Adrenal gland carcinomas are uncommon tumors, with an incidence of 0.5–2 cases per million inhabitants/year and a bimodal distribution in early childhood and between the fourth and fifth decades of life. Most cases (40–60%) manifest with clinical signs secondary to hormone overproduction, and Cushing's syndrome with or without virilization is the most common expression in this regard. Thirty percent of the cases present with nonspecific symptoms derived from tumor growth (abdominal discomfort, nausea, vomiting, back pain, etc.), and up to 20–30% are diagnosed as adrenal incidentalomas.1–3
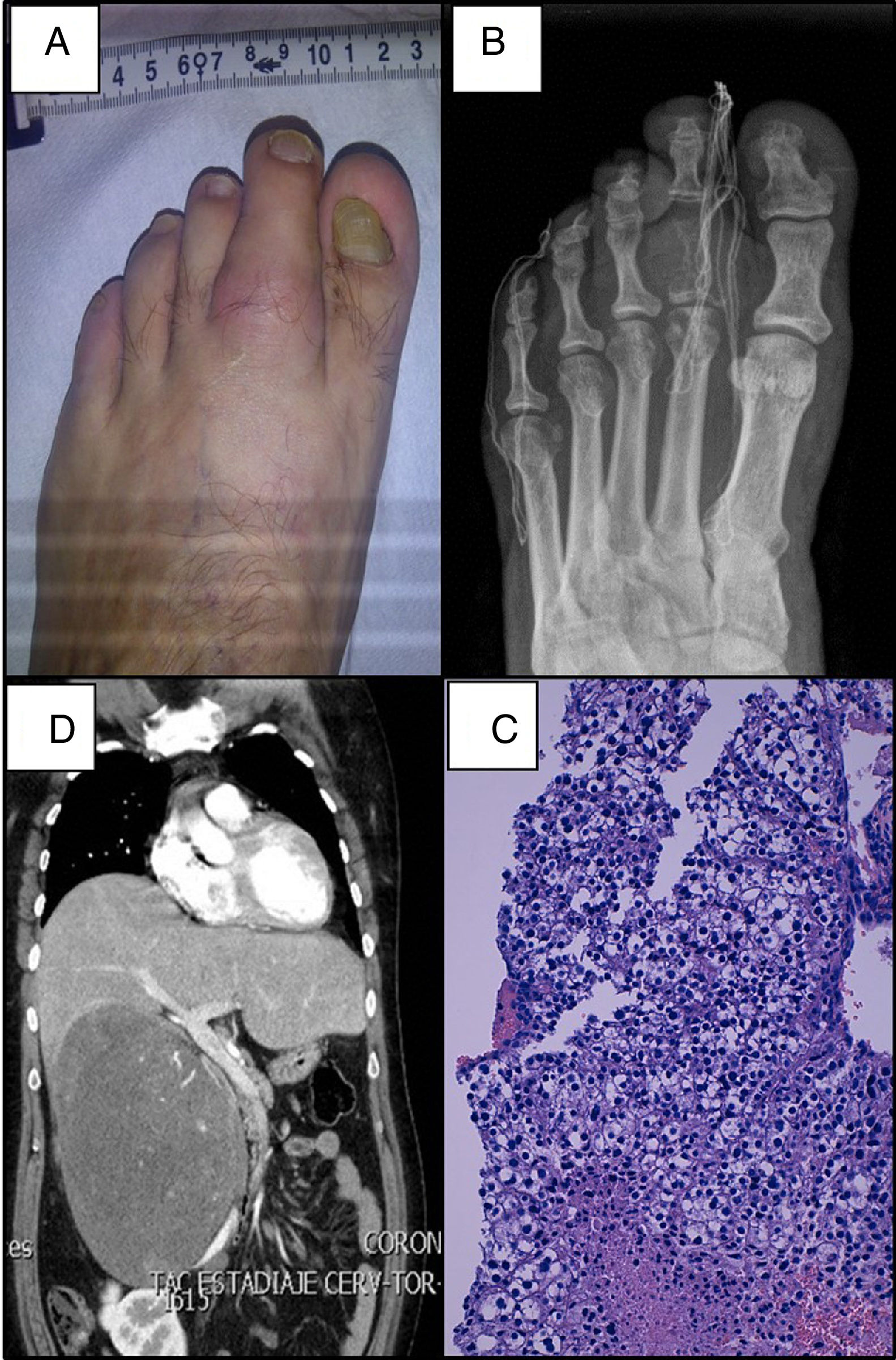
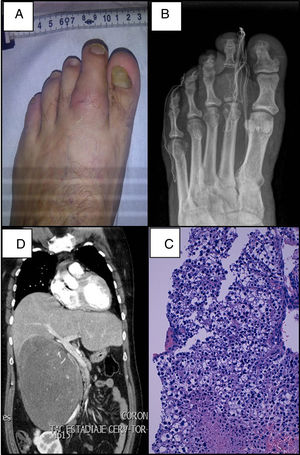
We report the case of a 47-year-old man consulting the Traumatology Department due to swelling and pain in the second toe of the left foot, with a history of trauma in that foot two months before (Fig. 1A). He reported no clinical symptoms in any other body region. The X-ray study revealed a lytic lesion in the proximal phalanx of the second toe (Fig. 1B). To complete the study, a biopsy was performed, revealing a neoplastic proliferation of atypical epithelial cells with round hyperchromatic nuclei and a clear cytoplasm, and focal necrosis (Fig. 1C). Immunohistochemistry proved positive for inhibin, vimentin, synaptophysin and melan A, and negative for cytokeratin AE1/AE3, CD10, EMA, CEA, chromogranin A, S100, p63 and TTF-1. On the other hand, Ki67 protein expression was 50%. These findings were consistent with metastasis of a carcinoma of adrenal gland origin.
