Primary hyperparathyroidism (PHPT) remains underdiagnosed among patients with hypercalcemia, potentially causing increased morbidity.
ObjectiveTo identify in surgically operated patients the presence of overlooked hypercalcemia and patients with criteria for surgery (CFS) for PHPT at least one year prior to referral to Endocrinology, and to determine whether this diagnostic delay leads to increased morbidity.
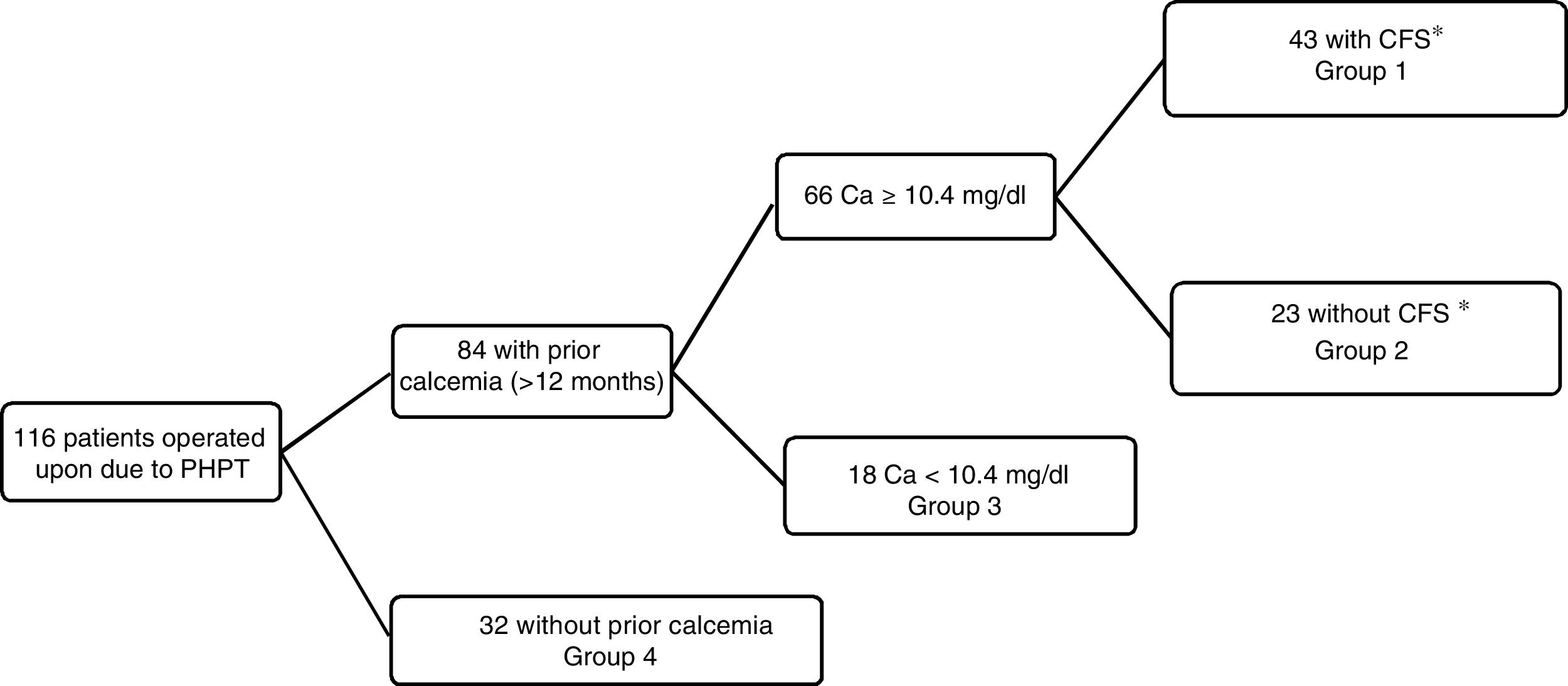
MethodsAn observational study was carried out in 116 consecutive patients. We evaluated electronic medical records registered at least 12 months prior to referral and divided them in four groups: hypercalcemia with CFS (group 1), hypercalcemia without CFS (group 2), normocalcemia (group 3), and cases without previous biochemical evaluation (group 4).
