Hyperglycemia is very common in hospitalized patients and is associated with worse clinical outcomes.
AimsWe implemented a clinical and educational program to improve the overall glycemic control during hospital admission, and, in patients with HbA1c > 8%, to improve their metabolic control after hospital admission.
MethodsNon-critical patients admitted to cardiovascular areas between October-2017 and February-2019. The program was led by an advanced nurse practitioner (ANP) and included a semiautomated insulin prescription tool. Program in 3 phases: 1) observation of routine practice, 2) implementation, and 3) follow-up after discharge.
ResultsDuring the implementation phase the availability of HbA1c increased from 42 to 81%, and the ANP directly intervened in 73/685 patients (11%), facilitating treatment progression at discharge in 48% (de novo insulin in 36%). One-year after discharge, HbA1c in patients who were admitted during the observation phase with HbA1c > 8% (n = 101) was higher than similar patients admitted during implementation phase (8,6 ± 1,5 vs. 7,3 ± 1,2%, respectively, p < 0,001). We evaluated 47710 point of care capillary blood glucose (POC-glucose) in two 9 months periods (one before, one during the program) in cardiology and cardiovascular surgery wards. POC-glucose ≥250 mg/dl (pre vs. during: cardiology 10,7 vs. 8,4%, and surgery 7,4 vs. 4,5%, both p < 0,05) and <70 mg/dl (2,3 vs. 0,8% y 1,5 vs 1%, p < 0,05), respectively, improved during the program.
ConclusionsThe program allowed improving inpatient glycemic control, detect patients with poor glycemic control, and optimize metabolic control 1-year after discharge.
La diabetes, o la hiperglucemia, es altamente prevalente en pacientes hospitalizados, asociándose con peores resultados clínicos.
ObjetivosImplementar un programa hospitalario de atención y educación terapéutica para mejorar el control glucémico medio y en pacientes ingresados con hemoglobina glucosilada (HbA1c) > 8% y mejorar su control metabólico tras el alta.
MétodosSe incluyó a pacientes no críticos ingresados en áreas cardiovasculares entre octubre del 2017 y febrero del 2019. El programa fue liderado por una enfermera de práctica avanzada (EPA) e incluía una herramienta semiautomática de prescripción de insulina. El programa tenía tres fases: 1) observación de práctica habitual, 2) implementación y 3) seguimiento-transición postalta.
ResultadosDurante la fase de implementación incrementó la disponibilidad de HbA1c (81 vs. 42% previo) en pacientes con diabetes y la EPA intervino directamente en 73/685 (11%) pacientes con HbA1c > 8%, modificando el tratamiento al alta en un 48% (insulina de novo 36%). Un año después del alta, la HbA1c de pacientes con mal control en fase de observación (n = 101) fue superior a los de fase implementación (8,6 ± 1,5 vs 7,3 ± 1,2 %, p < 0,001). Evaluamos 47710 glicemias capilares de dos periodos de 9 meses (antes y durante el programa). El porcentaje de glicemias ≥250 mg/dl (pre vs. durante: cardiología 10,7 vs. 8,4% y cirugía 7,4 vs. 4,5%, ambos p < 0,05) y <70 mg/dl (2,3 vs. 0,8% y 1,5 vs 1%, p < 0,05), respectivamente, mejoró durante el programa.
ConclusionesEl programa permitió mejorar el control glucémico durante el ingreso, maximizar la detección de pacientes mal controlados, y optimizar su control metabólico 1 año tras el alta.
People with diabetes mellitus (DM) are more likely to be hospitalised due to comorbidities and complications particular to their disease.1 It is estimated that up to 35% of all hospitalised patients have diabetes.2 Several observational studies have shown that hyperglycaemia in hospitalised patients, even in the absence of a known diagnosis of diabetes, is associated with higher mortality and a longer mean hospital stay.3,4 Despite this, hospital management of patients with diabetes is a common problem, and blood glucose control is often considered a less important objective than the reason for admission.5
Consensus statements and clinical practice guidelines for blood glucose control in non-critically ill hospitalised patients recommend regimens that consider baseline and prandial insulin needs versus traditional sliding-scale regimens.6–8 Despite these recommendations, basal-bolus therapy is perceived as complex, and therefore its use in blood glucose control has been limited at many hospitals.9–11 Some of the problems identified with its more extensive use include fear of hypoglycaemia, leading to insufficient starting doses, and inertia in relation to routinely adjusting doses according to the changing requirements of hospitalised patients.12
Hospital discharge is another crucial moment for a person with DM that is known or diagnosed on admission. There should be a structured, personalised discharge plan6 to avoid an extended hospital stay, reduce rates of readmission and increase patient satisfaction.13 The patient and/or family should receive treatment education (TE) suited to the home treatment prescribed, especially if it differs from what they had previously. In addition, it is considered key for hospital staff to ensure suitable monitoring of patients with diabetes until the follow-up visit by the primary care (PC) team and/or endocrinologist/internist who will monitor the patient on an outpatient basis.14 Hospital DM management programmes can yield better outcomes and cost savings, and teams specialising in diabetes can help to reduce readmission rates and duration of hospital stay, especially if they are involved in a patient's care from admission onwards.15
To address these problems and improve the care of people with diabetes who are admitted to hospital, and people with no known diagnosis of diabetes who develop hyperglycaemia requiring an insulin regimen, we proposed as an objective designing, implementing and evaluating a standardised programme for care and TE during hospitalisation (PCTE-Hospitalisation) on cardiovascular wards, which was led by an advanced nurse practitioner (ANP) in diabetes and cardiovascular risk. This manuscript reports the results of this programme.
