In recent months the world has experienced the most complicated situation ever faced by most of us. The SARS-CoV-2 (COVID-19) pandemic has shaken the foundations of our society, and certainly of our healthcare system. We have needed to adapt in record time to both in- and out-hospital health organization systems very different from our usual services and units; we have learned medical treatments that were not in our texts; and we have had to live every day with the fear of not fighting this virus under the best conditions. In this context, Clinical Nutrition has also had to adapt to a new scenario. Our hospitals have multiplied the units for critically ill patients, and both these patients and many of those filling the hospital wards have needed nutritional medical treatment. An essential element in this regard is the coordinated participation of the members of nutrition units and other services, including physicians, nurses, dieticians-nutritionists and hospital pharmacists, who all play very relevant roles in this crisis.
COVID-19 has been characterized by very diverse clinical manifestations that are not fully understood yet. In addition to marked respiratory problems, the virus causes a disproportionate immune response in many individuals, with a massive inflammatory reaction. From the start of the pandemic, the most severely affected patients were seen to be elderly individuals and subjects with multiple disease conditions,1 which constitute typical malnutrition risk groups. Moreover, the virus causes a significant loss of appetite, accompanied by other symptoms such as anosmia, dysgeusia or diarrhea, all of which increase the risk of disease-related malnutrition (DRM). In addition, some of the drugs used in treatment can worsen these symptoms, as in the case of diarrhea.
For quite some time we have had clear scientific evidence of the importance of nutritional status in many disease conditions. In Spain, the PREDYCES study2 showed that DRM is very common in our hospitals, and moreover that it constitutes an indicator of a poor prognosis. We also know that adequate and early nutritional treatment is able to improve the prognosis of patients with multiple diseases during hospital admission. Recent data from the EFFORT trial3 have shown that adequate and early nutritional care is able to reduce both mortality by 35% (odds ratio [OR] 0.65 [0.47−0.91]; p = 0.011) and a poor clinical course - defined as admission to intensive care, hospital readmission, major complications, functional impairment or mortality - by 21% (OR 0.79 [95%CI: 0.64−0.97]; p = 0.023).
Therefore, although the situation we were facing was new and unknown, we considered that nutritional care should be adequate to help our patients fight the virus. The European Society for Clinical Nutrition and Metabolism (ESPEN) proposed that the prevention, diagnosis and treatment of DRM should be included in the routine management of COVID-19, and established 10 practical recommendations particularly referring to the critically ill and to patients with multiple disease conditions.4 The European Society of Endocrinology also recognizes the importance of malnutrition in its recommendations on COVID-19.5