ResultsA total of 84 patients (72.4%) had a previous measurement of serum calcium at a time interval of ≥12 months. Sixty-six (56.9%) had hypercalcemia and 43 of them (37%) had ≥1 CFS, with an average delay of 57 months in receiving proper evaluation. Almost half of the calcemia measurements in group 1 had been made in the emergency room. Patients from group 1 were younger, and had a greater frequency of nephrolithiasis and renal impairment than patients in group 4. The serum calcium values at referral were similar in both groups and higher than the values found in patients from the other two groups.
DiscussionIn patients with PHPT and CFS, referral to an endocrinologist is made with an average delay of almost 5 years. The identified causes of this delay, which conditions more kidney disease, are unrecognized hypercalcemia and/or unawareness of the surgical criteria, while calcium elevations promote referral. Interventions are needed to avoid this delay in the diagnosis and resolution of PHPT.
El HPTP frecuentemente permanece sin diagnosticar en pacientes con hipercalcemia, lo que podría ocasionar un aumento de la morbilidad en estos sujetos.
ObjetivoIdentificar la presencia de hipercalcemia y de criterios de tratamiento quirúrgico (CTQ) no identificados desde al menos un año antes de su remisión a endocrinología en pacientes operados de HPTP. Valorar si este retraso terapéutico se asocia a mayor morbilidad.
MétodosEstudio observacional en 116 pacientes consecutivos. Mediante la revisión de los registros anteriores a 12 meses previos a su derivación a endocrinología se dividieron en 4 grupos: hipercalcemia con CTQ (grupo 1, n=43), hipercalcemia sin CTQ (grupo 2, n=23), calcemias normales (grupo 3, n=18) o ausencia de calcemias en dichos registros (grupo 4, n=32).
ResultadosEn 84 pacientes (72,4%) había calcemias previas, 66 (56,9%) con hipercalcemia, de ellos 43 (37%) con CTQ no valorados. La demora media hasta su remisión fue de 57 meses. Casi la mitad de las calcemias del grupo 1 procedían de urgencias. Respecto al grupo 4 los pacientes del grupo 1 tenían menor edad, mayor incidencia de nefrolitiasis e insuficiencia renal al remitírseles. Las calcemias en el momento de su derivación eran similares, superiores a las de los grupos 2 y 3.
DiscusiónLos pacientes con HPTP y CTQ se remiten a endocrinología con un retraso medio de 5 años. La inadvertencia de la hipercalcemia y/o el desconocimiento de los CTQ retrasan esta derivación, determinada por hipercalcemias superiores, y se asocian a una afectación renal más severa. Son precisas medidas correctoras para evitar este retraso en el diagnóstico y curación del HPTP.
In the past, primary hyperparathyroidism (PHPT) was considered to be an infrequent disorder. However, the number of diagnoses has increased exponentially since the late 1970s with the widespread use of multichannel analyzers, including the determination of calcemia. In previous decades, PHPT was identified through the kidney or bone complications associated with advanced stages of the disease,1 and the aforementioned diagnostic developments resulted in an avalanche of asymptomatic cases.2
The management of asymptomatic PHPT has been the subject of four consecutive consensuses since 1991, with changing criteria for indicating parathyroidectomy, the only definitive treatment generally performed.3 In all of these consensuses, patient age, the calcemia level and nephrolithiasis have been maintained as criteria for surgery. However, consideration of calciuria (and its limiting value) and bone density (and its location) has varied from one consensus to another.4–7 In 2016, the American Association of Endocrine Surgeons proposed parathyroidectomy in all cases in which such surgery has an acceptable risk weighed against benefit and cost-effectiveness versus patient monitoring and therapy with cinacalcet and antiresorptive drugs.8
Because of the increase in diagnoses, the most common presentation of PHPT nowadays corresponds to subclinical disease, which only manifests as commonly unnoticed laboratory test alterations, despite the fact that the disorder is the most common cause of hypercalcemia in non-hospitalized patients. This means that PHPT is an underdiagnosed and therefore undertreated disease, as shown by recent publications in which many patients with documented hypercalcemia remain undiagnosed.9,10 This diagnostic delay may favor the progression of PHPT, producing clear clinical manifestations, and may increase the risk of complications associated with the disease.