Material and methodsThe PCTE-Hospitalisation is an interdisciplinary, multidisciplinary programme planned by the hospital's cardiovascular risk group. The programme is led by an ANP who works together with referring endocrinologists as well as medical and nursing staff to care for patients admitted to each ward. The programme was started in October 2017; it was originally planned with a duration of three years and was implemented in cardiology, cardiovascular surgery and neurology (cerebrovascular disease) hospitalisation wards at Hospital Clínic de Barcelona [Clinical Hospital of Barcelona]. The programme is aimed at all hospitalised patients with diabetes (known or unknown) or stress-induced hyperglycaemia (blood glucose >180 mg/dl on three consecutive occasions) requiring capillary blood glucose monitoring and an insulin regimen. The characteristics and outcomes of patients with diabetes and glycosylated haemoglobin (HbA1c) >8%, an arbitrary level of metabolic control that in this programme was determined to be a reason for personalised actions for improvement, are presented in more detail. Patients with limitation of therapeutic effort were excluded. This clinical research project was approved by the independent ethics committee (HCB/2020/1139). The programme is currently used in routine clinical practice.
Programme objectivesObjective 1: General improvement in inpatient blood glucose control. An insulin calculator (IC) was implemented and made available to prescribing physicians to help safely standardise prescribing of basal-bolus insulin. Insulin glargine U-100 (in a single baseline dose) and rapid-acting insulin analogues (such as prandial insulin) were used. The variable insulin regimens were reviewed, updated, improved or made safer (Appendix B supplementary material) for patients in whom use of the IC was not believed to be indicated and for physicians who decided not to use it. The IC is incorporated into the hospital medical prescription information system and its dose-calculation algorithm is an adaptation of the current recommendations6 (Appendix B supplementary material). The process of training, supervising and implementing the IC is coordinated by the ANP (Appendix B supplementary material).
Objective 2: Identification of patients with diabetes and chronic poor control. The ANP worked on modifying protocols and laboratory panels on admission so that patients with diabetes (or hyperglycaemia) had recent information available on their degree of blood glucose control (HbA1c). Patients with HbA1c >8% underwent a personalised evaluation by the ANP to determine their educational needs and facilitate early planning of their need for a change of treatment on discharge, including de novo insulin therapy or insulin regimen intensification.
Objective 3: Improvement of the transition to discharge. For patients evaluated on a personalised basis, the ANP recorded educational activities, treatment changes and recommendations on discharge for the patient and/or responsible medical team in hospital discharge reports. The ANP also scheduled these patients for an outpatient appointment one to two weeks after discharge.
