore be regularly measured.
ObjectiveTo ascertain iodine nutritional status in Asturias and its relation to use of iodized salt and to other sociodemographic and nutritional parameters.
Material and methodsA descriptive, observational study was conducted in a random sample of schoolchildren aged 5–14 years, in whom urinary iodine levels were measured by high-performance liquid chromatography. Families completed a survey on use of iodized salt, consumption of dairy products and fish, and sociodemographic data.
ResultsThe study sample consisted of 705 schoolchildren (51.1% females) with a mean age of 9.9 years (SD 2.6). In a total of 620 valid measurements, mean urinary iodine level was 204.1μg/L (SD 120.6), while the median value was 180.7μg/L (P25–P75: 124–252.3μg/L, interquartile range 128.3μg/L). Urinary iodine levels were <100μg/L in 16.6% of children, and very low (<20μg/L) in 0.2%. Iodized salt was used in 69.3% of all households, and in all school canteens. Consumption of dairy products was significantly associated to urinary iodine levels (p<.0005).
ConclusionIodine nutrition of Asturian schoolchildren is adequate, although the target of use of iodized salt in 90% of households is still far away. Adequate iodine nutrition may be due to other sources, such as dairy products. Public health campaigns are required to promote iodized salt consumption. Regular assessment of iodine nutritional status is also needed.
El déficit de yodo es considerado un problema de salud pública. El estado nutricional de yodo de una población debería determinarse periódicamente.
ObjetivoConocer el estado de nutrición de yodo en Asturias y su relación con el uso de sal yodada y con otros parámetros sociodemográficos y nutricionales.
Material y métodosEstudio observacional descriptivo en una muestra aleatorizada de población escolar de 5 a 14 años, determinando yoduria mediante cromatografía líquida de alta resolución. Previamente, la familia de cada niño respondía una encuesta sobre consumo de lácteos, pescado, sal yodada y datos sociodemográficos.
ResultadosSe estudió a 705 escolares (51,1% niñas), con una edad media de 9,9 años (DE 2,6). La yoduria media fue 204,1μg/L (DE 120,6), la mediana 180,7μg/L (P25-P75: 124–252,3μg/L; rango intercuartílico 128,3μg/L), en un total de 620 determinaciones válidas. La proporción de niños con yodurias<100μg/L fue del 16,6% del total y con yodurias muy bajas (<20μg/L) del 0,2%. Se consumía sal yodada en el 69,3% de los hogares y todos los comedores escolares la utilizaban. El consumo de lácteos se relacionó significativamente con la yoduria (p<0,0005).
ConclusiónLa nutrición de yodo en escolares asturianos es adecuada, aunque aún queda lejos el objetivo del 90% de consumo de sal yodada en los hogares. El adecuado estado de nutrición de yodo podría deberse a otras fuentes, como el consumo de lácteos. Son necesarias campañas de salud pública para fomentar el consumo de sal yodada en nuestra población, así como la evaluación periódica del estado nutricional de yodo.
Iodine is a micronutrient of crucial importance for the synthesis of thyroid gland hormones, and iodine deficiency has multiple effects in humans. The problem posed by iodine deficiency classically has been referred mainly to endemic goiter,1 though in recent decades research in different countries has demonstrated that in addition to goiter there are also so-called iodine deficiency disorders (IDDs), including among other conditions increased neonatal mortality and miscarriages, congenital anomalies with permanent neuromotor damage, hearing problems and reduced intellectual capacity and growth.2 In fact, the World Health Organization (WHO) considers iodine deficiency to be the main preventable cause of brain damage in the fetus and nursing infants, and of psychomotor retardation in small children.3
Iodine deficiency is a public health problem of geological origin. It affects an important part of the world population: IDDs are among the most frequent deficiency disorders. Prevention programs targeted to IDDs therefore should be included in all national health policies. On the other hand, the universal iodization of salt is the best strategy for controlling iodine deficiency, and is clearly cost-effective.4
In recent years there have been major advances in the struggle to eradicate iodine deficiency. In 1993 the WHO estimated that IDDs affected 110 countries worldwide,5 while more recent studies estimate that 30 countries have iodine deficiency problems.6 Furthermore, 71% of the world population now has access to iodized salt, compared with only 20% in 1990.7 Since many countries have reached the objective of eliminating iodine deficiency or are close to doing so, current efforts now focus on maintaining this objective. For this purpose, governments should promote periodic iodized salt consumption campaigns, with the regular evaluation of their impact upon the population.8 Children living in areas with iodine deficiency are vulnerable even to short periods of iodized salt suspension.9 As a result, in 2005 the WHO recommended the evaluation of iodine prophylactic programs with a periodicity of at least once every three years.10
The methods used to evaluate iodine deficiency in a population have gradually changed. In this regard, the presence of goiter (widely used in the past) has been replaced by urine iodine concentration and percentage regular consumption of iodized salt in the home.8 In order to consider iodine deficiency to have been eradicated, the WHO, UNICEF and ICCIDD consider it necessary for the following criteria to have been met11: iodized salt must be consumed regularly in over 90% of all homes, and less than 50% of all schoolchildren should have ioduria values of under 100μg/L and less than 20% ioduria values of under 50μg/L.