With the aim of analyzing this phenomenon, we conducted a retrospective review of a series of patients with PHPT subjected to surgery, based on an evaluation of the laboratory and clinical records prior to patient referral to the endocrinology clinic. The primary objective of the study was to identify delays in diagnosis and subsequent surgical treatment of at least one year until referral to the endocrinology clinic. The secondary objectives included evaluation of whether patients with a diagnostic delay have greater associated morbidity, or whether the latter is more severe than in patients who are referred earlier.
MethodsThe Clinical Research Ethics Committee (CREC) of the hospital authorized the present study. All patients had given written consent to surgery, as well as permission to use their disease-related data for research purposes.
This was a retrospective observational study including all patients undergoing surgery with a firm diagnosis of PHPT in a third-level hospital during the period from 1 February 2015 to 31 May 2018. The data were collected from the electronic health records of the patients. In all cases we evaluated the records corresponding to previous visits to other departments (including emergency and primary care), previous hospital admissions with their respective discharge reports, radiological examinations, and all laboratory test results accessible through the Osabide Global system. This system contains the health records referring to specialized care (outpatient and inpatient) of all patients since 2012, and allows access to episodes documented through primary care since the year 2003, as well as imaging tests, hospital discharge reports and laboratory test data since 1998. The presence of a diagnosis of nephrolithiasis/renal colic was specifically determined from the primary care records, with individual assessment of the events. From the biochemical parameters compiled since 1998 in the Omega system, we identified all calcemia values recorded before patient referral to the endocrinology clinic and their date. We also identified the alkaline phosphatase value closest to the moment of referral and also at the time of the first detection of elevated calcemia (if performed), the date of the first measurement of intact parathyroid hormone (PTH), and the plasma creatinine concentration in the test leading to referral to the clinic and also at the time of the first detection of elevated calcemia. In laboratory tests performed after 2010, the estimated glomerular filtration rate (eGFR) was obtained using the MDRD-4 formula.
Calcemia was measured using an automated autoanalyzer with an upper limit of normal (ULN) of 10.4mg/dl. Alkaline phosphatase was documented using the same methodology, with an ULN of 104IU/l in adults. Renal failure was defined as eGFR according to the MDRD-4 formula <60ml/min, and in the years before 2010 as creatinine >1.4mg/dl in women and >1.5mg/dl in men. Parathyroid hormone was measured using a commercial immunoassay with an ULN of 65pg/ml.
Twenty-four hour calciuria and densitometric studies were not recorded, since such data typically were not available on the date of the first hypercalcemia measurement or on the date of patient referral to the clinic. Another reason for not taking these data into consideration was that our retrospective study period covered years in which the different consensuses did not always include these parameters as criteria for surgical treatment, or assigned different limits to such parameters.7
The interval of up to 12 months between the first detection of hypercalcemia and patient referral to Endocrinology for evaluation was considered to be a correct measure. When this interval was longer than 12 months, it was considered to represent inappropriately delayed patient referral. This limit was applied due to the tendency of the referring physician to check hypercalcemia in a second test, usually within less than 12 months, and accompanied by a request for simultaneous PTH determination. In patients with prior hypercalcemia (defined as total serum calcium ≥10.4mg/dl more than 12 months before referral), we calculated the months between the first pathological measurement and patient referral to the endocrinology clinic, as well as the interval from the date of first hypercalcemia to the date of first PTH measurement. The interval between the last normal calcemia value recorded in the biochemical history and the first elevated value was also considered for the 49 patients for whom this information was available.
