To provide practical recommendations for the comprehensive approach of people with type 2 diabetes according to evidence-based medicine.
ParticipantsMembers of the Diabetes Knowledge Area of the Spanish Society of Endocrinology and Nutrition.
MethodsThe recommendations were formulated according to the degrees of evidence of the Standards of Medical Care in Diabetes—2022. After reviewing the available evidence and formulating recommendations by the authors of each section, several rounds of comments were developed incorporating the contributions and voting on controversial points. Finally, the final document was sent to the rest of the members of the area for review and incorporation of contributions, to finally carry out the same process with the members of the Spanish Society of Endocrinology and Nutrition Board of Directors.
ConclusionsThe document establishes practical recommendations based on the latest available evidence for the management of people with type 2 diabetes.
Proporcionar recomendaciones prácticas para el abordaje integral de las personas con diabetes tipo 2 según la medicina basada en la evidencia.
ParticipantesMiembros del Área de Conocimiento de Diabetes de la Sociedad Española de Endocrinología y Nutrición.
MétodosLas recomendaciones se formularon según los grados de evidencia de los Standards of Medical Care in Diabetes—2022. Tras la revisión de la evidencia disponible y la formulación de recomendaciones por los autores de cada apartado, se desarrollaron varias rondas de comentarios con incorporación de las aportaciones y votación de los puntos controvertidos. Por último, el documento final se remitió al resto de los miembros del área para revisión e incorporación de aportaciones, para, finalmente, realizar el mismo proceso con los miembros de la Junta Directiva de la Sociedad Española de Endocrinología y Nutrición.
ConclusionesEl documento establece unas recomendaciones prácticas basadas en la última evidencia disponible para el manejo de las personas con diabetes tipo 2.
In 2018, the Diabetes Working Group of the Sociedad Española de Endocrinología y Nutrición [Spanish Society of Endocrinology and Nutrition] (SEEN) drafted a document on a comprehensive approach to type 2 diabetes (DM2), which compiled the evidence available at the time. Although some specific updates were made to the document based on the publication of new studies, the SEEN Diabetes Knowledge Area suggested that there were substantial changes, not only in terms of new evidence on anti-diabetic therapies, but also in terms of the comprehensive approach to people with DM2. Therefore, a comprehensive update of the document was proposed.
MethodThe recommendations were formulated according to the degrees of evidence of the Standards of Medical Care in Diabetes—2022.1 Following the review of the available evidence and the formulation of recommendations by the authors of each section, there were several rounds of comments, incorporating the contributions and voting on controversial points. The final document was sent to the other members of the area for review and incorporation of the contributions made, and then the same process was carried out with the members of the SEEN Board of Directors.
The following is a summary of the main changes in the document: Comprehensive Approach to People with Type 2 Diabetes, 2022, available at: https://www.seen.es/portal/documentos/texto-completo-abordaje-integral-dm2-2022.
Guide to recommendationsThis section covers the main points of comprehensive management of people with DM2 in terms of treatment selection and the detection of complications associated with diabetes, in an attempt to advance the concept of personalised medicine.
–Consider the initial combination therapy of choice, depending on comorbidities and glycaemic control.
–Early intensification of treatment (and reassessment every 3–6 months) until therapeutic goals are achieved.
–Individualise glycaemic control targets dynamically throughout the course of diabetes.
–Use of therapies with proven cardiorenal benefit, regardless of the degree of glycaemic control, assessing whether adjustments of other therapies are necessary.
–Intensive treatment of cardiovascular risk factors (dyslipidaemia, hypertension, smoking) together with the prevention and treatment of overweight/obesity.
–Perform systematic screening for micro- and macrovascular complications and other comorbidities associated with DM2, such as metabolic liver disease.
–The presence of high or very high cardiovascular risk, established cardiovascular disease (CVD)/heart failure (HF) or diabetic kidney disease should be determining factors for the selection of pharmacological treatment.
–Prevention and treatment of overweight and obesity should be one of the key determining factors of treatment.
