The aim of this study was to analyze the relationship between HDL-cholesterol and the risk of SARS-CoV-2 infection in over 75-year-olds residing in the Community of Madrid.
MethodsStudy of a population-based cohort, composed of all residents in Madrid (Spain) born before January 1, 1945 and alive on December 31, 2019. Demographic, clinical and analytical data were obtained from primary care electronic medical records from January 2015. Confirmed SARS-CoV-2 infection was defined as a positive RT-PCR or antigen test result. Infection data correspond to the period March 1, 2020 through December 31, 2020.
ResultsOf the 593,342 cohort participants, 501,813 had at least one HDL-cholesterol determination in the past 5 years. Their mean age was 83.4 ± 5.6 years and 62.4% were women. A total of 36,996 (7.4%) had a confirmed SARS-CoV2 infection during 2020. The risk of infection [odds ratio (95% confidence interval)] for SARS-CoV2 according to increasing quintiles of HDL-cholesterol was 1, 0,960 (0,915–1,007), 0,891 (0,848–0,935), 0,865 (0,824–0,909) y 0,833 (0.792–0,876), after adjusting for age, sex, cardiovascular risk factors and comorbidities.
ConclusionsThere is an inverse and dose-dependent relationship between HDL-cholesterol concentration and the risk of SARS-CoV2 infection in subjects aged over 75 years of age in the Community of Madrid.
El objetivo de este estudio fue analizar la relación entre el colesterol-HDL y el riesgo de infección por SARS-CoV-2 en mayores de 75 años residentes en la Comunidad de Madrid.
MétodosEstudio de una cohorte de base poblacional, compuesto por todos los residentes en Madrid (España) nacidos antes del 1 de enero de 1945 y vivos el 31 de diciembre de 2019. Los datos demográficos, clínicos y analíticos se obtuvieron de las historias clínicas electrónicas de atención primaria desde enero de 2015. La infección confirmada por SARS-CoV-2 se definió como un resultado positivo en la RT-PCR o en la prueba de antígeno. Los datos sobre infección por SARS-CoV-2 corresponden al periodo del 1 de marzo de 2020 hasta el 31 de diciembre de 2020.
ResultadosDe los 593.342 participantes de la cohorte, 501.813 tenían al menos una determinación de colesterol-HDL en los últimos 5 años. Su edad media era 83,4 ± 5,6 años y el 62,4% eran mujeres. Un total de 36.996 (7,4%) tuvieron una infección confirmada por SARS-CoV2 durante el año 2020. El riesgo de infección [odds ratio (intervalo de confianza 95%)] por SARS-CoV2 según los quintiles crecientes de colesterol-HDL fue de 1, 0,960 (0,915–1,007), 0,891 (0,848–0,935), 0,865 (0,824–0,909) y 0,833 (0.792–0,876), tras ajustar por edad, sexo, factores de riesgo cardiovascular y comorbilidades.
ConclusionesExiste una relación inversa y dosis-dependiente entre la concentración de colesterol-HDL y el riesgo de infección por SARS-CoV2 en los mayores de 75 años de la Comunidad de Madrid.
Since the appearance of the first case of infection by the SARS-CoV2 virus in Wuhan (China) at the end of 2019 (COVID-19),1 the disease has spread throughout the world, with almost 200 million cases up to August 2021.2 Somewhat more than 80% of those infected suffer a mild or asymptomatic infection and do not require hospitalization.3
Several factors have been associated with increased risk of infection. These include being male, older, obesity, arterial hypertension, diabetes or smoking.4 The possibility that the concentration of HDL-cholesterol may modify the risk of infection by SARS-CoV2 has also been raised.
HDL particles are lipoproteins with a heterogeneous composition, size and density. Their main function is to transport cholesterol from tissues to the liver so that it can eventually be eliminated in the bile. HDL particles also regulate the inflammatory response, and they have antithrombotic and antioxidant effects as well as antiapoptotic properties.5 Several authors have shown that HDL may modulate innate and adaptive immunity, modifying the inflammatory response and the activation of B and T6 lymphocytes. HDL also influence humoral immunity by modulating complementary system activation and pentraxin 3 expression. HDL also control the inflammatory response by regulating the proinflammatory expression of cytokines induced by toll-like receptors.6
Some observational studies have described an association between low concentrations of HDL-cholesterol and a higher risk of nosocomial infection in hospitalized patients.7,8 A Danish cohort study reported that low or very high levels of HDL-cholesterol are associated with an increased risk of hospitalization due to infection.9 Additionally, Mendelian randomization studies show an inverse relationship between genetically determined levels of HDL-cholesterol and the risk of hospitalization due to an infectious disease.10
Respecting COVID-19, several studies have described how low levels of HDL-cholesterol were associated with a higher risk of hospitalization, more severe disease and an increased risk of death.11,12 Nevertheless, few studies have associated with concentration of HDL-cholesterol with the risk of infection by SARS-CoV2, independently of the severity or evolution of the same13 and especially in the elderly, who are the most susceptible population and the one with the worst prognosis.