All patients were analyzed for the presence of the following four criteria for surgery (CFS), both on the date of the first detected hypercalcemia and at the time of referral: age ≤50 years at the time of analysis, calcemia ≥11.4mg/dl in patients over 50 years of age, nephrolithiasis (established from imaging techniques or documented renal colic), and renal failure according to the parameters defined above. Calciuria and densitometry were not assessed as criteria for the indication of parathyroidectomy due to the aforementioned reasons.
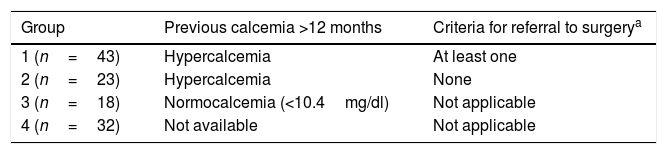
Patients with hypercalcemia documented at least one year before referral, and with at least one CFS, were placed in the inadequately delayed surgery group (group 1). Patients with prior hypercalcemia but none of the four CFS at that time were included in group 2. Patients with documented normal prior calcemia in turn were put into group 3, and those with no recorded previous calcemia values and a time to referral of over 12 months constituted group 4. Table 1 summarizes these four groups.
Definition of the four groups into which the 116 study participants were divided.
| Group | Previous calcemia >12 months | Criteria for referral to surgerya |
|---|---|---|
| 1 (n=43) | Hypercalcemia | At least one |
| 2 (n=23) | Hypercalcemia | None |
| 3 (n=18) | Normocalcemia (<10.4mg/dl) | Not applicable |
| 4 (n=32) | Not available | Not applicable |
Continuous variables (age, calcemia, time intervals and alkaline phosphatase) were reported as the mean and standard deviation (SD). Comparisons of such variables were made using the Student t-test. In the case of qualitative variables such as gender comparison or the presence of nephrolithiasis, we made use of the Fisher exact test. Statistical significance was considered for p<0.05. The SPSS version 23 statistical package (SPSS Inc., Chicago, IL, USA) was used throughout.
ResultsA total of 116 patients subjected to surgery due to PHPT at the same hospital in the period from 1 February 2015 to 31 May 2018 were analyzed.
Of these 116 patients, 84 (72.4%) had calcium measurements obtained over 12 months before the date of referral to the endocrinology clinic, while 32 (27.6%) did not. Of these 84 patients, 66 presented values in the hypercalcemia range (56.9% of the total) and 18 of them had calcemia <10.4g/dl (Fig. 1). The patients presenting hypercalcemia had a mean delay of 58 months (range: 14–166 months) until referral to the endocrinology clinic, counting from the date of this first pathological calcemia value. Seven of the patients (6% of the total) had a delay of over 10 years.
Of the 66 patients with confirmed hypercalcemia more than 12 months before evaluation, 23 (33.9%) had none of the defined CFS, while 43 of the 66 subjects (66.1%) had at least one CFS at the time of the detection of hypercalcemia. The criteria for surgery not considered at the time of the diagnosis of hypercalcemia were: 22 patients (51.2%) under 50 years of age, 22 (51.2%) with nephrolithiasis, 10 (23.3%) with calcemia ≥11.4mg/dl at that measurement, and 5 patients (11.6%) with eGFR <60ml/min. Ten patients (8.6% of the total) had two CFS, with the combination of nephrolithiasis and age being the most frequent presentation (7 cases; 6%), while three patients (2.6%) had three criteria for parathyroidectomy. The mean delay in referral to the endocrinology clinic of these 43 patients from the time of the evidence of hypercalcemia with CFS was 57 months (range: 14–132). This was similar to the delay of the 23 patients with prior hypercalcemia but none of the four CFS (61 months, range: 17–166; p=0.35). These laboratory tests – with results that went unnoticed despite the fact that the patients had CFS referring to PHPT - had been requested by the emergency room in 21 cases (48.8%), by family medicine in 7 (16.3%), Rheumatology in 3 (7%), Endocrinology in 2 (4.7%), Urology in 2 (4.7%), and by another 8 different specialties, with one case each (2.3%).