According to the recommendations of the WHO on the evaluation of iodoprophylaxis programs and their impact, periodic epidemiological studies of the school population are necessary in order to ascertain the current situation regarding iodine nutrition.
The present study has the following objectives:
- 1.
To establish the current iodine nutritional status in Asturias (Spain), by determining ioduria in the school population.
- 2.
To determine whether Asturias meets the WHO recommendations for the eradication of IDDs.
- 3.
To determine whether there are other parameters that could influence iodine nutritional status, apart from the consumption of iodized salt.
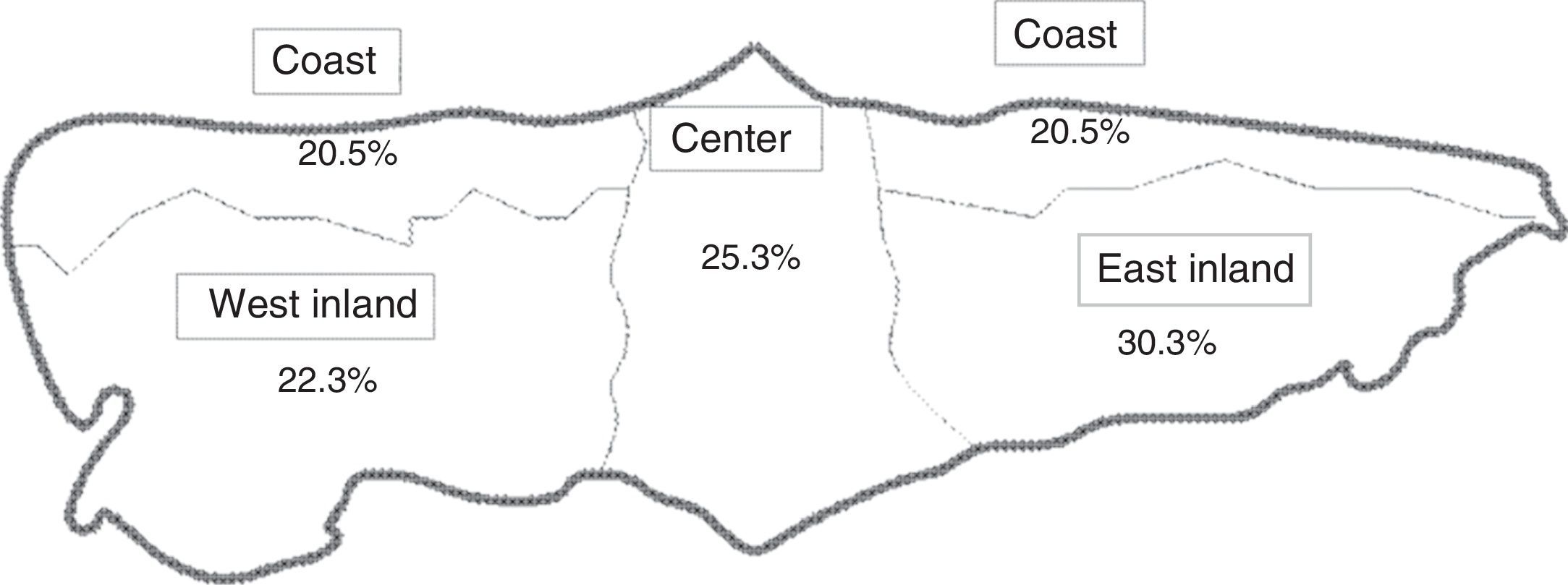
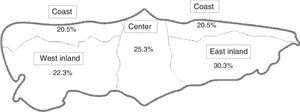
A descriptive observational study was made of the Asturian school population corresponding to the school year 2009–2010. The study was approved by the Ethics Committee of Hospital Universitario Central de Asturias. The region of Asturias was divided into four geographical zones (west inland, east inland, coast and center) for purposes of comparison.