The aim of this study was to analyse the relationship between HDL-cholesterol concentration and the risk of infection by SARS-COV2 in individuals over the age of 75 years who live in the Community of Madrid, and to study whether this relationship remained after adjusting for factors associated with HDL-cholesterol concentration and SARS-COV-2 infection.
Material and methodsStudy designAn observational study of a population base cohort established on 1 January 2015 consisting entirely of inhabitants of the Community of Madrid (Spain) who were born before 1 January 1945. The Community of Madrid offers free medical care to 100% of the population. Its primary care system consists of 3881 family doctors who work in 424 health centres. All of the inhabitants of the region have an electronic clinical history in primary care (AP-Madrid database). On 31 December 2019 this contained information on 6,466,966 living individuals, of whom 593,342 were born before January 1945 and had at least one data entry during the previous 2 years.
Study variablesThe available data for all of the participants included their age, sex, cardiovascular risk factors and comorbidities until 31 December 2019, as obtained from the AP-Madrid database. Morbidities were registered according to the International Classification of Primary Care (ICPC-2). The existence of any previous cardiovascular disease was specifically recorded (myocardial infarct, angina, ictus or peripheral artery pathology), any active cancer during the 5 previous years (except for non-melanoma skin cancer), and the presence of arterial hypertension, diabetes, chronic kidney failure, congestive heart failure, chronic obstructive pulmonary disease, auricular fibrillation and dementia. Information was also collected from AP-Madrid on alcohol and tobacco consumption. Data were gathered on infection, hospitalization or death due to SARS-CoV-2, from 1 March 2020, when the pandemic started in Spain, until 31 December 2020.
All of the blood analyses and anthropometric measurements performed from 1 January 2015 to 31 December 2019 were available for this study. The average of all of the samples analysed during this period was used for each continuous variable. HDL-cholesterol quintiles were calculated separately for men and women.
SARS-CoV-2 infection was considered to have been confirmed when the patient had a positive antigen test or a positive RT-PCR (real time polymerase chain reaction). The results were obtained from AP-Madrid and were supplied by the Public Health Office, Madrid.
The quality of primary care electronic clinical histories has already been validated for research purposes,14 and the database has been widely used to study the epidemiology of cardiovascular risk factors in elderly patients.15
Statistical analysisQuantitative variables are shown as a mean ± standard deviation, and categorical variables are shown according to prevalence, calculated using the coefficient between the number of patients with each diagnosis and the total number of patients. A Kolmogorov–Smirnov test was used to check the normal distribution of the variables. Comparisons between continuous variables were undertaken using ANOVA and categorical variables were compared using the chi-squared test.
Logistic regression analysis was used to identify the variables that were independently associated with SARS-CoV2 infection, obtaining the odds ratios and their confidence interval at 95%. The variables included in the final model were those which univariate analysis showed had a level of significance of less than 10% (P < .10) and those which were considered to be opportune because of their potential role as confusion variables. Statistical analyses were carried out using the SPSS 19.0 statistical package (IBM Corp, Armonk, New York, U.S.A.).
This study was approved by the Ethics and Medicine Research Committee (CEIm) of Ramón y Cajal Hospital (Madrid).
ResultsOf the 593,342 participants in the cohort, 501,813 had at least one determination of HDL-cholesterol in the previous 5 years. Their average age was 83.4 ± 5.6 years, and 62.4% were women. The average level of HDL-cholesterol in the men was 49.8 ± 12.1 mg/dl, and in the women it was 58.9 ± 14.2 mg/dl. A total of 36,996 (7.4%) participants had had a confirmed SARS-CoV2 infection during the year 2020, with an accumulated incidence of 6.9% in the women and 8.2% in the men. Table 1 shows the clinical and biological characteristics of the total population, and the populations of infected and uninfected individuals. The infected patients were older, with a higher proportion of men, a reduced proportion of dyslipidaemia and increased diabetes mellitus, auricular fibrillation, heart failure, cardiovascular disease, chronic obstructive pulmonary disease, cancer and Alzheimer’s disease in comparison with the uninfected participants. The infected participants also had a higher body mass index. Respecting the lipid profile, the infected participants lower concentrations of total cholesterol and LDL- and HDL-cholesterol, although they had higher levels of triglycerides than the uninfected participants. In terms of their state of nutrition, the infected participants had lower concentrations of haemoglobin, albumin and fewer lymphocytes.