–Prescribe diet and physical exercise at any time during the course of diabetes, adapting according to comorbidities. Ensure personalised therapeutic education as a pillar of comprehensive care for people with diabetes.
–Prioritise patient-centred conversation: anticipatory guidance. Inform the person with diabetes of the benefits of the therapies, as well as possible adverse events, in order to improve adherence.
–Consider de-intensifying treatment if frailty is present, maintaining drugs with cardiorenal benefit on a case-by-case basis.
The overall glycaemic control target, HbA1c <7%, should be adapted during the course of diabetes, individualising and avoiding episodes of hypoglycaemia. A more stringent HbA1c target of <6.5% can be achieved in people without frailty and on antidiabetic therapies without risk of hypoglycaemia. In contrast, in the presence of frailty and other comorbidities, in case of high hypoglycaemic risk or the presence of inadvertent hypoglycaemia, a less stringent glycaemic control target may be appropriate (HbA1c 8%–8.5%).
In addition, control targets are included depending on the continuous monitoring record or flash glucose, adapted according to each clinical situation.2
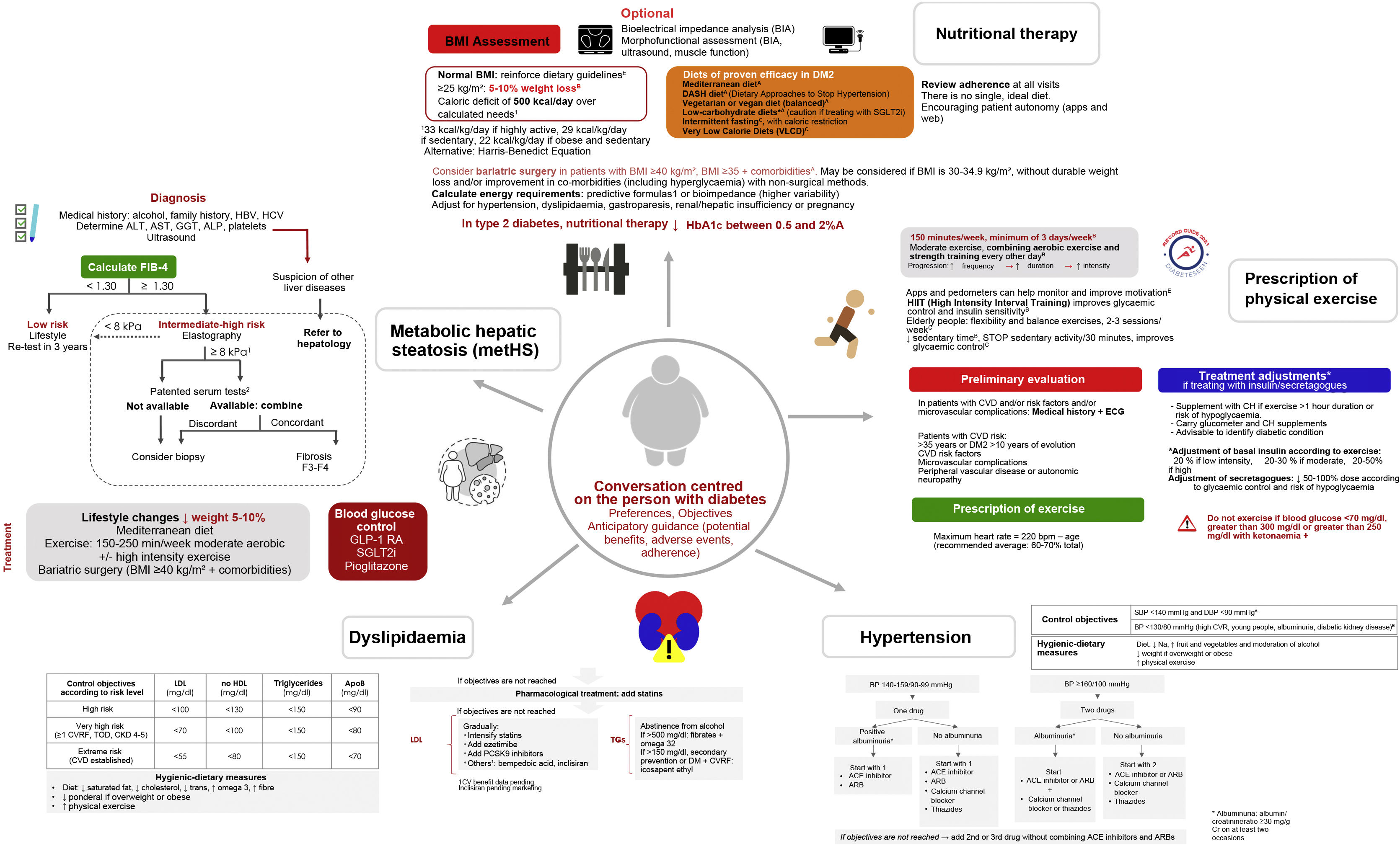