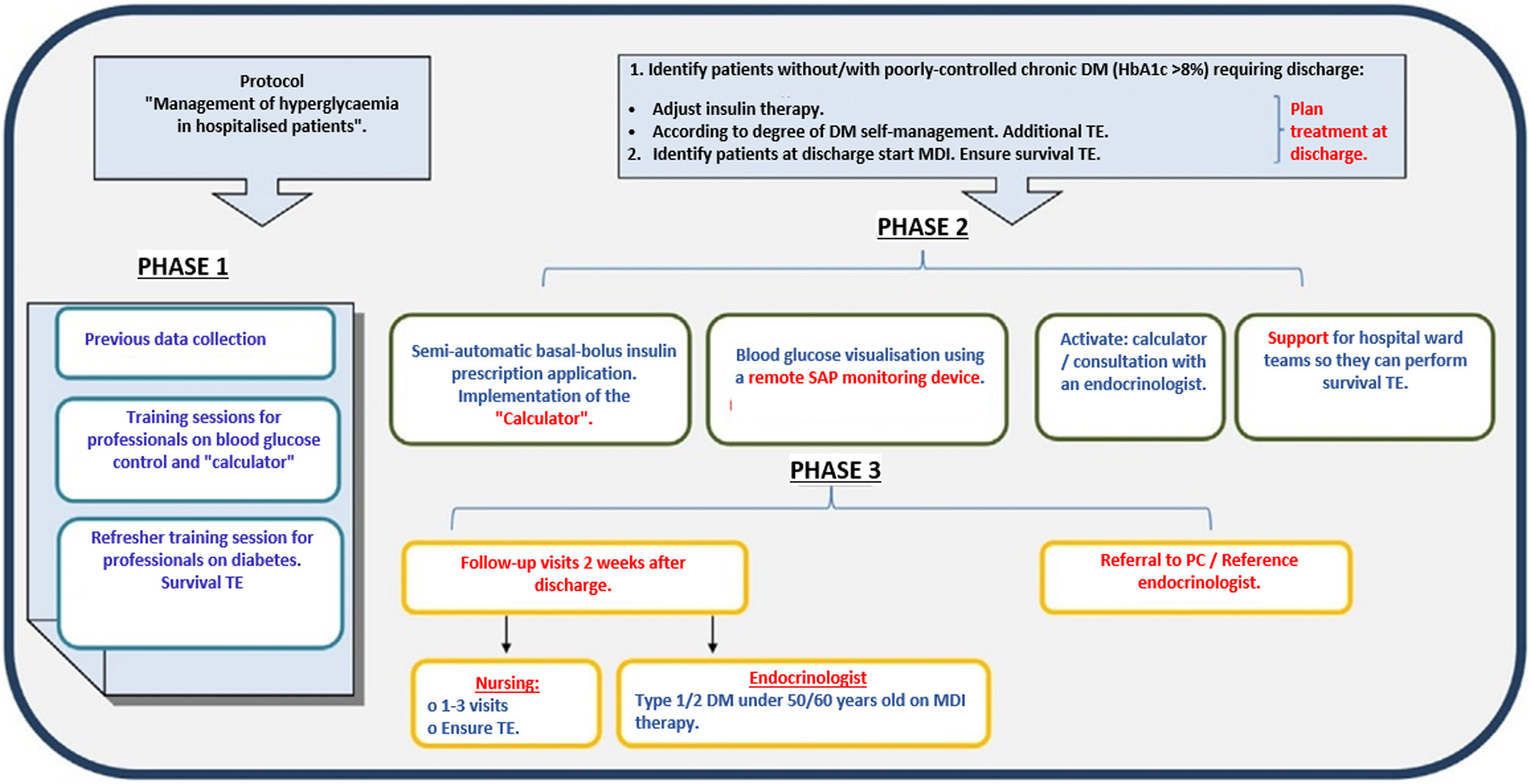
Programme phases/periods (Fig. 1). The phases of the programme, and the key times during which the data we report were collected, the analysis of which enabled us to evaluate achievement of prior objectives, are described below:
- a
Phase 0: PCTE-Hospitalisation pre-implementation. A nine-month period (January to September 2017) before implementing the PCTE-Hospitalisation. The capillary blood glucose checks performed and reported in the information system were collected from this period.
- b
Phase 1: PCTE-Hospitalisation. This was a three-month period (October to December 2017) for training of professionals and observation on hospitalisation wards of prior regular clinical practice in admitted patients with diabetes and HbA1c >8%.
- c
Phase 2: PCTE-Hospitalisation execution or implementation. This was a 12-month period (February 2018 to February 2019) for executing the programme. It consisted of implementation and promotion of the use of the insulin calculator, daily work by the ANP with professionals on hospitalisation wards, and personalised work with patients with DM and HbA1c >8%. During the first nine months of this phase, information was collected on blood glucose control in admitted patients so that it could be compared to Phase 0 of the programme.
- d
Phase 3: PCTE-Hospitalisation post-discharge. This was a 12-month period after hospital discharge. Up to three outpatient follow-up visits were held with the ANP one to two, four to six and six to eight weeks after discharge by patients requiring personalised intervention for a change or adaptation/improvement in insulin therapy. Subsequently, patients were discharged from the programme and referred to the primary care team (physician and/or nurse), or the referring endocrinologist or internist.
Phases of the Leyenda programme. The main phases of the programme are shown: Phase 1, observation of routine practice; Phase 2, execution; Phase 3, post-discharge. DM: diabetes mellitus; MDI: multiple-dose insulin; PCC: primary care centre; SAP: hospital system for electronic medical record management; TE: treatment education.
To evaluate the programme, we considered clinical data that was specifically collected and data from daily capillary blood glucose checks recorded automatically by ward nursing staff in the electronic medical record as part of routine care. The variables collected were: mean age; gender (male/female); duration of hospital stay in days; drug treatment (non-insulin antidiabetic drugs, baseline insulin or multiple-dose insulin) and non-drug treatment (diet) for diabetes, before and during admission; capillary blood glucose checks during admission (mg/dl); and HbA1c (%) on admission and three, six and 12 months after admission. Our hospital uses the Nova Pro® glucose meter (Menarini Diagnostics, Florence, Italy) to measure capillary blood glucose on hospitalisation wards. In order to learn the opinion of the professionals from the participating wards, an ad hoc general satisfaction survey with the programme and with the role of the ANP was conducted.
