Pituitary abscess (PA) is a rare pituitary lesion. Diagnosis suspicion could arise in the presence of hypopituitarism, a suggestive pituitary MRI image or a recent history of meningitis, sinusitis or cranial surgery. We present the case of a patient with PA who progressed favourably with medical treatment.
A 55-year-old man, smoker, consumer of alcohol and inhaled cocaine, with a history of meningitis in childhood and recurrent renal colic for which the patient customarily drank 4–5 l of water a day. He presented with a two-month history of forehead headache and was diagnosed by CT with acute maxillary, ethmoid and sphenoid sinusitis. He received antibiotic therapy but his condition worsened, and he was referred to the emergency department due to acutely reduced level of consciousness, headache and fever. Meningoencephalitis with cerebral oedema and incipient signs of uncal herniation were diagnosed by CSF and cranial CT. He was admitted to the Intensive Care Unit for 7 days, receiving antibiotic therapy, external ventricular shunt and dexamethasone 4 mg/8 h (5 days) with good initial response, but persistence of fever. Three days after discharge from the ICU and four or five days after stopping the corticosteroid treatment, he presented with hypotension, nausea and vomiting. The most relevant laboratory test findings were ACTH 19.9 pg/mL (4.7–48 pg/ml), cortisol 5.37 mcg/dl (6–19.4 mg/dl), TSH 0.52 mU/l (0.4−4 mU/l), T3 1.18 pg/mL (1.8–4.6 pg/ml), T4 0.5 png/dl (0.7–1.8 ng/dl), LH < 0.1 mIU/mL (1.7–8.6 mIU/mL), FSH 1.19 mIU/mL (1.5–12.4 mIU/mL), testosterone 0.03 mcg/l (2.8−8 mcg/l).
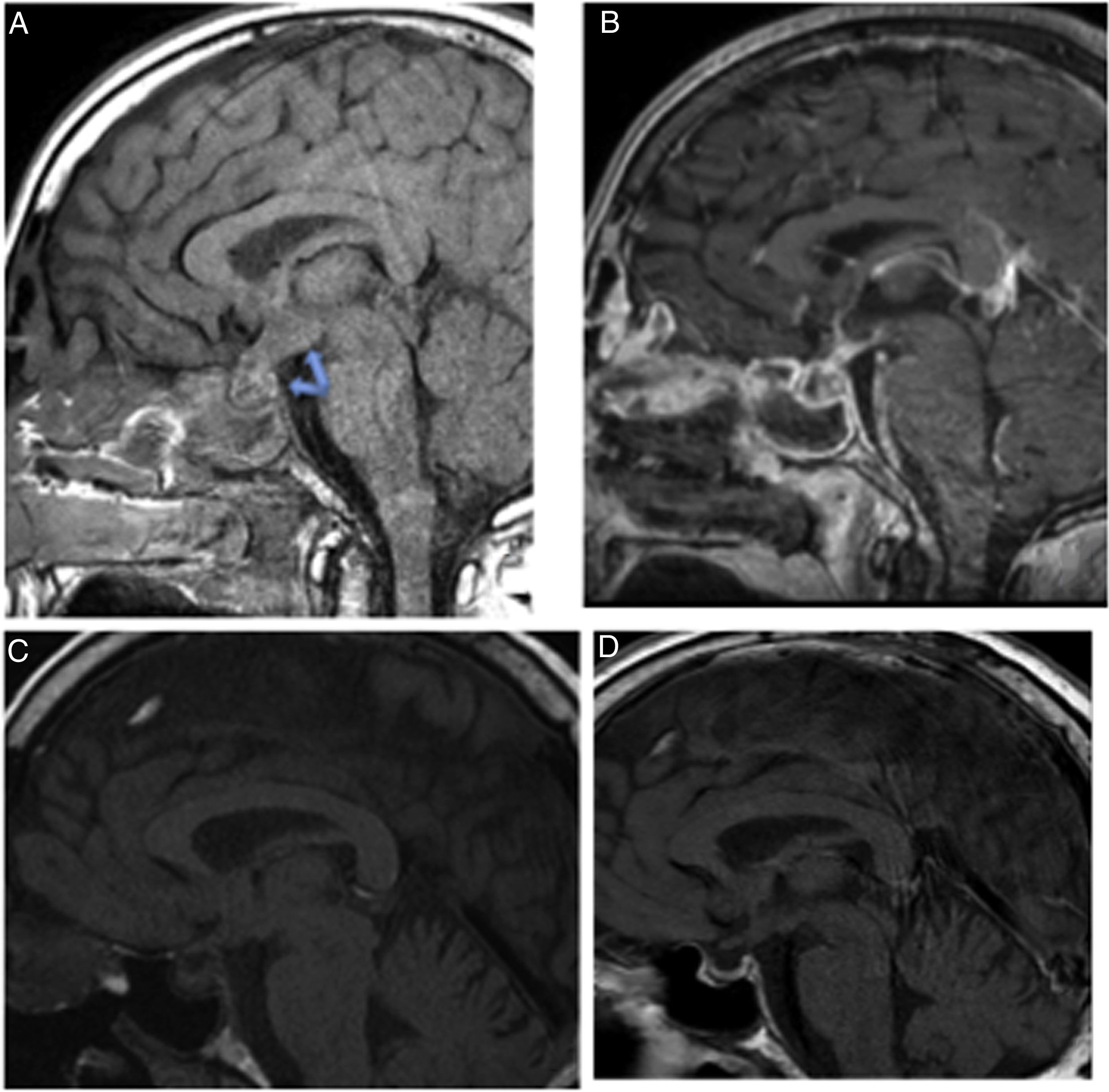
MRI revealed a cystic collection in the hypothalamus with restricted diffusion of 12 × 9 × 11 mm connected to another image in the pituitary of 14 × 12 × 8 mm, findings consistent with hypothalamic-pituitary abscess (Fig. 1. A and B).
Pituitary MRI images.
A: Sagittal T1 without contrast revealing hypothalamic-pituitary occupation with infundibular (pituitary stalk) thickening, which with the introduction of contrast (B) reveals peripheral enhancement and cystic content. C: Follow-up MRI one month after diagnosis: disappearance of the hypothalamic abscess. Persistence of an infiltrative lesion in the pituitary gland and in the pituitary stalk. D: Follow-up MRI at 6 months. Resolution of the hypothalamic-pituitary abscess.