Prescription of physical exerciseThe prescription of physical exercise is a highly relevant aspect in people with DM2. Physical exercise should be prescribed and monitored at each visit. The minimum recommendation is 150min/week, distributed over at least three days a week, and combining aerobic and strength exercise, subsequently increasing the frequency, duration and intensity of the exercise, according to the sequence, frequency, duration and intensity (Fig. 1).
Comprehensive approach to people with type 2 diabetes mellitus (DM2): nutritional therapy, physical activity, hypertension, dyslipidaemia and metabolic hepatic steatosis.
ELF: Enhanced Liver Fibrosis; N/E: not evaluated.
1If the result is compatible with F3–F4, consider serum tests for metabolic hepatic steatosis.
2Cut-off points: ELF™ 9.8 (NAFLD/ALD); FibroMeter 0.45 (NAFLD), Fibrotest 0.48 (NAFLD).
Prior assessment is recommended in patients with CVD, risk factors and/or microvascular complications. In addition to prescribing exercise, it is necessary to assess whether treatment adjustments (insulin and secretagogues) are necessary, ensuring sufficient knowledge for the detection and treatment of hypoglycaemia. In addition, if there are chronic micro- or macrovascular complications, some exercises are advisable and others should be avoided.
To supplement this information, reference is made to the RECORD3 Guide: clinical recommendations for the practice of sport in people with diabetes mellitus, produced by the diabetes area and available on the SEEN website.
Nutritional therapyThe first step should be to assess the body mass index. Other optional techniques are bioimpedance body composition assessment and morphofunctional assessment with bioimpedance, muscle ultrasound and muscle function testing. In addition to the Mediterranean diet, there are other dietary approaches that have shown benefit in DM2, such as low-carbohydrate diets and vegetarian or vegan diets4 (Fig. 1).
It also includes updated recommendations for the different food groups, indicating which ones are advisable and which ones should be avoided or limited.4
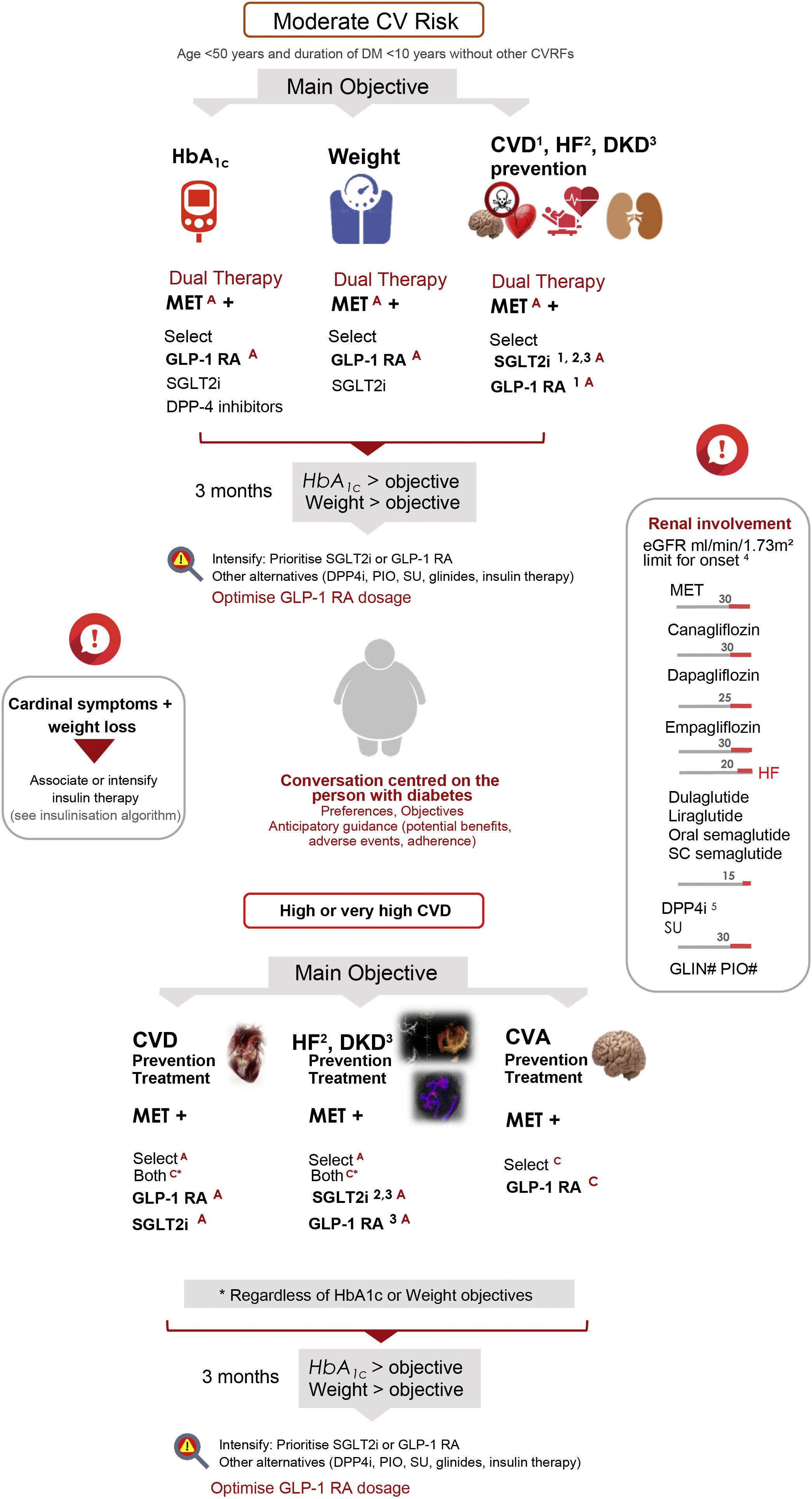
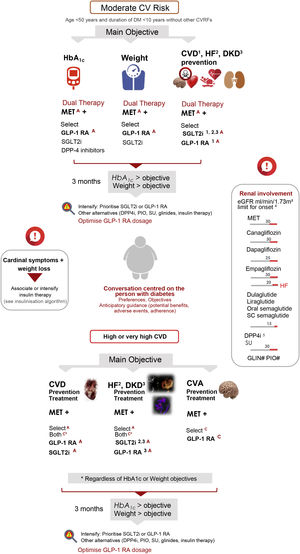
Selection of drugs in type 2 diabetes mellitusTwo situations are identified: moderate cardiovascular risk (age <50 years and diabetes duration <10 years, without other cardiovascular risk factors [CVRF]) and high or very high CV risk, depending on the presence of CV and/or renal involvement5 (Fig. 2).
Drug selection in type 2 diabetes mellitus. Initial treatment or with previous therapy (OAD, GLP-1 RA, insulin).
Drugs indicated in order of priority. GLP-1 RA in Spain funding limited to BMI≥30kg/m2. Avoid sudden drops in HbA1c in patients with advanced retinopathy.