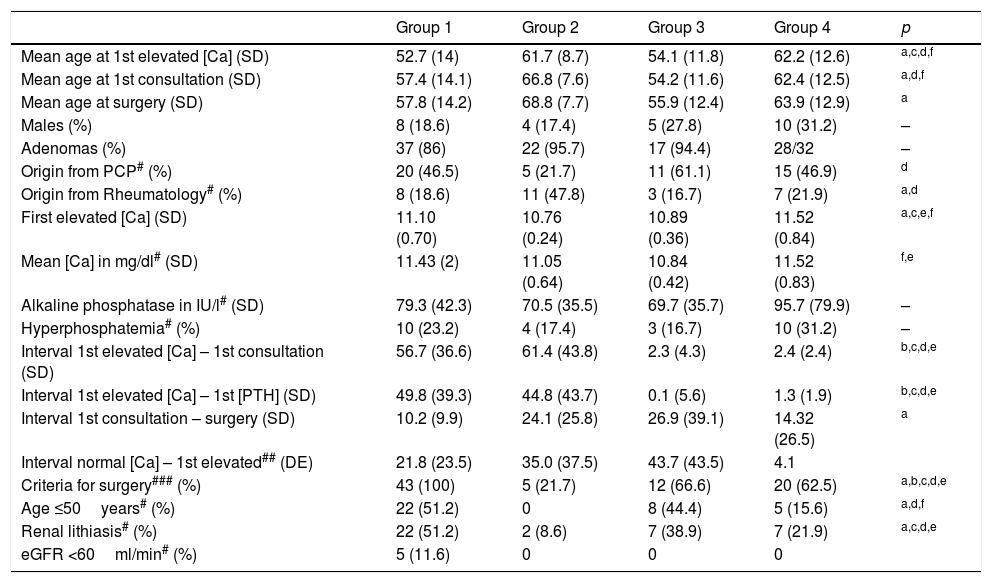
Both the age at which first hypercalcemia was shown and the ages at which the patients in group 1 were referred to the clinic and at which surgery was performed were significantly lower than in groups 2 and 4, but were not significantly different from the corresponding ages recorded in group 3.
The mean first hypercalcemia value recorded was significantly greater in group 1 than in group 2. This was expected, since calcemia ≥11.4mg/dl was a criterion for belonging to the former group, though hypercalcemia was even higher in group 4. This could indicate that the severity of hypercalcemia was one of the key criteria for deciding patient referral to the endocrinologist. The group 1 patients underwent surgery earlier, after a mean interval of 10 months from the first endocrinology visit, as compared to 24 months in group 2. This suggests that the former patients were prioritized because of their greater clinical and laboratory alterations. This interval was similar in group 4, possibly reflecting their more severe PHPT, as suggested by the serum calcium values. The mean time from first elevated calcemia to the first recorded request for PTH measurement was over three years in the first two groups, significantly longer than in the other two patient groups. This finding suggests that one of the reasons for non-referral could be the lack of awareness of such hypercalcemia, and consequently of PHPT, in many of these 66 cases. With regard to patient origin, most subjects were referred to the endocrinology clinic from Rheumatology and primary care, with a predominance of Rheumatology in group 2. This could be because rheumatologists monitored hypercalcemia until the patients met some criterion for referral. There were no differences among groups in terms of gender distribution or the incidence of adenomas.