The total study population consisted of 74,837 schoolchildren between 5 and 14 years of age, distributed among 232 schools. The analytical unit was the school, and within the latter we included all the children enrolled in first to sixth grade elementary school, and in the first and second year of secondary schooling (ESO), thereby covering all the schooling stages.
Cluster sampling was performed, the sample being initially stratified according to the above-mentioned four geographical zones, and 30 schools were then randomly selected (27 state and 3 private schools), distributed within these zones.
In order to determine mean ioduria in that population with a confidence level of 95% and a precision of ±10μg/L, the sample size calculation formula indicated the need to include 382 schoolchildren (formula applied to a finite population).
The total number of children initially selected by this sampling approach (i.e., before study losses) was 932 schoolchildren. The final number of children studied was 705 (0.94% of the total school population of Asturias and 75.4% of the initially selected sample), allowing us to minimize imprecision in the statistical calculations. Fig. 1 shows the map with the geographical distribution and the proportion of schoolchildren per zone.
Following sample selection, the schools received the list of selected children, the parent permission request forms, and a brief questionnaire to be completed by the families, addressing sociodemographic data (place of origin, educational level and profession of both parents), daily milk and yoghurt consumption on the part of the child, and the weekly consumption of cheese, fish, vegetables and eggs. The questionnaire also explored the regular use of iodized salt in the home. The use of iodized salt in school dining rooms was also evaluated.
The field work in turn comprised the following:
- •
The measurement of body height and weight (with a measuring rod and scale, respectively).
- •
Laboratory tests: a urine sample was collected for the measurement of ioduria from all the schoolchildren. The samples were stored frozen in sealed plastic containers until processing by means of HPLC-ECD (High Performance Liquid Chromatography with Electrochemical Detection). An Agilent 1200 chromatograph with a BioRad 1640 electrochemical detector and Waters Resolve C18, 3.9×150mm column was used. Assaying was performed by the Department of Clinical Biochemistry of Hospital Universitario Central de Asturias. The intra-assay precision was 4.8%, with a systematic error of −4.49%, while the inter-assay precision was 5.45%, with a systematic error of −3.73%. Comparisons were made versus the Benotti and Benotti method, with a good correlation being obtained, which showed the results of the two techniques to be comparable.12
Sample collection took place between December 2009 and May 2010 in the schools.
The SPSS version 15.0 statistical package was used for data processing. The values were reported as the mean±standard deviation (SD), or as the median and interquartile range (IQR) in the event of a non-normal distribution. The Mann–Whitney U-test and Kolmogorov–Smirnov test were used for comparison purposes. Correlations were established based on the Pearson or Spearman correlation coefficient, according to the study variables involved.
Statistical significance was considered for p<0.05 in all cases.
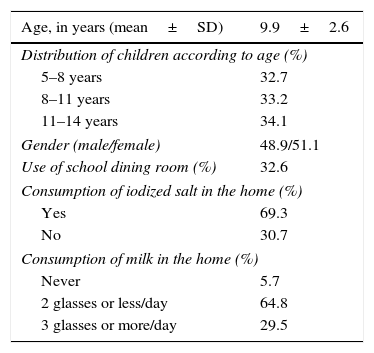
ResultsA total of 705 schoolchildren were studied (51.1% girls), with a mean age of 9.9 years (SD 2.6) (range 5–14 years). Table 1 shows the main demographic characteristics and data regarding milk and iodized salt intake.
Demographic characteristics and data regarding milk and iodized salt intake in the studied school population.
| Age, in years (mean±SD) | 9.9±2.6 |
|---|---|
| Distribution of children according to age (%) | |
| 5–8 years | 32.7 |
| 8–11 years | 33.2 |
| 11–14 years | 34.1 |
| Gender (male/female) | 48.9/51.1 |
| Use of school dining room (%) | 32.6 |
| Consumption of iodized salt in the home (%) | |
| Yes | 69.3 |
| No | 30.7 |
| Consumption of milk in the home (%) | |
| Never | 5.7 |
| 2 glasses or less/day | 64.8 |
| 3 glasses or more/day | 29.5 |
Mean ioduria was 202.5μg/L (SD 114), with a median of 180.7μg/L (P25–P75: 124–252.3μg/L; IQR 128.3μg/L), in a sample of 620 valid determinations (family permission for collecting the urine sample was not obtained in 85 children). There were no significant differences in urine iodine levels between genders (median ioduria 184.9μg/L in boys and 175.8μg/L in girls; p=0.26).