In outpatients with active infection, the oral diet should be adapted to ensure nutritional enrichment capable of covering the energy, protein and other nutrient requirements in the lowest possible amounts of food, to be acceptable to patients with no appetite and with eating difficulties. At the start of the pandemic, and through its website, the Spanish Society of Endocrinology and Nutrition (Sociedad Española de Endocrinología y Nutrición [SEEN]) organized a specific information section on COVID-19 that included concrete recommendations for diet enrichment, as a priority concern for these patients at a high risk of DRM.6
With regard to patients requiring hospital admission, the known data from the epidemic in China7 led us to design an early nutritional strategy that was made known through the SEEN website.8 These patients are at high nutritional risk because of the increased requirements resulting from the severe acute inflammatory condition and the difficulty of satisfying these requirements due to hyporexia, dyspnea and feeding difficulties. Whenever possible, nutritional risk screening should be performed upon admission. The ESPEN recommendations suggest using MUST or NRS-2002.4 However, we should be aware that in many cases healthcare is being provided by non-routine staff with a considerable workload. Other proposals therefore suggest simplified versions that only record whether the patient has a body mass index (BMI) < 22 kg/m2, has lost weight in the last three months, or has a low food intake.9
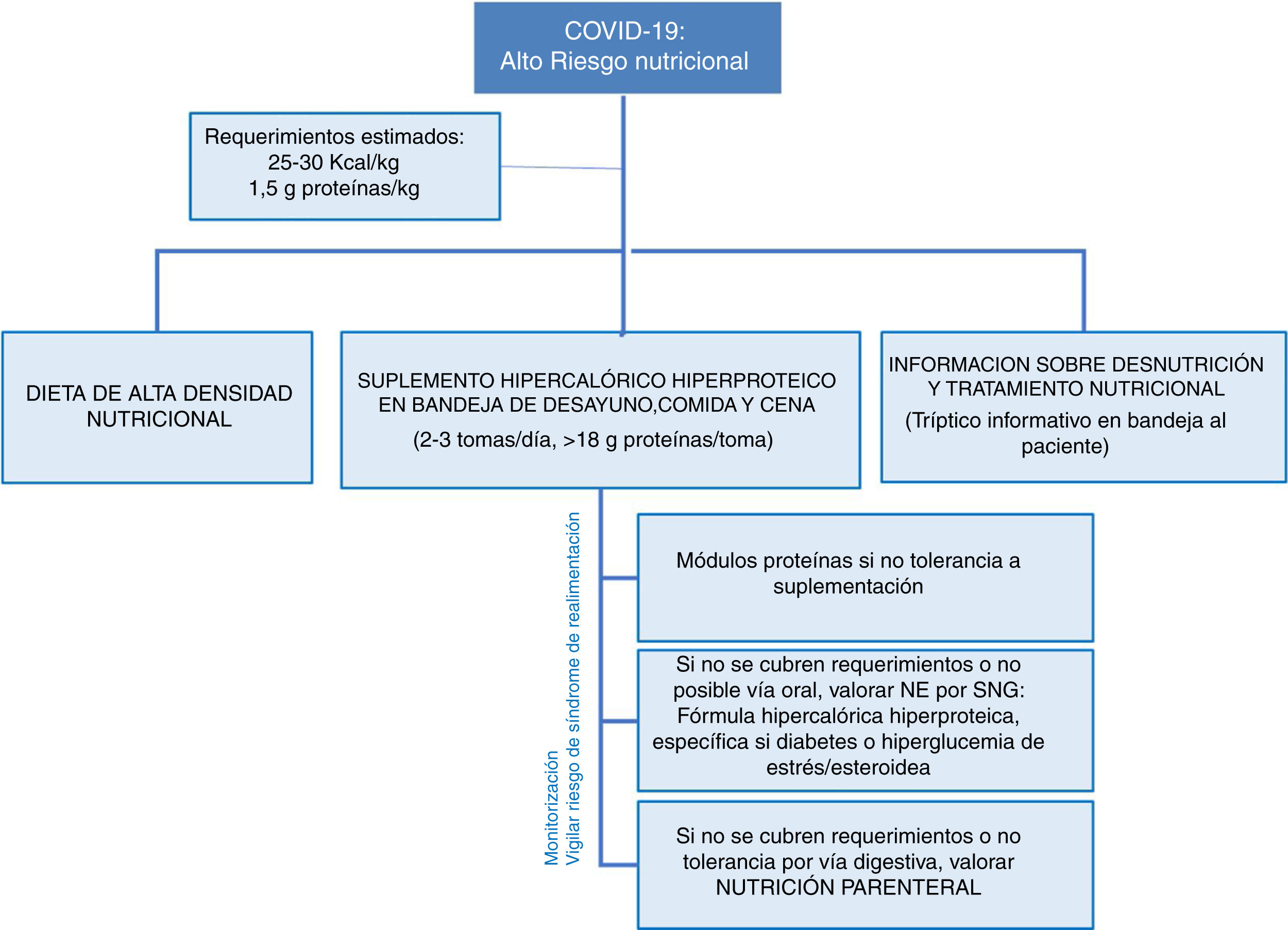
The estimated nutritional requirements are 25−30 kcal/kg body weight and 1.5 g protein/kg/day.7 To achieve this, a diet with a high nutritional density should be contemplated from the time of hospital admission, with due consideration of the difficulties involved in meeting the nutritional requirements due to the associated hyporexia. In this regard, we should consider hyperproteic-hypercaloric supplementing in 2–3 daily doses (adjusting as far as possible to the oral diet intake), supplying at least 18 g of protein per intake and an additional supply of 30 g of protein daily.4 We must take into account the isolation required by these patients. In this regard, we recommend including an informative leaflet on malnutrition and nutritional supplementation with the patient food tray to promote adherence and improve tolerance as far as possible. When tolerability to supplementing is low, we can consider adding protein modules and, of course, should contact the Nutrition Units to adapt treatment to specific conditions, particularly in patients with poorly controlled diabetes, dysphagia, kidney disease, etc.