Of the 43 patients in group 1, a total of 19 (44.2%) had normal calcemia values before the elevated calcemia value, versus 12 of the 23 patients in group 2 (52.2%), with a tendency toward a comparatively longer interval between the two measurements in group 2. This interval from the last previous normal calcemia value to the calcemia value resulting in patient referral was even longer in the 18 patients in group 3, with 44 months versus 22 months in group 1, though the difference did not reach statistical significance (p=0.07), possibly due to the small number of cases involved.
The 32 patients in group 4, together with the 16 patients in group 3, comprised a population with no evidence of hypercalcemia more than one year before referral took place. On comparing these two groups, the patients in group 4 were seen to be significantly older, with significantly higher calcium levels at the time of referral, and also with a tendency toward higher alkaline phosphatase concentrations. A similar percentage of patients in both groups (approximately 60%) met one or more of the four CFS considered at the time of referral to the endocrinology clinic. There were no differences in terms of gender distribution, renal function, the presence of lithiasis, or other CFS, though it must be noted that the number of patients involved was small.
All these data are summarized in Table 2.
Comparison of the biological and laboratory test parameters between the four patient groups. Age in years. Mean intervals in months.
| Group 1 | Group 2 | Group 3 | Group 4 | p | |
|---|---|---|---|---|---|
| Mean age at 1st elevated [Ca] (SD) | 52.7 (14) | 61.7 (8.7) | 54.1 (11.8) | 62.2 (12.6) | a,c,d,f |
| Mean age at 1st consultation (SD) | 57.4 (14.1) | 66.8 (7.6) | 54.2 (11.6) | 62.4 (12.5) | a,d,f |
| Mean age at surgery (SD) | 57.8 (14.2) | 68.8 (7.7) | 55.9 (12.4) | 63.9 (12.9) | a |
| Males (%) | 8 (18.6) | 4 (17.4) | 5 (27.8) | 10 (31.2) | – |
| Adenomas (%) | 37 (86) | 22 (95.7) | 17 (94.4) | 28/32 | – |
| Origin from PCP# (%) | 20 (46.5) | 5 (21.7) | 11 (61.1) | 15 (46.9) | d |
| Origin from Rheumatology# (%) | 8 (18.6) | 11 (47.8) | 3 (16.7) | 7 (21.9) | a,d |
| First elevated [Ca] (SD) | 11.10 (0.70) | 10.76 (0.24) | 10.89 (0.36) | 11.52 (0.84) | a,c,e,f |
| Mean [Ca] in mg/dl# (SD) | 11.43 (2) | 11.05 (0.64) | 10.84 (0.42) | 11.52 (0.83) | f,e |
| Alkaline phosphatase in IU/l# (SD) | 79.3 (42.3) | 70.5 (35.5) | 69.7 (35.7) | 95.7 (79.9) | – |
| Hyperphosphatemia# (%) | 10 (23.2) | 4 (17.4) | 3 (16.7) | 10 (31.2) | – |
| Interval 1st elevated [Ca] – 1st consultation (SD) | 56.7 (36.6) | 61.4 (43.8) | 2.3 (4.3) | 2.4 (2.4) | b,c,d,e |
| Interval 1st elevated [Ca] – 1st [PTH] (SD) | 49.8 (39.3) | 44.8 (43.7) | 0.1 (5.6) | 1.3 (1.9) | b,c,d,e |
| Interval 1st consultation – surgery (SD) | 10.2 (9.9) | 24.1 (25.8) | 26.9 (39.1) | 14.32 (26.5) | a |
| Interval normal [Ca] – 1st elevated## (DE) | 21.8 (23.5) | 35.0 (37.5) | 43.7 (43.5) | 4.1 | |
| Criteria for surgery### (%) | 43 (100) | 5 (21.7) | 12 (66.6) | 20 (62.5) | a,b,c,d,e |
| Age ≤50years# (%) | 22 (51.2) | 0 | 8 (44.4) | 5 (15.6) | a,d,f |
| Renal lithiasis# (%) | 22 (51.2) | 2 (8.6) | 7 (38.9) | 7 (21.9) | a,c,d,e |
| eGFR <60ml/min# (%) | 5 (11.6) | 0 | 0 | 0 |
Ca: calcium; SD: standard deviation; eGFR: estimated glomerular filtration rate; PCP: primary care physician.