CVD: cardiovascular disease; CVRF: cardiovascular risk factors; DKD: diabetic kidney disease; DM: diabetes mellitus; GLP-1 RA: GLP1 receptor agonists; HF: heart failure; MET: metformin; OAD: oral antidiabetics; PIO: pioglitazone; SGLT2i: sodium-glucose cotransporter 2 inhibitors; SU: sulfonylureas.
Benefit demonstrated in 1CVD, 2HF, 3DKD, with the indicated therapeutic groups.
4If eGFR <60, CANA 100mg, EMPA 10mg, maintain SGLT2i and GLP-1 RA until haemodialysis.
5Dose adjustment in CKD except for linagliptin.
# No dose adjustment required; in advanced CKD, monitor repaglinide dose (hypoglycaemia).
In both situations, it is advisable to select treatment that includes metformin in combination with other anti-diabetic therapies that have demonstrated benefit in CVD, HF or diabetic kidney disease (GLP-1 receptor agonists [GLP-1 RA], SGLT2 inhibitors [SGLT2i]), while ensuring adequate glycaemic and weight control.6 Dual therapy is considered at baseline according to risk, intensifying early until targets are achieved.
The different therapies are prioritised according to the main treatment goal (glycaemic control, weight, prevention and treatment of CVD-HF-diabetic kidney disease) and the evidence demonstrated for each goal is specified.
As a novelty, the importance of a conversation centred on the person with diabetes is established, considering their preferences and setting agreed treatment goals. In addition, it is advisable to provide information on both the expected benefits of antidiabetic treatment and the potential adverse effects, in order to try to improve adherence.
In selecting antidiabetic therapies in DM2, it is recommended that metformin, GLP-1 RA and SGLT2i be prioritised. If using GLP-1 RA, the dose should be optimised to achieve the greatest clinical benefit.6
Renal function, measured by eGFR, determines the eligibility for different antidiabetic therapies and may condition a dose adjustment, as indicated in the document (Fig. 2).
Evidence on CVD, mortality and diabetic kidney disease from diabetes therapiesDifferent antidiabetic therapies have demonstrated benefits on major adverse CV events, CV and all-cause mortality, hospitalisation due to HF, stroke and major adverse renal events.6
The available evidence on the different targets is compiled in the 2022 version of the document, and it is recommended to use the therapies within each pharmacological group that have demonstrated CV or renal benefit (GLP-1 RA, SGLT2i), or that have at least completed a CV safety study with a neutral result (sitagliptin, linagliptin).