Nutritional treatment is not static. Every 48−72 h we should assess compliance with the therapeutic objectives, and if these are not reached despite oral supplementing, the data from the EFFORT trial and the usual recommendations of the clinical guides referring to patients of this kind with multiple diseases10 underline the need for early enteral nutrition, either complementary to oral feeding or complete, and preferably using a hyperproteic-hypercaloric formula adjusted to the estimated requirements. The frequent presence of diabetes or hyperglycemia in these patients (either due to metabolic stress or in relation to corticosteroid therapy) may make it reasonable to use diabetes-specific hyperproteic formulas, which have shown clinical benefits11. The blood glucose levels should be monitored, with a target of 100−140 mg/dl.4
We need to be aware that the placement of nasogastric tubes is an aerosol-generating procedure; the use of complete personal protective equipment (PPE) is therefore essential. The British Association for Parenteral and Enteral Nutrition (BAPEN) has established practical safety recommendations for the administration of enteral nutrition12. We should remember that the need for prone decubitus to improve ventilation in some of these patients does not contraindicate enteral nutrition, though special monitoring of gastrointestinal tolerance is advisable. When enteral nutrition is not possible or the nutritional requirements are not met, for instance due to inadequate gastrointestinal tolerance, parenteral nutrition should be considered, though only after all other possible strategies have been tried.
Critical patients constitute a special subgroup. In this case, the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]) has also proposed an algorithm for the nutritional treatment of patients with COVID-1913, recommending a progressive increase in the calorie and protein targets: 20 kcal/kg and 1.2 g protein/kg on days 1–3 of Intensive Care Unit (ICU) admission, 25 kcal and 1.5 g/kg from day 4, and 30 kcal and 1.8 g/kg in the recovery phase. The American Society for Parenteral and Enteral Nutrition (ASPEN) and the Society of Critical Care Medicine (SCCM)14 have also established specific recommendations in this line, advising the slow and gradual start of enteral nutrition in the first 24−36 h of admission to the ICU.
The risk of refeeding syndrome should always be considered in patients with previous malnutrition. Accordingly, phosphorus, potassium and magnesium levels should be monitored, and thiamine 100 mg/8 h should be supplemented in patients with previous weight loss > 10% or previous inadequate food intake for more than 5 days. Fig. 1 summarizes the nutrition approach strategy in these patients.
In nutritional treatment, it is important to prevent and treat micronutrient deficiencies, but there is currently not enough evidence to support the empirical use of supraphysiological or supratherapeutic doses of micronutrients to improve the clinical course of COVID-19.4
After the acute phase has been passed, and especially in patients who have required intensive care or who have developed a severe form of the disease, we should pay attention to nutritional and muscle recovery. We know the loss of muscle mass to be associated with a poor prognosis, and so due care is required in the recovery phase. In addition to adequate rehabilitation, the nutritional status of the patient should continue to be monitored, with the use of nutritional supplementation, if necessary. Supplements enriched with leucine or beta-hydroxymethylbutyrate (HMB)15 could play a beneficial role in such recovery. Data from the NOURISH trial16 support the use of hyperprotein supplements with HMB during hospital admission and up to 90 days later, in elderly patients with cardiorespiratory disease, with a demonstrated 51% decrease in mortality (relative risk [RR] versus placebo 0.49; p = 0.018). The ESPEN recommendations advocate the maintenance of nutritional supplementation for at least one month.4 In this recovery phase, it is also important to pay attention to possible dysphagia, particularly in patients who have required prolonged orotracheal intubation, have suffered a significant loss of muscle mass, or who have previous predisposing conditions. And of course, we will need to begin to define how we are going to conduct outpatient nutritional monitoring in these patients, because this situation - which has appeared without prior notice - is causing us to redefine our clinics, and in the case of Clinical Nutrition it represents another challenge we will need to face in the very near future.
We should not forget the negative impact of disorders such as obesity upon the prognosis of COVID-19. The ESPEN recommendations already speak of a "double burden of malnutrition", since both obesity and malnutrition are associated with a greater severity of the disease. Therefore, the start of nutritional treatment should not be delayed on the grounds that the patient is overweight.
Considering the importance of healthy living habits, particularly in relation to lockdown during the pandemic, the SEEN has also established recommendations for a balanced diet17 and exercise18 to help palliate the effects which inadequate eating during lockdown may have upon future health. Knowing that obesity is another pandemic with important health consequences, its coexistence with the COVID-19 pandemic requires us to further improve our strategies at both the healthcare and population levels. This is one of our most relevant and urgent current challenges.
In conclusion, COVID-19 has represented a social and health challenge, and also a challenge in terms of clinical nutrition, both because of the number of patients requiring nutritional medical treatment and due to the management difficulties related to the important inflammatory situation and the characteristics of these patients, who are often elderly, with multiple diseases and obese. The adaptation of the guidelines of the main scientific bodies is a help in this new context in which solid scientific evidence still needs to be obtained.
Please cite this article as: Ballesteros Pomar MD, Bretón Lesmes I. Nutrición Clínica en tiempos de COVID-19. Endocrinol Diabetes Nutr. 2020. https://doi.org/10.1016/j.endinu.2020.05.001