Clinical–biological characteristics of the total population analysed, divided into infected and uninfected individuals.
| Variable | Total | Not infected | Infected | P |
|---|---|---|---|---|
| n = 501,813 | n = 464,817 | n = 36,996 | ||
| Age (years) | 83.4 ± 5.6 | 83.3 ± 5.6 | 84.6 ± 5.9 | <.001 |
| Women (%) | 62.4 | 62.7 | 58.2 | <.001 |
| Arterial hypertension (%) | 65.0 | 65.0 | 65.3 | .198 |
| Dyslipidaemia (%) | 57.1 | 57.5 | 55.4 | <.001 |
| Diabetes (%) | 25.9 | 25.6 | 29.2 | <.001 |
| Auricular fibrillation (%) | 15.6 | 15.3 | 18.9 | <.001 |
| Heart failure (%) | 6.5 | 6.3 | 9.3 | <.001 |
| Cardiovascular disease (%) | 17.9 | 17.6 | 21.8 | <.001 |
| Ischemic cardiac pathology (%) | 9.2 | 9.1 | 11.0 | <.001 |
| Ictus (%) | 6.2 | 6.8 | 8.1 | <.001 |
| Peripheral arterial disease (%) | 4.6 | 4.5 | 5.9 | <.001 |
| Chronic obstructive pulmonary disease (%) | 10.9 | 10.7 | 13.5 | <.001 |
| Cancer (%) | 5.2 | 5.2 | 5.7 | <.001 |
| Chronic kidney failure (%) | 6.7 | 6.6 | 7.9 | <.001 |
| Alzheimer’s disease (%) | 8.3 | 7.9 | 13.8 | <.001 |
| Alcohol consumption (%) | 1.2 | 1.2 | 1.4 | <.001 |
| Tobacco consumption (%) | 5.1 | 4.2 | 5.9 | <.001 |
| Body mass index (kg/m2) | 28.2 ± 4.5 | 28.2 ± 4.5 | 28.5 ± 4.7 | <.001 |
| Total cholesterol (mg/dL) | 184 ± 33 | 184 ± 33 | 178 ± 33 | <.001 |
| LDL-cholesterol (mg/dL) | 106 ± 27 | 106 ± 27 | 102 ± 28 | <.001 |
| HDL-cholesterol (mg/dL) | 55.4 ± 14.2 | 55.6 ± 14.2 | 53.0 ± 13.8 | <.001 |
| Triglycerides (mg/dL) | 116 ± 48 | 116 ± 48 | 118 ± 50 | <.001 |
| Albumin (g/dL) | 4.1 ± 0.3 | 4.1 ± 0.3 | 3.9 ± 0.4 | <.001 |
| Haemoglobin (g/dL) | 13.8 ± 1.4 | 13.9 ± 1.4 | 13.6 ± 1.4 | <.001 |
| Lymphocytes (×103/mm3) | 2.5 ± 2.8 | 2.6 ± 3.3 | 2.5 ± 3.3 | <.001 |
When the relationship between SARS-CoV-2 infection and HDL-cholesterol concentration was studied in the multivariate analysis, adjusting for cardiovascular risk factors and comorbidities, the odds ratio was 0.991 (confidence interval at 95%, 0.990−0.992) for every mg/dL of HDL-cholesterol, P < .001. There was therefore an inverse relationship between HDL-cholesterol and the risk of infection. This level of statistical significance did not change after adjusting for malnutrition indicators such as albumin, haemoglobin or lymphocytes.