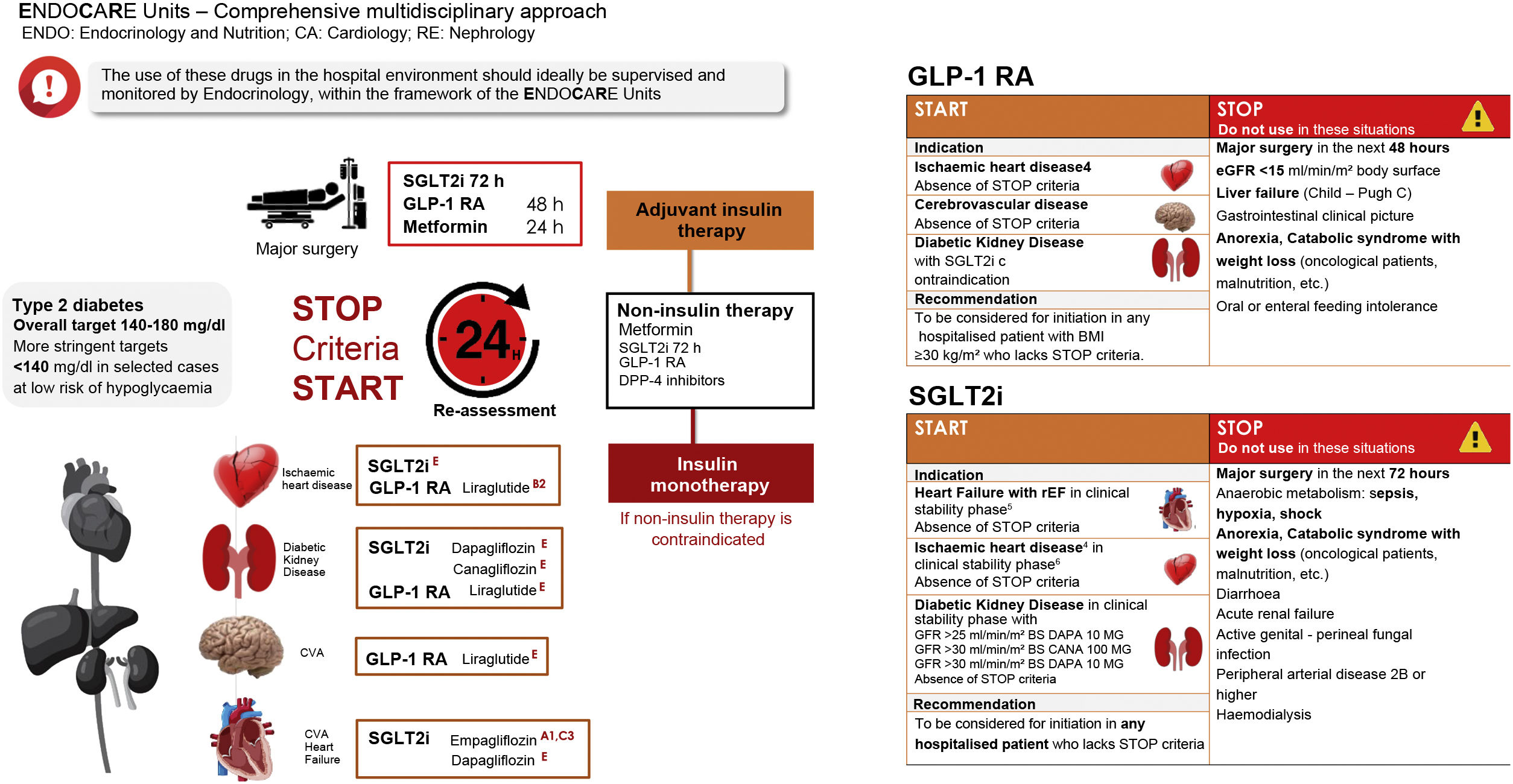
DM2 treatment in hospitalised patientsThis chapter is a new addition in the 2022 version of the document. In addition to insulin treatment during hospitalisation, there is the possibility of a comprehensive multidisciplinary approach in ENDOCARE units (ENDO: Endocrinology and Nutrition; CA: Cardiology; RE: Nephrology), using GLP-1 RA and SGLT2i not only on hospital discharge, but also as part of the management of the hospitalised DM2 patient.
Hospitalisation of a person with DM2 is an excellent opportunity to improve not only antidiabetic and CVRF treatment, but also to positively influence the subsequent evolution by associating disease-modifying therapies, to make a comprehensive assessment of the different comorbidities and, ideally, to improve treatment adherence. Multidisciplinary inpatient care would allow for optimisation of treatment, and at the same time, would ideally improve transition to discharge, coordination of the different specialists involved in the care of people with DM2 and variability in treatment.
Diabetes is present in approximately 30% of hospitalised patients, and almost all of these patients have very high cardiovascular risk or established atherosclerotic disease. The implementation of a clinical practice guideline for the comprehensive management of diabetes in the in-hospital setting, including therapies with benefits in cardiorenal morbidity and mortality (SGLT2i, GLP-1 RA) and their real-life validation, has become a priority for any centre of excellence, with the aim of improving the quality of care and optimising resources. ENDOCARE units emerge as multidisciplinary integrated elements (endocrinology, nephrology, cardiology and family and community medicine) and the aim is to create solid clinical management structures throughout the care process. Their main objectives include: developing an efficient care model with measurable objectives, expanding the application of evidence-based precision medicine and therapeutic education (specialised nursing), improving quality of life and reducing morbidity and mortality in people with DM2, the pursuit of excellence in care and continuity of care and, lastly, promoting multidisciplinary teaching and research activities.