Statistical analysisData are presented in terms of mean ± standard deviation, median (interquartile range), proportions or absolute frequencies and percentages, as applicable based on the distribution and nature of the variables. The χ2 test, Mann–Whitney U test and Student's t test were used for categorical variables, continuous variables with a non-normal distribution and continuous variables with a normal distribution, respectively. The results are represented with a p value (<0.05 being statistically significant) and estimated confidence intervals. Data analysis was performed with SAS®, version 9.4 (SAS Institute Inc., Cary, North Carolina).
ResultsAppendix B Table 1 and Supplementary Table 1 show the clinical characteristics of patients with diabetes admitted in Phase 1. The mean age was 71 years, 70% were men and HbA1c was ordered on admission in 42% of the patients. Some 20% had HbA1c >8%. The basal-bolus insulin regimen was prescribed in 48% of patients in the first 48 hours following admission, subsequently increasing to 57%. We found some differences in the use of a basal-bolus regimen after the first 48 hours of admission, at rates under 30%-35% in surgery and neurology and as high as 87% in cardiology (Appendix B Supplementary Table 1).
Table 1 also shows the clinical characteristics of the patients with diabetes admitted during Phase 2. The mean age and the proportion of males were similar to Phase 1. In this phase, the availability of HbA1c on admission was 81%. Some 30% of patients had HbA1c >8% (with 15% >9%); the mean for this group of patients with HbA1c >8% was 9.3 ± 1.3% (Appendix B Supplementary Table 2). The ANP directly intervened (Table 1, Phase 2 of execution-ANP) in 73 patients (11%). In total, 84% of them had HbA1c >8%, 55% were on outpatient treatment with non-insulin antidiabetic drugs, and 30% were receiving two or more doses of insulin. On discharge, treatment intensification was seen in 48% of these patients and 36% of them received de novo insulin therapy (Table 1).
Characteristics, initial treatment and treatment at discharge of patients with diabetes in the different phases.
| PHASE 1 OBSERVATION (n = 101) | PHASE 2 EXECUTION (n = 685) | PHASE 2 EXECUTION-ANP (n = 73) | |
|---|---|---|---|
| Age, years | 71 ± 11 | 69 ± 12 | 63 ± 12b |
| Male sex | 70 (70) | 483 (71) | 57 (78) |
| HbA1c available on admission | 42 (42) | 554 (81) | 73 (100)b |
| HbA1c (%) on admission | 7.2 ± 1.7 | 7.4 ± 1.5a | 9.2 ± 1.9b |
| HbA1c on admission >8% | 16 (20) | 166 (30)a | 61 (84)b |
| Prior treatment | |||
| Diet/NIADs | 49 (49) | 391 (57) | 40 (55) |
| NIADs + Basal | 21 (21) | 120 (18) | 11 (15) |
| 2/3 doses/MDI | 29 (29) | 171 (25) | 22 (30) |
| Treatment on discharge | |||
| Diet/NIADs | 41 (44) | 329 (49) | 13 (18)b |
| NIADs + Basal | 17 (18) | 116 (17) | 18 (25) |
| 2/3 doses/MDI | 33 (36) | 224 (34) | 42 (58) |
| General treatment progression | 11 (11) | 85 (13) | 35 (48)b |
| De novo insulin therapy | 6 (12) | 54 (14) | 27 (36)b |
Basal: basal insulin; MDI: multiple-dose insulin or basal-bolus therapy; NIADs: non-insulin antidiabetic drugs.
The data indicate mean ± SD or n (%) or median (Q1-Q3).
The characteristics of patients included in the different phases are shown: 1) observation of prior clinical practice (n = 101); 2) programme execution phase; and 3) patients from execution requiring direct personalised care from the advanced nurse practitioner (ANP) in Diabetes and Cardiovascular Risk.
To evaluate programme objective 3 (transition to discharge), we compared changes over time in blood glucose control in patients who had HbA1c >8%. HbA1c one year after discharge in patients identified in Phase 1 was reduced after hospital discharge, but still persisted at high levels (9.9 ± 2 versus 8.6 ± 1.5; p = 0.0001). However, in patients followed up after the implementation of the programme (Phase 3), there was a significant reduction in HbA1c after one year, with attainment of suitable levels for this patient type (9.2% ± 1.9% versus 7.3% ± 1.2%; p = 0.0001) (Table 2). The percentage of these patients who showed an HbA1c less than 6.5% or 7% after three, six and 12 months ranged from 14%-19% to 40%-49%, respectively.