Likewise, no statistically significant differences were observed in median ioduria among the four geographical zones: center 182.7μg/L; coast 176.1μg/L; west 183.2 and east 183.3μg/L (p=0.46).
All the school dining rooms were seen to offer iodized salt, and 69.3% of the homes (95% confidence interval [95%CI] 65.3–72.1) consumed iodized salt regularly and homogeneously throughout Asturias: center 69.1%, coast 68.4%, west 74.7% and east 66.4% (p=0.40).
Ioduria among the schoolchildren using the school dining room was significantly higher than in those who did not (median 194.1 and 176.8μg/L, respectively; p=0.031).
Likewise, the children that regularly consumed iodized salt at home had significantly higher ioduria values (median 194μg/L) than those who did not (median 154μg/L; p<0.0005).
The proportion of children with low ioduria values (<50μg/L) was 2.5% (95%CI: 1.04–3.15%), while the proportion with very low ioduria values (<20μg/L) was only 0.2% (a single case from western Asturias).
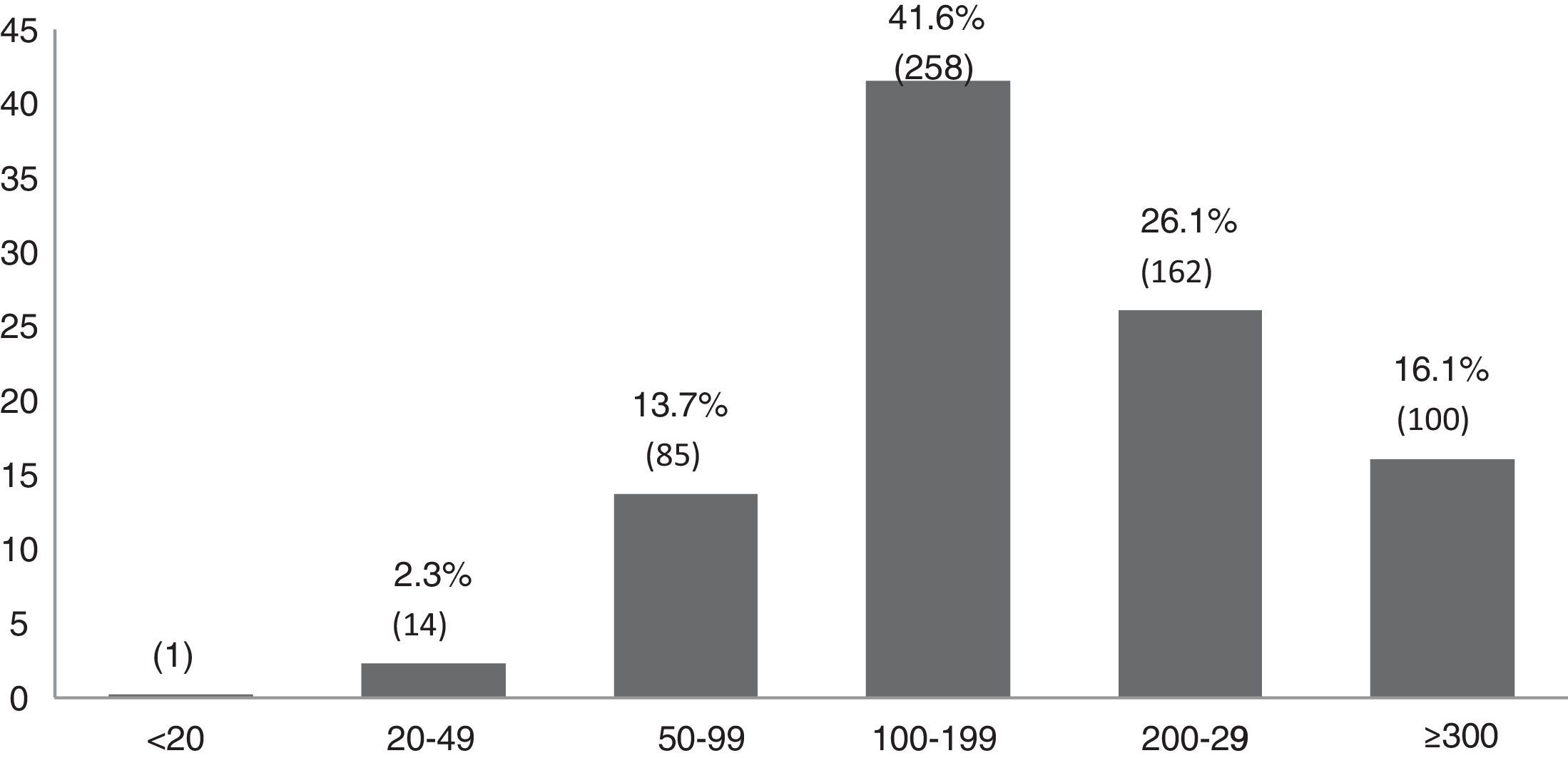
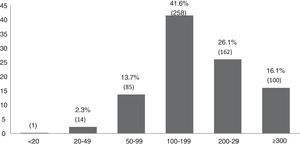
A total of 16.1% (95%CI: 13.2–19%) had ioduria values of under 100μg/L. In the west inland zone the percentage of children with ioduria values under 100μg/L was higher than on the coast (22% versus 11.2%; p<0.0001). The center and east zones showed a similar proportion of children with ioduria values under 100μg/L (17 versus 17.2%). Fig. 2 shows the distribution of ioduria into the different epidemiological intervals recommended by the WHO.10