A general target of 140–180mg/dl is set as a goal for glycaemic control in hospitalised patients. More stringent targets, such as <140mg/dl, may be considered in selected cases with low risk of hypoglycaemia.
The available evidence for each drug from in-hospital studies and the precautions to be taken into account before major surgery (discontinue 24h before if treated with metformin, 48h if treated with GLP-1 RA, 72h before if treated with SGLT2i) are included. Criteria for use, START and STOP criteria, are established to be assessed every 24h during treatment with non-insulin therapies in hospitalised patients and to ensure safe use of these therapies during hospitalisation (Fig. 3).
Treatment of type 2 diabetes mellitus in the hospitalised patient.
BS: body surface; DPP4i: dipeptidyl peptidase-4 inhibitors (sitagliptin, linagliptin); GLP-1 RA: GLP1 receptor antagonists (liraglutide, semaglutide sc/oral, dulaglutide); HF: heart failure; PAD: peripheral arterial disease; SGLT2i: sodium-glucose cotransporter 2 inhibitors; (empagliflozin, dapagliflozin, canagliflozin).
EvidenceA–E available applicable to:
1Composite target reduction: death, number of HF events, time to first HF event, changes in KCCQ-TSS after 90 days of treatment.
2Better metabolic control vs. insulin monotherapy.
3Fewer hypoglycaemias vs. insulin monotherapy.
4Individualise its indication against GLP-1 RA/SGLT2i as an alternative or evaluate combination.
5Absence of haemodynamic instability, uncontrolled PAD or cardiogenic shock.
6Absence of signs of acute ischaemia or haemodynamic instability.
At hospital discharge maintain-initiate SGLT2i/GLP-1 AR or both, according to evidence-based medicine (see “Selection of drugs in DM2”).
In people with DM2 on non-insulin therapy who do not achieve glycaemic control within target range, it is advisable to consider starting basal insulin. The document presents the evidence for each basal insulin, the starting dose and the individualised dose adjustment according to glycaemic values and the characteristics of the person with diabetes. If target glycaemic control is not achieved after initiation and adjustment of basal insulin, the addition of SGLT2i and/or GLP-1 RA and/or DPP4i is recommended, if not previously used, on a case-by-case basis.
If target glycaemic control is not achieved with previous therapies, the addition of rapid insulin will be considered according to the glycaemic values at different meals.
Management of cardiovascular risk factorsTreatment of dyslipidaemia and hypertension should be targeted according to the level of risk. Lifestyle measures are a fundamental part of treatment, in addition to drug therapy, which will be necessary from the outset depending on the treatment goal to be achieved.7
To reduce LDL-cholesterol concentrations, statins, ezetimibe and PCSK9 inhibitors are advised, using a scaled approach. The possibility of evaluating forthcoming new lipid-lowering therapies, such as bempedoic acid and inclisiran, which have yet to demonstrate their efficacy on cardiovascular morbidity and mortality, is included (Fig. 1).
Abstinence from alcohol is recommended for the treatment of hypertriglyceridaemia. If triglyceride concentrations are greater than 500mg/dl, treatment with fibrates and omega-3s is indicated, although high doses of omega-3s are needed and CV benefit has only been demonstrated with icosapent ethyl, which will be available soon. If triglyceride concentrations are >150mg/dl, secondary prevention or for diabetes+CVRF, icosapent ethyl is advised.
Safety profileInformation on the adverse effects of anti-diabetic therapies is compiled according to the latest information in the summaries of product characteristics. Precautions regarding the use of metformin and SGLT2i during hospitalisation and prior to scheduled surgery are included.
The importance of informing the person with diabetes of the potential adverse effects of GLP-1 RA and SGLT2i and measures to reduce these adverse effects is included, as a measure to promote treatment adherence and consistency.