Primary hyperparathyroidism has an estimated prevalence of 0.86% in the general population, according to a study conducted in almost three million individuals.10 However, the diagnosis of PHPT is often delayed, at least in part due to the failure to notice hypercalcemia in the laboratory tests.11,12 As a result, the patient is not referred in a timely fashion to specialized care for evaluation and treatment.
A delay in surgery to treat PHPT increases the risk of associated bone and renal morbidities, as shown by follow-up studies in nonsurgical patients,13 with bone mineral loss becoming evident at 8 years of follow-up and proving more severe after 10–15 years.14,15 By contrast, the reversal of PHPT affords very early benefits, as demonstrated by the bone remodeling biochemical parameters and densitometric findings.16 Early diagnosis and surgery in patients with PHPT also reduces the recurrence of nephrolithiasis,17 though the risk remains persistently higher than in the general population for up to 10 years after surgery.18,19 Such lithiasis associated with PHPT accounts for over 15% of all cases of end-stage renal failure secondary to nephrolithiasis, with an average delay between calculus formation and the start of dialysis of 86 months.20
This delay in diagnosis has been shown in series on the presence of unevaluated hypercalcemia.9–12 However, no studies have analyzed the incidence of such delay together with its possible causes and consequences in surgical patients. The present series found over half of the patients subjected to surgery for PHPT at a third level center to have evident hypercalcemia in laboratory tests performed more than one year before the operation, and almost two-thirds of them had criteria for surgery (CFS) when the basic parameters (age, lithiasis, renal function, and calcemia) were taken into consideration, but not bone mineral density (BMD) or calciuria. If these two parameters had been available, the percentage of patients with surgical indications at the time of the first episode of hypercalcemia might have been even greater. The delay in patient referral to the clinic despite the indication for surgery was approximately 5 years, and in 15% of these patients with overlooked hypercalcemia the delay exceeded 10 years. The presence of patients with renal failure in the group exhibiting inadequate delay (group 1), and the greater incidence of lithiasis at the time of referral to the clinic, demonstrate the pathogenic impact of such a delay at the renal level.
Patients without prior calcemia measurements recorded more than 12 months before referral (group 4) had significantly higher calcium levels at the time of referral (mean: 11.52mg/dl), suggesting that higher calcemia values increase the probability of direct patient referral to the endocrinology clinic. The severity of hypercalcemia as a preferential patient referral criterion is also supported by the observed progression of the concentrations in group 1, in which initial calcemia (mean: 11.1mg/dl) did not lead to referral, while referral was found to be indicated in the presence of higher calcemia values (mean: 11.43mg/dl). These data point to underestimation or a lack of knowledge of other established criteria for parathyroidectomy, apart from severe hypercalcemia, among the physicians that care for these patients, even without including osteoporosis or hypercalciuria. Recent studies have suggested the need for interventions to correct this problem.11,12
Because of the characteristics of our study, we were unable to assess the potential benefits of earlier patient intervention. Some, but not all, studies13 have revealed improvements in the patient neuropsychological parameters21 and quality of life after parathyroidectomy,22 and such improvement is particularly correlated to the previous hypercalcemia values,23 which were higher after delays in referral among the patients in group 1.