Blood glucose control (HbA1c) on admission and in the year after discharge in admitted patients with diabetes.
| [0,2–3]PHASE 1 OBSERVATION N = 101 | [0,4–5]PHASE 2-3 EXECUTION-ANP N = 73* | |||
|---|---|---|---|---|
| Admission | Discharge | Admission | Discharge | |
| Mean age ± SD | 71 ± 11 | 63 ± 12 | ||
| HbA1c ordered | 42 (42) | 73 (100)a | ||
| HbA1c >8% | 16 (20) | 61 (84)a | ||
| HbA1c | 9.9 ± 2 | 9.2 ± 1.9 | ||
| HbA1c + 3 months | -- | 8.4 ± 1.5 | -- | 7.4 ± 1.1b |
| HbA1c + 6 months | -- | 8.7 ± 1.2 | -- | 7.3 ± 1.4b |
| HbA1c + 12 months | -- | 8.6 ± 1.5 | -- | 7.3 ± 1.2b |
| Treatment | ||||
| Diet/NIADs | 49 (49) | 41 (44) | 44 (55) | 13 (17)b |
| NIADs + Basal | 21 (21) | 17 (18) | 11 (15) | 18 (25) |
| 2/3 doses — MDI | 29 (29) | 33 (36) | 22 (30) | 42 (58) |
| De novo insulin therapy | -- | 6 (12) | -- | 27 (36)a |
Basal: basal insulin; MDI: multiple-dose insulin or basal-bolus therapy; NIADs: non-insulin antidiabetic drugs.
The data indicate mean ± SD or n (%).
The characteristics of patients included in two phases are shown: 1) patients from prior clinical practice observation (n = 101); and 2) patients from execution requiring direct personalised care from the advanced nurse practitioner (ANP) in Diabetes and Cardiovascular Risk.
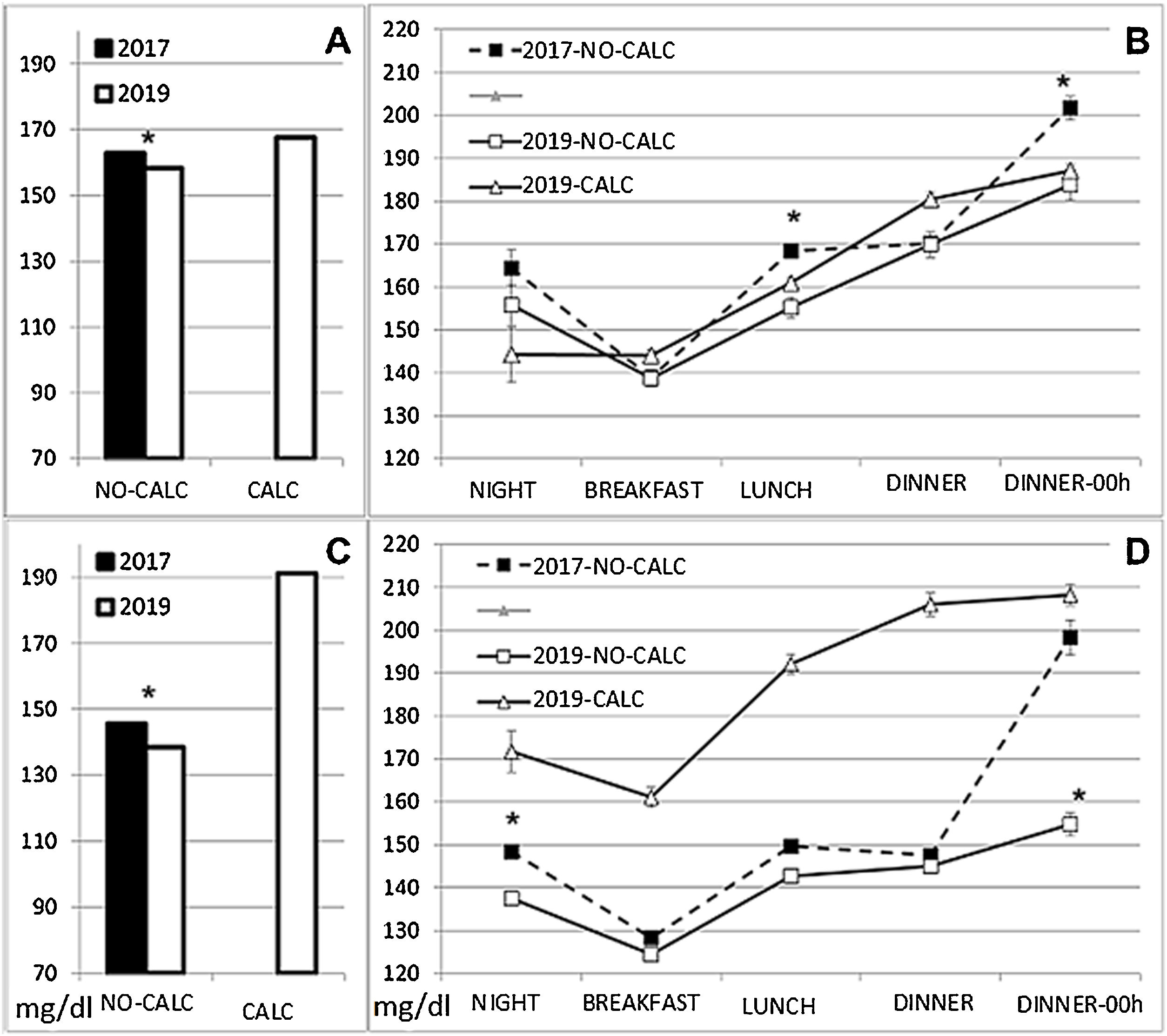
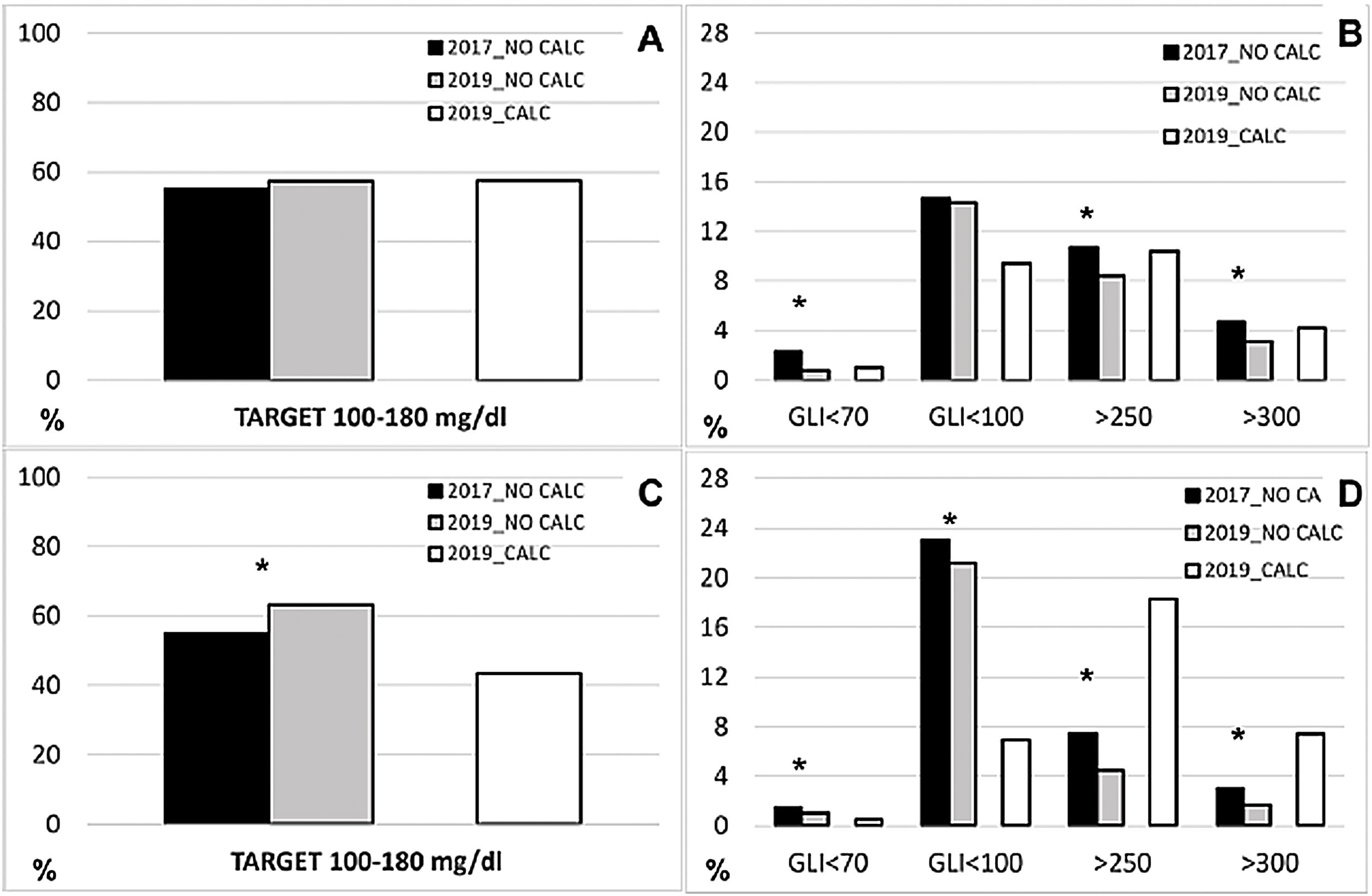
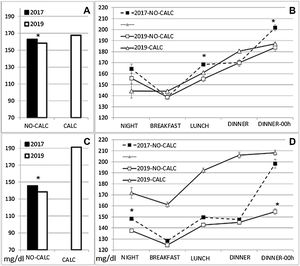
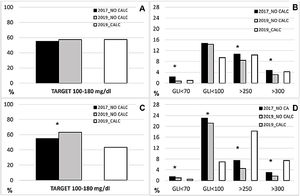
With the aim of determining whether there was an overall improvement in blood glucose control during the programme, we compared hospital blood glucose levels in two nine-month periods during Phase 0 and Phase 2. We evaluated a total of 47,710 capillary blood glucose checks for a total of 1,997 patients from cardiology and cardiovascular surgery wards (Appendix B Supplementary Table 3). On the cardiology ward during Phase 2 (possibility of calculator use), we found that 9,896 capillary blood glucose checks (78% of the total, n = 12,668) in 234 patients (48% of the total, n = 485) were linked to insulin prescribing with a calculator. In cardiovascular surgery (CVS) these totalled 3,971 capillary blood glucose checks (27% of the total, n = 14,484) from 101 patients (15% of the total, n = 681). Mean blood glucose levels in patients without an IC were higher in Phase 0 than during Phase 2, with some differences found at different periods of the day (Fig. 2). We saw a significant difference in the