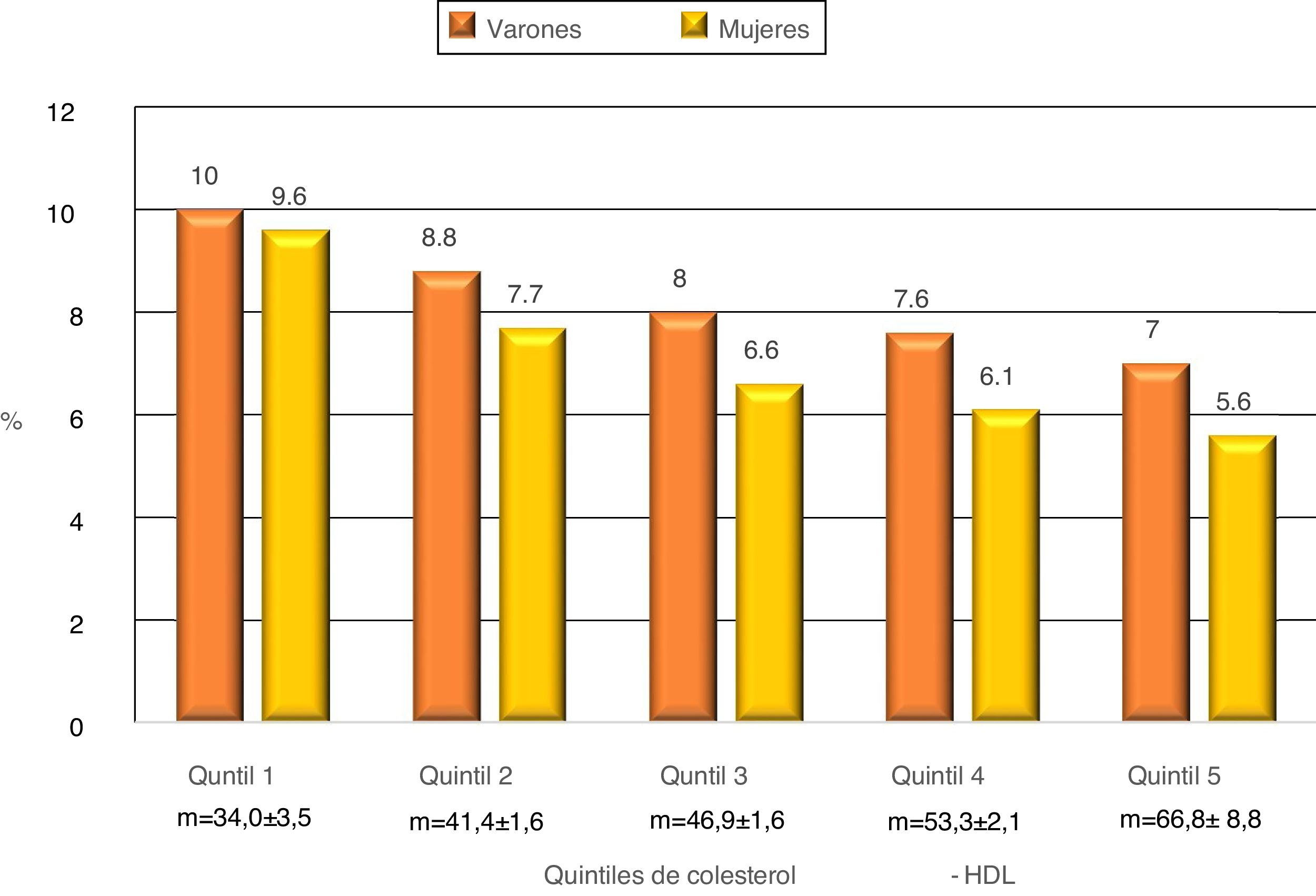
Fig. 1 shows the accumulated incidence of SARS-CoV-2 infection according to the HDL-cholesterol quintiles. When the population is divided into quintiles according to HDL-cholesterol, separately for men and women, and taking the first quintile as the reference, there was a gradual and significant dose-dependent fall in the risk of infection with each quintile. This was so after adjustment only for age and sex (model 1), as well as after adjustment for all of the co-variables (model 2) (Table 2).
Risk of infection by SARS-CoV-2 in individuals over the age of 75 years according to HDL-cholesterol quintiles, adjusted for age and sex (model 1) and for all of the co-variables (model 2).
| HDL-cholesterol | Model 1 | P | Model 2 | P | |
|---|---|---|---|---|---|
| m ± SD (mg/dL) | OR (CI95%)a | OR (CI95%)b | |||
| Q1 | 34 ± 3.5 | 1 | 1 | ||
| Q2 | 41.4 ± 1.6 | .881 (.836−.928) | <.001 | .960 (.915−1.007) | .092 |
| Q3 | 46.9 ± 1.6 | .799 (.758−.842) | <.001 | .891 (.848−.935) | <.001 |
| Q4 | 53.3 ± 2.1 | .755 (.716−.795) | <.001 | .865 (.824−.909) | <.001 |
| Q5 | 66.8 ± 8.8 | .692 (.657−.729) | <.001 | .833 (.792−.876) | <.001 |
CI: confidence interval; m ± SD: mean ± standard deviation; OR: odds ratio.