Metabolic hepatic steatosisThe diagnostic approach to metabolic liver disease is based on the calculation of FIB-4 (pathological if value ≥1.3); depending on the estimated risk (intermediate-high), elastography is recommended. If the elastography value is ≥8kPa and the result is compatible with F3–F4, serum tests in combination with other patented serum tests, if available (ELF™, FibroMeter, Fibrotest) should be considered, as they will help to define the degree of fibrosis. If these tests are not available or the results are not consistent, a liver biopsy should be considered8 (Fig. 1).
In people with DM2 and metabolic hepatic steatosis, it is important to assess CV risk and the presence of renal involvement, given the coexistence of these conditions.
The main pillar of treatment is lifestyle change and following a Mediterranean diet to achieve a weight loss of 5%–10%. GLP-1 RA (semaglutide, liraglutide), SGLT2i and pioglitazone are recommended as anti-diabetic therapies. These three therapies have been shown to reduce steatosis, GLP-1 RA and pioglitazone reduce inflammation, and pioglitazone has been shown to reduce fibrosis, although the evidence is limited.
Given the association between metabolic hepatic steatosis, CVD and renal disease, strict blood pressure control (ARBs have preliminary data of hepatic benefit) and intensive lipid-lowering therapy are also advised.
Comprehensive approach in the elderly patientIn people with DM2 and advanced age, it is advisable to assess for frailty (FRAIL scale). In individuals with good functional status, the principles of treatment selection are the same as those recommended in the section on selection of antidiabetic treatment. An annual geriatric assessment using the Pfeiffer test and the Yesavage scale is recommended, and family support should be assessed at each visit. Avoidance of hypoglycaemic episodes should be a priority, as well as proper treatment of CVRFs (hypertension and dyslipidaemia) and systematic assessment of chronic complications.9
In elderly people with DM2 and frailty, the glycaemic control target may be less stringent and it is advisable to consider treatment withdrawal if HbA1c is below target, while maintaining therapies with CV and renal benefit on an individualised basis. Consideration will be given to treatment with weekly GLP-1 RA, ensuring adapted nutritional and physical activity therapy, and with iSGT2 and DPP4i because of the low risk of hypoglycaemia.
Diabetes and pregnancyGestational diabetes (GD) is diabetes that is diagnosed for the first time during pregnancy, although other types of diabetes (DM2, type 1 diabetes, MODY) may manifest for the first time during pregnancy. GD entails increased morbidity in the mother/foetus and neonate, increased CV risk in the mother, and increased risk of DM2 in the mother and child. Therefore, proper postpartum reassessment and multidisciplinary collaboration (endocrinology, family and community medicine, nursing/education, midwifery, nutrition, obstetrics, paediatrics) is essential.
In women at risk of GD, the following measures are recommended before pregnancy: smoking cessation, weight and blood pressure control, lifestyle measures and optimisation of maternal weight. In addition, basal blood glucose, HbA1c and TSH should be determined and iodine and folic acid supplementation should be initiated.
Diagnostic screening is recommended in the first trimester in women at high risk of GD and at 24 weeks, on a universal basis. The initial treatment consists of lifestyle measures, which achieve adequate control in 80% of cases. If medical treatment is necessary, only insulin therapy (basal insulins: detemir, glargine U100/U300, degludec; rapid acting insulin analogues) is advised, as other drugs are not authorised.10
Postpartum assessment is essential because GD poses a high risk for developing DM2, and periodic reassessment (every 1–3 years) is necessary if the postpartum oral glucose tolerance test is normal. Reclassification will preferably be done with a 75g oral glucose tolerance test (4–12 weeks postpartum), using standard diagnostic criteria. Alternatively, HbA1c and basal glycaemia can be measured.10
In women without diabetes, lifestyle measures, weight control and smoking cessation are advised, and metformin should be considered if there is abnormal glucose tolerance and other CVRFs. If the diagnosis is DM2, treatment will be carried out in a comprehensive approach. If another type of diabetes is suspected, the patient will be referred to endocrinology for assessment.
ConclusionThe document sets out practical recommendations based on the latest available evidence for the management of people with DM2.
FundingThis article did not receive funding.
Conflicts of interestThe authors declare that they have no conflicts of interest related to this publication.