prevalence of hypoglycaemia and of blood glucose levels greater than 250 mg/dl, both in cardiology (Phase 0 versus Phase 2 blood glucose ≤70 mg/dl 2.3% versus 0.8%; >250 mg/dl 10.7% versus 8.4%, both p < 0.05) and in CVS (1.5% versus 1%; 7.4% versus 4.5%, respectively, both p < 0.05). However, there were no differences in the percentage of 100-180 mg/dl blood glucose levels in cardiology (55% versus 57.1%, p = 0.079), although this rate did improve in CVS (55.1% versus 63.1%, p < 0.001) (Fig. 3). Mean blood glucose levels were higher in patients prescribed insulin with an IC, especially in CVS (168 mg/dl in cardiology; 191 mg/dl in CVS). These patients were on more complex outpatient treatment for their diabetes: in CVS, 50% of them received multiple-dose insulin, 21% received basal insulin and 28% received non-insulin antidiabetic drugs; and in cardiology, 27% received multiple-dose insulin, 17% received basal insulin and 53% received non-insulin antidiabetic drugs.
Of the 160 surveys sent out, 51 were completed; 62.75% of respondents were nursing staff (n = 32). Dissemination (80.39%), usefulness (96.08%) and communication with the endocrinology team (90.2%) were rated "very positively". Some 86.3% rated the implementation of the diabetes survival treatment education programme "quite useful" or "very useful", and some 78.4% rated the resources used to disseminate the programme "positively" or "very positively". Of the survey respondents, 90.2% considered the support of the ANP to be "quite/very useful", and 92.16% of the professionals answered that the programme had improved care for their patients with diabetes from the ward/unit where they worked.
DiscussionWe have reported the results of a clinical initiative to improve blood glucose control in patients with diabetes (or with hyperglycaemia subject to insulin therapy), hospitalised on cardiovascular wards or areas and their transition to discharge. We integrated the leadership of an advanced nurse practitioner into the care team and used a tool incorporated into the prescribing system so that any professional could initiate basal-bolus insulin therapy in a standardised, safe manner.