(A) Tumefacción en el segundo dedo del pie izquierdo. (B) Lesión ósea lítica en la falange proximal del segundo dedo del pie. (C) Infiltración ósea por células tumorales, tinción hematoxilina-eosina (×100). (D) Tomografía axial computarizada que muestra gran masa suprarrenal derecha que produce desplazamiento de estructuras adyacentes.
Computed tomography in turn revealed a large heterogeneous right adrenal mass measuring 25cm×21×16cm in size, locoregional adenopathies, and lung lesions suggestive of metastasis (Fig. 1D). The physical examination revealed a palpable abdominal mass and bilateral gynecomastia. Laboratory tests showed normal cortisol and aldosterone levels with increased estrogen (17-beta estradiol 85pg/ml [normal reference 0–40pg/ml]), androgen (DHEA-S 6970ng/ml [800–5600ng/ml] and androstenedione concentrations >10ng/ml [0.3–2.9ng/ml]).
Local symptomatic treatment was provided with radiotherapy targeted to the bone lesion of the foot. Due to the advanced stage of the disease, systemic treatment was started with mitotane and streptozotocin, requiring up to a fourth line of chemotherapy due to disease progression, with the appearance of liver metastases and pulmonary progression. The patient died 13 months after diagnosis.
In males, isolated androgen-producing tumors usually go unnoticed due to the absence of symptoms. Only 1–3% of all functioning tumors are estrogen producers. These lesions may appear in men with gynecomastia, loss of libido, and testicular atrophy. The present case corresponded to an adrenal carcinoma producing androgens and estrogens, with gynecomastia on physical examination, and no other clinical signs derived from hormone hyperproduction.4
The extent of tumor disease at diagnosis is the main prognostic factor in adrenal carcinoma. The two main staging systems are that published in 2004 by the Union Internationale Contre le Cancer (UICC) and the World Health Organization, and the system proposed by the European Network for the Study of Adrenal Tumors (ENSAT) in 2008. The latter system differentiates metastatic disease due to its poor prognosis, with the inclusion in stage IV only of those tumors with distant metastatic spread, while stage III includes locally advanced disease. The 5-year survival rate is 50% in stage III and only 13% in stage IV. Apart from tumor stage, other important prognostic factors include the mitotic index and Ki67. Likewise, advances in molecular biology have facilitated the identification of molecular subgroups with a better or poorer prognosis, which could help develop new markers and guided therapies.5,6
Approximately 25% of all adrenal carcinomas can present in stage IV, with metastases at the time of diagnosis, mainly in the lungs (40–80%) and liver (40–90%).2 Bone metastases are less common, with an incidence ranging from 5 to 20% depending on the published series, the most common being in the pelvic region or spinal column.7,8 A review of the literature yielded no cases corresponding to metastases in the bones of the foot. Surgery with complete tumor resection is the only treatment option that can prove curative in the early stages of the disease. In advanced stages, the course is usually very aggressive, with a mean patient survival of 12 months. In such stages, mitotane and chemotherapy are the mainstays of treatment. Response is poor, however, and the 5-year survival rate is only 13%.4,9 In recent years, drugs aimed at the molecular targets involved in the development of cancer (mTOR inhibitors such as temsirolimus or everolimus, or tyrosine kinase inhibitors such as sunitinib) have been investigated, though with not very promising results to date.10
Please cite this article as: Bellido V, Larrañaga I, Vazquez F, Velasco V, Gaztambide S. Metástasis ósea en el pie como presentación clínica de un carcinoma suprarrenal. Endocrinol Diabetes Nutr. 2018;65:418–419.