Occasionally, delays in patient referral to the specialist and subsequent surgical treatment may be due to advanced patient age, despite the proven efficacy and safety of the surgical approach, even in very elderly patients.24 In our series, this reason did not appear to justify the delay in the patients in group 1, since their mean age at the first measurement showing hypercalcemia was under 60 years, with only three exceeding 75 years, and none more than 80 years. In any case, elderly patients with PHPT have been shown to experience longer survival after fracture if they have undergone parathyroidectomy than if they have received nonsurgical management.25
The presence of incidental hypercalcemia in the emergency care tests constitutes the first indication of PHPT in 20% of the cases.26,27 In our series, almost half of the patients in group 1 (n=21; 48.8%) presented hypercalcemia in the laboratory tests made in the hospital emergency care setting. An active hypercalcemia detection policy in hospital laboratories has been shown to effectively increase early diagnosis and intervention in PHPT, at a reasonable economic cost.28 In group 1, emergency care, primary care, and Rheumatology (where the patients were evaluated for osteoporosis) were the areas which most frequently requested laboratory tests with hypercalcemia. Curiously, there were two cases where hypercalcemia appeared in tests requested by Endocrinology – both due to thyroid disease – in which the results were not taken into account. On analyzing the department that finally referred the patients to the endocrinology clinic, the proportion of cases originating from primary care was seen to be similar in group 1 and groups 2 and 3 considered jointly (approximately 40%), suggesting that the indication of surgical treatment was not the cause of referral to Endocrinology from primary care, but that management may have been conditioned to each individual physician and to the calcemia levels, as previously mentioned.
A source of bias in our study is the fact that it did not include all the patients evaluated for PHPT during the defined period of time: we only included patients subjected to surgery, and excluded those evaluated in the clinic during that period but not subjected to surgery due to failure to meet the CFS, patient rejection of surgery, or the decision not to indicate surgery for some other reason. In the group of patients not included in the study, the pattern of delayed referral to Endocrinology presumably remained the same, in agreement with the observations of the 23 patients of group 2, with regard to the date of the first laboratory test, in which the delay was not significantly different from that recorded in group 1 (61 versus 57 months). The non-inclusion of hypercalciuria and osteoporosis as criteria for surgical referral may have generated bias in lowering the number of patients included in group 1 in our study. Had these data been available in the retrospective evaluation of the patients in group 2, the percentage of individuals in group 1 would possibly have increased. Another limitation of the study is its retrospective nature and the limited number of patients involved, though the quality of the available data and the clarity of the study objectives appear to warrant the validity of the study.
In conclusion, the referral of patients with PHPT to Endocrinology is made late, with a mean delay of almost 5 years from the first measurement showing hypercalcemia, despite the presence of CFS in two-thirds of the cases. The most determinant factor for deciding referral appears to be the magnitude of hypercalcemia, without due consideration being given to the presence of other criteria indicating parathyroidectomy. This delay is associated with increased patient morbidity (at least at the renal level), and points to a need for awareness campaigns among physicians, particularly in the emergency and primary care settings, in order to ensure earlier identification among patients with PHPT.
AuthorshipMiguel Paja: study conception and design, and writing of the manuscript.
Adela L. Martínez: data collection and interpretation, design, and critical review of the article.
Andoni Monzón: data collection and interpretation, and critical review of the article.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to the patients for their collaboration in this publication.
Please cite this article as: Paja-Fano M, Martínez-Martínez A-L, Monzón-Mendiolea A. Retraso diagnóstico y terapéutico en el hiperparatiroidismo primario. Un problema no resuelto. Endocrinol Diabetes Nutr. 2020;67:357–363.





![Diagram of the patients evaluated in the study. CFS: criteria for surgery: age ≤50 years, [Ca] ≥11.4mg/dl, lithiasis or eGFR <60ml/min. Diagram of the patients evaluated in the study. CFS: criteria for surgery: age ≤50 years, [Ca] ≥11.4mg/dl, lithiasis or eGFR <60ml/min.](https://static.elsevier.es/multimedia/25300180/0000006700000006/v2_202009180803/S253001802030086X/v2_202009180803/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)