Graphic representation of the distribution of ioduria among the schoolchildren of Asturias into the different epidemiological intervals recommended by the WHO.10
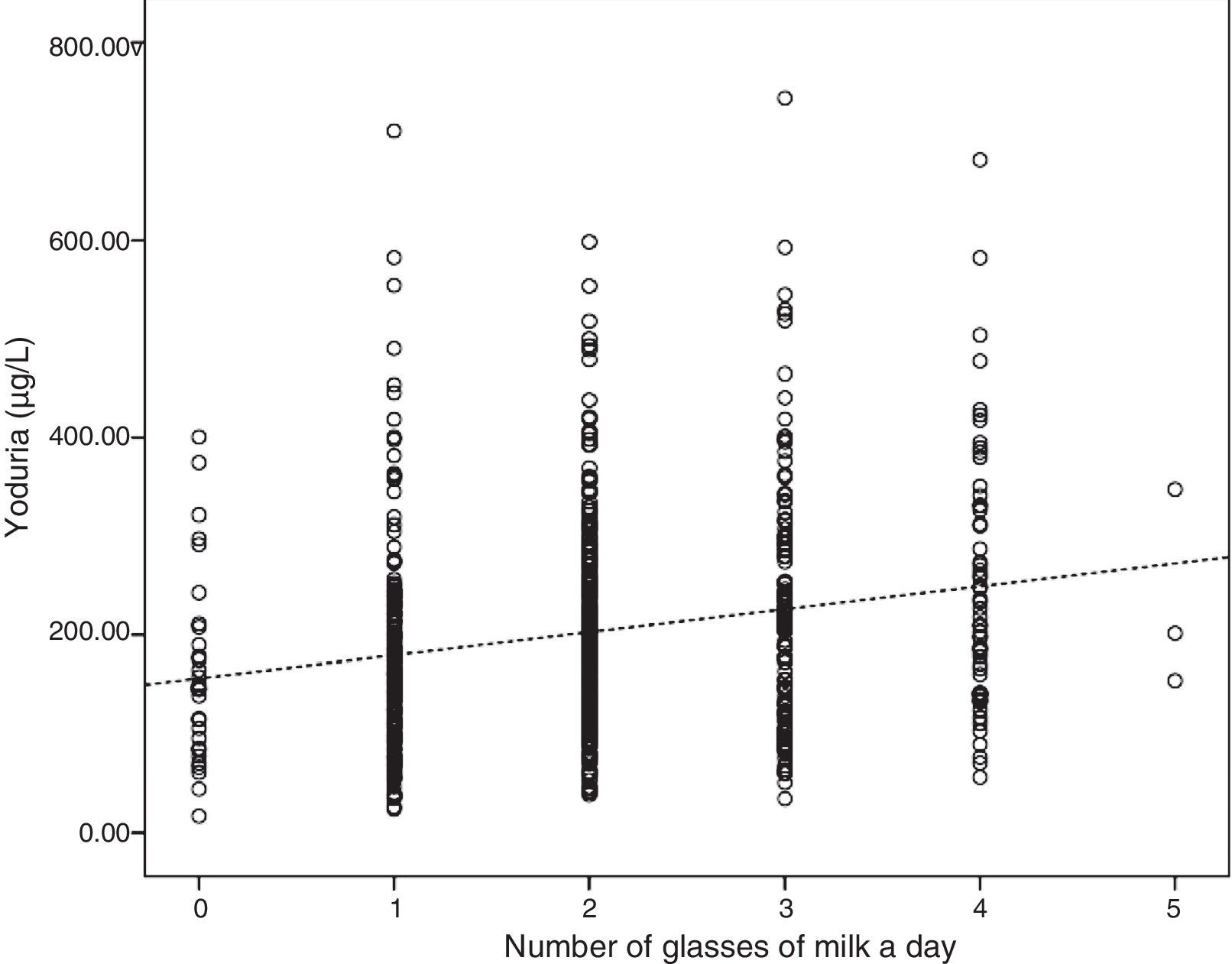
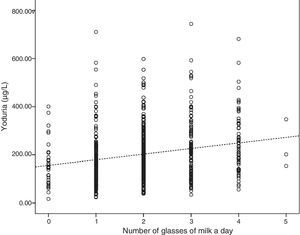
Milk consumption was significantly correlated to ioduria, the latter increasing proportionately with the number of daily glasses of milk consumed (p<0.0001; Fig. 3). Specifically, ioduria was seen to increase 24μg/L with each daily glass of milk. These differences were not observed in the case of the weekly servings of other foods such as fish, eggs or vegetables.
Differences in ioduria were also observed according to the time of year of urine sampling, with significantly lower values in the winter months (median 173μg/L; IQR 128.25) than in spring (median 198μg/L; IQR 138.27; p=0.006).
There were no differences in the iodine nutritional status of the schoolchildren in relation to the educational level or country of origin of the parents.
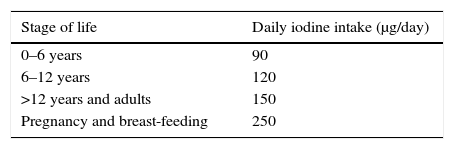
DiscussionAfter extreme starvation, dietetic iodine deficiency is the most frequent cause of avoidable mental retardation. In areas characterized by severe iodine deficiency it is possible to find maternal and fetal hypothyroxinemia secondary to such deficiency, resulting in damaged fetal neurological development.13 In developed countries, universal salt iodization is usually the most effective method for correcting IDDs.10 The recommended daily iodine intakes are well established (Table 2).14
Daily iodine intake recommendations by age groups (WHO).10
| Stage of life | Daily iodine intake (μg/day) |
|---|---|
| 0–6 years | 90 |
| 6–12 years | 120 |
| >12 years and adults | 150 |
| Pregnancy and breast-feeding | 250 |
In recent years the Spanish health authorities have adopted legislative and educational measures to increase iodine intake in our population15 (e.g., the mandatory use of iodized salt in school dining rooms in Galicia, Asturias and Andalucía). However, as the WHO emphasizes, it is not enough to legislate and introduce measures to ensure adequate iodine intake: further action is needed to periodically assess the impact of such interventions.
Asturias is the Spanish Autonomous Community which has carried out the largest number of studies within the IDD eradication program. In the first study in 1982,16 a clear iodine deficiency was found, with a mean ioduria in schoolchildren of 63.5μg/L. Subsequently, in 1983, the Spanish Royal Decree 1424/1983 of 27 April approved the technical-sanitary regulations for the obtaining, circulation and sale of edible salt and brines, with the definition of iodized salt. This was followed by an information campaign on the use of iodized salt, targeted both to health professionals and to the general population and, endorsed by the health authorities of Asturias. Since then, four further studies have been carried out (including the present study) to evaluate and strengthen these campaigns.