The programme was designed based on evidence from similar programmes,16,17 but with the difference that it included the IC. The aim of the IC is to standardise safe prescribing of insulin and to help eliminate a reactive strategy for blood glucose control: sliding-scale rapid-acting insulin regimens. In recent years, technology in this sphere has advanced in hospitals. GlucoTab18 has proven safe and efficient with good acceptance among healthcare professionals,19 and Glucommander improved blood glucose control with a lower incidence of episodes of hypoglycaemia. These systems can improve adherence to treatment with basal-bolus insulin without increasing rates of episodes of hypoglycaemia.20,21 The use of electronic blood glucose management systems is safe and effective with quick implementation by professionals, enabling treatment standardisation and minimising the need for experts in inpatient diabetes management.22,23
In this programme, collection of information and incorporation of the IC into clinical practice were possible thanks to coordinated efforts with professionals from the hospital's information systems department. We were able to evaluate tens of thousands of capillary blood glucose checks recorded annually by nursing professionals, and we offer the first data from a complex ongoing analysis. The programme was beneficial in that it reduced blood glucose levels ≤70 mg/dl (with reduction of episodes of hypoglycaemia being a priority objective in insulin prescribing) and reduced blood glucose levels >250 mg/dl in patients with insulin prescribed outside of the use of the IC. We hypothesise that general awareness-raising on improvements in control during the programme, the day-to-day work of the ANP and the switch from variable insulin regimens to a safer, more personalised version might partly account for these improvements. For patients with diabetes in whom the IC was used, unfortunately, we lacked a prior control, as the IC was not used prior to the programme. However, we did find that patients prescribed insulin with the calculator were more complex patients, especially in vascular surgery, due to their pre-admission insulin therapy. This explains their higher mean blood glucose levels compared to patients in whom the IC was not used (Figs. 2 and 3). Finally, use of the calculator was not uniform, varying according to professional background (lower in CVS versus cardiology), despite being safe in both settings, as demonstrated by a reduction in episodes of hypoglycaemia (<70 mg/dl). This is a challenge for improvement, as the evidence indicates that surgical patients could derive even greater benefits24,25 from inpatient blood glucose control.