Panhypopituitarism secondary to pituitary infundibulum (stalk) abscess was diagnosed. After introducing replacement therapy with corticosteroids and levothyroxine, and coinciding with the free intake of water to which the patient was accustomed, he manifested polyuria of up to 11 l. A water deprivation test was performed that was consistent with central diabetes insipidus (DI) (baseline urine osmolarity 103 mOsm/kg [300–1000 mOsm/kg], after water deprivation 272 mOsm/kg and post-administration of desmopressin 402 mOsm/kg) and treatment with desmopressin was initiated.
CSF and blood cultures were negative; Staphylococcus epidermidis, Streptococcus parasanguinis and Streptococcus constellatus grew in the pus culture from the paranasal sinuses. Antibiotic therapy was adjusted and maintained for six weeks.
The patient continued follow-up in endocrinology; six months after the onset of the condition, the ACTH and ADH deficiency had recovered. The hypothalamic abscess had resolved in the first month MRI, and the pituitary abscess by the sixth month (Fig. 1C and D).
PAs are rare sellar lesions (<1% of all pituitary lesions) but are associated with high mortality.1–3
They can be classified according to their aetiology as primary PA (70%)—occurring in a previously healthy gland—and secondary (30%), which arise from pre-existing lesions, the most common of which being pituitary adenoma, followed by Rathke's cleft cyst, craniopharyngioma and lymphoma.1,3–5
PAs can be caused by haematogenous spread or by direct spread of an adjacent infection (sinusitis, meningitis, contaminated CSF fissure or cavernous sinus thrombophlebitis).1,5–7
In our case, it is striking that the source of infection was acute maxillary, ethmoid and sphenoid sinusitis that spread to the central nervous system. The history of inhaled cocaine use is significant, since it has been reported that it causes bone lesions (for example, the base of the skull) that facilitate communication of the sinonasal cavity with the central nervous system and the pituitary. However, the CT/MRI ruled out visible lesions.8
The most commonly isolated pathogens are Staphylococcus spp. and Streptococcus spp., followed by Neisseria spp., Micrococcus, Citrobacter spp., Escherichia coli, Brucella, Salmonella, Corynebacterium and Mycobacterium. In immunocompromised patients the most common are Aspergillus, Candida and Histoplasma.4,9
Initial empirical antibiotic therapy with ceftriaxone is proposed pending microbiological confirmation. The duration of antibiotic therapy is 4–6 weeks.1,4,5
In our case, empirical treatment with ceftriaxone and vancomycin was started, which was later modified to linezolid for 6 weeks.