**Adjusted for age, sex, heart failure, auricular fibrillation, dyslipidaemia, diabetes, chronic kidney failure, alcohol consumption, tobacco consumption, chronic obstructive pulmonary disease, cardiovascular disease, dementia, body mass index, haemoglobin, albumin and leukocytes.
In the population aged over 75 years in the Community of Madrid, HDL-cholesterol levels are inversely associated with the risk of infection by SARS-CoV-2, so that the risk of infection decreases as levels rise. Other factors have been described that are also associated with low levels of HDL-cholesterol, such as obesity or diabetes. These too are risk factors for infection, and they may be the cause of the said finding. In our study, after adjusting for these factors and other co-factors that are also associated with a higher risk of infection, the statistical significance of the inverse relationship between HDL-cholesterol and infection by SARS-CoV-2 remained the same.
The higher incidence of infections in subjects with low HDL-cholesterol is well-known, not only in those who are hospitalized7,8 but also in cohort studies.9,10 At least 2 studies using Mendelian randomization have described the association between a low level of HDL-cholesterol and a higher risk of hospitalization due to a bacterial or viral infection. In the cohort of the general population of Copenhagen using 2 common variants of genes that regulate the concentration of HDL-cholesterol, hepatic lipase and cholesterol ester transporter protein,9 and in the UK Biobank using a multi-gene score for genes that regulate the concentration of HDL-cholesterol.10 Genetically determined low levels of HDL-cholesterol are therefore associated with a higher risk of hospitalization due to an infectious disease, indicating that this may be a causal relationship.
Several authors have described the inverse association of HDL-cholesterol at admission to hospital with increased severity of COVID-19, a higher risk of admission to an ICU and higher mortality.11,12 However, this association has also been described when the concentration of HDL-cholesterol prior to infection was used.16,17 In a study of cases and controls in which half of the cases were outpatients, a high level of HDL-cholesterol determined years previously was associated with a lower risk of a positive PCR for SARS-CoV2.13 Nevertheless, when in this population a Mendelian randomization study was performed using a genetic risk score based on polymorphisms associated with HDL-cholesterol levels, no association was found between increased HDL-cholesterol levels and a low risk of infection by SARS-CoV2, even after adjustment for body mass index and diabetes.13 This disparity with large cohort Mendelian randomization studies which found a relationship with a low risk of infection may be due to the relatively small number of individuals in this study, compared with the previous ones.9,10
Several studies have shown that HDL may modulate innate and adaptive immunity, increasing the resistance against infections.18 HDL neutralize and clear proinflammatory toxins, especially the polysaccharide of the membrane of gram-negative bacteria, as well as promoting their clearance by their binding to the SR-B1 receptor.19 HDL control the inflammatory response by regulating the expression of proinflammatory cytokines induced by the Toll-like receptor through the transcriptional regulator which activates the transcription-3 factor.20 However, HDL also have properties that may increase resistance against viral infections.21 More specifically, respecting SARS-CoV2, high concentrations of HDL are associated with faster clearance of the virus.22 In vitro studies have shown how native HDL play an important role against the virus without increasing cytotoxicity, although glycated HDL lose this activity, and they may be the cause of the poorer prognosis in diabetic patients.23
The limitations of this study would include the fact that during the first months of the pandemic there was a great shortage of diagnostic tests for SARS-CoV2, so that many patients with symptoms or asymptomatic contacts could not be diagnosed with the infection, so that the number of infected individuals was under-estimated. There would also have been a selection bias, given that the few diagnostic tests performed during the first months of the pandemic took place mainly in the hospitals used by the most severe cases, or patients with multiple risk factors for suffering the disease, especially elderly people. Thus, somewhat more than 50% of our infected patients required hospitalization, and approximately half of them died. The main strengths of this study are the inclusion of all of the inhabitants of Madrid over the age of 75 years who had at least one determination of HDL-cholesterol, the reliability of its data and the consistency of its results, even after adjustment for multiple co-variables.
To conclude, HDL-cholesterol levels measured prior to the pandemic are associated in a dose-dependent way with lower risk of infection by SARS-CoV2, in inhabitants of Madrid over the age of 75 years. These data show that HDL-cholesterol plays a protective role against infections.
FinancingThis paper was partially financed by a SEA grant for clinical-epidemiological research in the year 2020.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Lahoz C, Salinero-Fort MA, Cárdenas J, Rodríguez-Artalejo F, Díaz-Almiron M, Vich-Pérez P, et al. Concentración de colesterol-HDL y riesgo de infección por SARS-CoV-2 en personas mayores de 75 años: una cohorte con medio millón de participantes de la Comunidad de Madrid. Clin Investig Arterioscl. 2022;34:113–119.