Our real clinical practice data showed the use during hospitalisation of sliding-scale rapid-acting insulin regimens (mean over 30% at least 48 hours after admission to a conventional ward), despite the fact that a basal-bolus regimen represents the safest, most effective strategy.26,27 The data also confirmed that approximately 30% of patients admitted to "cardiovascular" wards have DM (HbA1c >8%, 20%-30%), and that information on their ongoing blood glucose control available on admission is limited (HbA1c ordered in 42%).9 Adding HbA1c to laboratory testing on admission increased its availability (81%) in Phase 2 of the programme. Knowledge of the patient's HbA1c offers an opportunity to plan better treatment on discharge and is an essential aid in decision-making.28 HbA1c levels greater than or equal to 8% identify patients whose treatment progresses after hospitalisation.29 In addition, this cut-off point (8%) is perhaps the maximum that can be recommended, even for cardiovascular patients of this mean age, and it is a convenient point that identifies a number of individuals that can be managed by a single ANP in a programme with a significant workload. The combined strategy, identification and personalised work, and transition enabled a sustained, consistent improvement (mean HbA1c <7.5%, with 40% <7%), a year after admission compared to Phase 1 (mean HbA1c 8.5%). Scientific associations recommend putting this improvement in practice, either through a specialised nurse or jointly with the endocrinologist.6,14
Continuing education of professionals is an important challenge due to constant changes over time in DM treatment and high turnover of hospitalisation ward staff. In this programme, training of physicians and nurses, accompanied by a set of standardised orders for prescribing insulin, helped to safely improve blood glucose control in hospitalised patients treated with subcutaneous insulin.30 In addition, consensuses of experts in diabetes such as the Sociedad Española de Diabetes [Spanish Diabetes Society] defend the role of the expert nurse in diabetes.31 There is evidence of the usefulness of the ANP in diabetes in the promotion of greater use of basal-bolus therapy32 and better blood glucose control before discharge.33 Blood glucose control can be managed by nurses and standardised protocols,34 and this form of management is feasible, safe and non-inferior to physician-directed care.35 Perception on the part of professionals was highly satisfactory, reflecting support for this nursing professional and for the programme as a whole.
This study had limitations. We did not report blood glucose results in the neurology area. The complexity of analysing tens of thousands of data points in patients most often treated with intravenous insulin and hourly blood glucose checks (the IC is also used in this scenario) prevents us from offering data for these patients at this time. Analysis of the capillary blood glucose results recorded in the system by nursing and of the variables collected using the IC tool is incomplete, but continuous improvement of protocols will enable us to be more agile and arrive at individual data. This improvement will also facilitate the incorporation of algorithms in phenotypes of special patients (for example, medical or surgical, corticosteroid therapy [in particular, at high doses], enteral/parenteral nutrition, etc.), and advancement towards achievement of more intelligent systems for control, including in real time. We compared nine-month periods from different years (2017 and 2019). The groups of patients whose blood glucose levels were analysed may differ with regard to characteristics of which we are not aware. However, with the exception of the number of patients, which was higher in 2019, it is possible that the average phenotype of the patient who is admitted to these wards and has diabetes or hyperglycaemia subject to blood glucose control and insulin prescription should not be very different, especially considering prolonged periods of time. Finally, we did not offer data on percentages of blood glucose levels in the range accepted as a target in hospitalised patients, i.e., 140-180 mg/dl, although we believe that percentages of values of 100-180 mg/dl could be a valid approximation.
In summary, the programme facilitated the identification of patients with diabetes and ongoing poor control, provided them with personalised care and thus improved their control in the year after discharge. We were able to safely extend the insulin treatment of choice (basal-bolus) and reduce rates of episodes of hypoglycaemia and of blood glucose levels over 250 mg/dl. This study was coordinated between different types of professional (physicians and nurses) and specialisations (cardiology, neurology, CVS and endocrinology), was led by an expert nurse and used tools that facilitated prescription and use of information collected and ensured care continuity.
FundingAmgen Inc., biotechnology, Thousand Oaks (California, US), supported this project without conditions.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We are grateful to Dr Josep Vidal and Dr Marta Sitges, Director and Medical Director of the Institut Clínic de Malalties Digestives i Metabòliques [Hospital Clínic Gastrointestinal and Metabolic Disease Institute] (ICMDM) and the Institut Clínic Cardiovascular [Hospital Clínic Cardiovascular Institute] (ICCV), respectively, for facilitating the implementation and development of the programme. We would like to thank all the medical, nursing, auxiliary and administrative staff on the cardiology, cardiovascular surgery, neurology and nephrology wards, where the programme was implemented. More importantly, we wish to thank the patients, who were foremost in our thoughts when we conceived of and implemented the programme, for their selfless participation.