Based on the ioduria values recorded in our study (median 180.7μg/L), it can be affirmed that nutritional iodine status is sufficient in Asturias (median ioduria >100μg/L and <50μg/L in less than 20% of the cases), with only 16.1% of the schoolchildren presenting ioduria values of <100μg/L. This iodine status has been maintained since 1992. In this regard, ioduria values of <100μg/L were recorded in 84.8% of the schoolchildren in 1982 compared to only 16.1% at the present time, thereby confirming the efficacy of these campaigns.
In relation to the consumption of iodized salt in Asturian homes, the levels were seen to be lower than those currently recommended (69.3% of the homes consumed iodized salt regularly). This figure clearly falls short of the recommended target of 90% and is slightly lower than the value documented by the last study in Asturias in the year 2000,17 when 75% of homes were found to consume iodized salt.
Nevertheless, compared with other parts of the country, consumption in Asturias is noticeably greater than that revealed in other studies, which have reported iodized salt consumption rates of under 60% in Madrid18 and the Basque Country.19 With regard to the studies conducted at a nationwide level, the findings are quite consistent with those of the Tirokid study,20 with consumption in 69.8% of the homes. In the Di@bet.es study,21 iodized salt intake was significantly lower (43.9%), though the study population in this case was limited to adults only. It is therefore essential to conduct periodic health campaigns to promote iodized salt consumption among the global population.
In many industrialized countries the main dietetic sources of iodine are iodized salt and certain foods enriched with iodine during production and processing – particularly milk, due to the use of iodized feed and iodine disinfectants for the udders of the cows.19 On the other hand, salt iodization is the best and cheapest strategy for eradicating and preventing IDDs. The WHO and ICCIDD recommend as a target the regular consumption of iodized salt in 90% of homes.22
Despite the low implementation of iodized salt intake, the iodine nutritional status among the schoolchildren in Asturias remains adequate: appropriate ioduria levels are found even in children that do not consume iodized salt at home (median 154μg/L). There consequently may be other sources of iodine apart from iodized salt in the home. Iodized salt consumption in school dining rooms, documented in 32.6% of the children, constitutes another possible source of iodine apart from iodized salt in the home, and could contribute to the adequate iodine nutritional status in the studied population.
Because of the frequency with which they are consumed, milk and dairy products have become vehicles for the supply of a considerable amount of dietetic iodine in different countries. A study carried out in Spain with different brands of cow's milk recorded iodine concentrations of between 200–270μg/L of milk.23 Iodine prophylactic measures in livestock have been in use in Europe for 80 years.24 In Spain, studies among schoolchildren in the area of Axarquía,25 the Basque Country19 and, more recently, at a nationwide level in the Tirokid study20 have demonstrated a relationship between dairy product consumption and iodine nutritional status. The consumption of dairy products has also been directly related to ioduria. It may have made an uncontrolled contribution to the observed iodine nutrition level, and is confirmed as another important source of this micronutrient. This relationship has also been demonstrated in pregnant women.26
Mention should be made of the observed seasonal differences in ioduria. In effect, the results showed that median ioduria was not constant throughout the year: lower values were recorded from December to February (173μg/L) compared with the spring months from March to May (198μg/L). Seasonal differences have also been found in other studies, though with a different trend, since most studies, such as that conducted in the Basque Country,19 have reported higher ioduria values during the winter months. This variation in principle can be attributed to the increased use of iodized animal feed in the winter months, due to lesser access to pastures. A review of the scientific literature revealed no large population-based studies with data on seasonal variations, possibly because most studies involve only a short period of time, thereby precluding the observation of variations in ioduria during the course of the year.
One of the limitations of our study is the fact that the consumption of both iodized salt and dairy products was determined on the basis of the questionnaire completed by the parents of the schoolchildren, with no “on site” verification as in the study published by Arrizabalaga et al.19
In conclusion, the iodine status of the schoolchildren in Asturias is currently sufficient, though the consumption of iodized salt in the home is still far from the established 90% target rate. In any case, there are other dietetic iodine sources, such as milk, which have contributed to maintain this nutritional status. The development of health education initiatives and public health campaigns favoring the consumption of iodized salt in the home, and particularly the periodic evaluation of such campaigns, remain necessary in order to fully eradicate IDDs.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Riestra Fernández M, Menéndez Torre E, Díaz Cadórniga F, Fernández Fernández JC, Delgado Álvarez E. Estado nutricional de yodo en la población escolar asturiana. Endocrinol Diabetes Nutr. 2017;64:491–497.