Acute PAs (as in our case) are rare, presenting with acute and severe infectious symptoms.
Subacute PAs (less than one month) present mild infectious manifestations such as fever and/or leukocytosis, with DI being common. Chronic PAs (more than one month) present polyuria, headache and/or other symptoms of endocrine dysfunction, without infectious symptoms, and can be confused with a pituitary tumour. DI is the most common symptom (40%) and useful for differential diagnosis, because it is rarely a presenting feature of pituitary adenomas.1
The most common symptoms are headache, visual disturbances and anterior pituitary dysfunction due to the destruction and necrosis manifested as asthenia, anorexia, vomiting, amenorrhoea and hypogonadism.5 Panhypopituitarism is the most common manifestation of hypopituitarism (83% according to the series by Lu et al.), followed by isolated hypogonadotropism (9.3%), isolated ACTH deficiency (3.7%), isolated hypothyroidism (1.8 %) and hypogonadism combined with ACTH deficiency (1.8%). This severe pituitary hypofunction is an important feature in the differential diagnosis, since it is rare in pituitary adenomas, and when it occurs it produces mild symptoms, except in acute pituitary apoplexy.1,3
Typical features of the abscess on MRI include a totally or partially cystic mass in the sellar region, hypointense or isointense on T1, and hyperintense or isointense on T2, revealing peripheral ring enhancement after gadolinium injection (Fig. 1 B).5 In our case, it is notable that this pituitary lesion continues to the hypothalamus. However, this pituitary finding is not specific, since it is observed in Rathke's cleft cyst, in cystic craniopharyngiomas and in cystic adenomas; these characteristics are useful if there are compatible signs and symptoms. In pituitary apoplexy, bleeding on imaging evolves as follows: in the acute phase it is hypointense on T2, in the subacute phase it is hyperintense on T1 and hypo/hyperintense on T2, and in the chronic phase it is hypointense on T1 and T2.1,3,4,7
Transsphenoidal surgery is the treatment of choice if PA is suspected, followed by antibiotics, although some acute-subacute cases can be treated with antibiotics alone. Craniotomy will be performed if the abscess is suprasellar or if complete evacuation is problematic. Surgical complications include meningitis, vascular injury and CSF leakage, which are less and less common.1,4–6,10
In the series published by Weng-sheng, 66.7% of patients recovered ACTH function, 50% TSH and 62% gonadotropin. In our case, the ACTH and ADH deficiencies recovered, but the TSH and gonadotropin deficiencies persist.2
Men, acute onset and normal prolactin levels are predisposed to greater clinical recovery than women, chronic and hyperprolactinaemia, respectively. PA recurrence tends to be rare.5
Surgery does not significantly affect the rate of recovery from anterior pituitary disorders and DI, and could even increase or delay the risk. Additionally, if symptoms abate before surgery or if the MRI shows a substantial reduction in the abscess, surgery may not be necessary.2,6
Patients with acute infectious systemic symptoms (such as our case) are good candidates for antibiotic therapy without surgery.2
Death from PA is due to severe hypopituitarism and not the abscess itself, so hormonal support is the priority treatment to prevent life-threatening crises. However, surgery helps to quickly resolve the lesions and supports endocrine recovery if the abscess persists.2
PA is a rare lesion that is difficult to manage. However, medical treatment can be a successful therapeutic option in acute and subacute cases.
Please cite this article as: Reyes Céspedes LM, Barahona San Millán R, Gómez Roselló E, Chara Cervantes J, Recasens Sala M. Absceso hipotálamo hipofisario como complicación de sinusitis aguda: caso clínico y evolución con tratamiento conservador. Endocrinol Diabetes Nutr. 2021;68:441–443.