We have read with great interest the paper by Pérez et al.1 about gastric perforation in an adult due to a trichobezoar (Rapunzel syndrome). The fact is that we have recently had the opportunity to treat a similar case, and the exceptional nature of the case (as commented by the authors) has encouraged us to publish our experience.
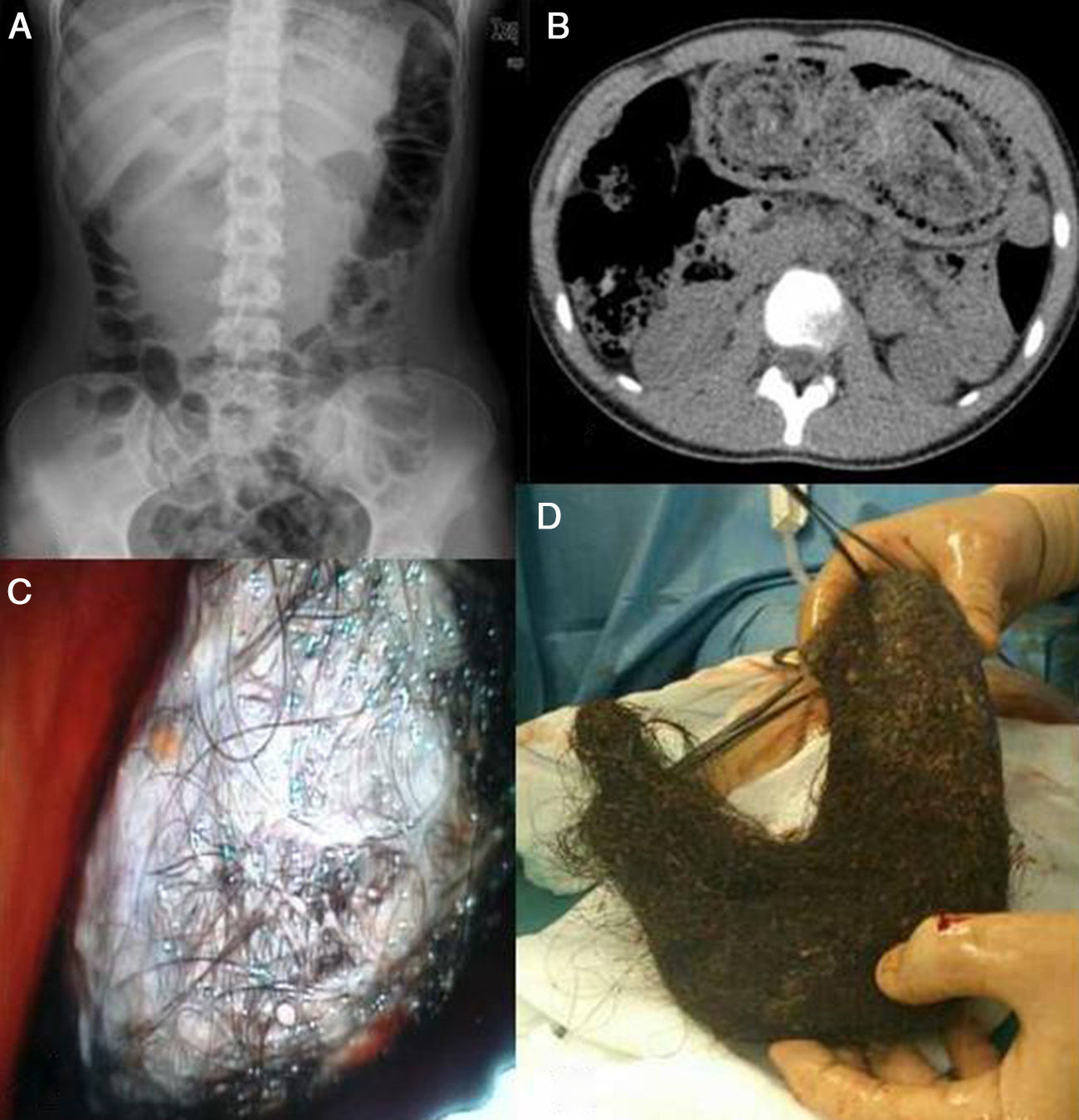
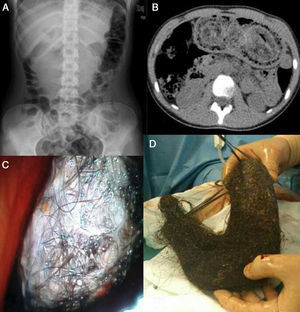
The patient was a 13-year-old girl who was being studied due to chronic iron-deficiency anemia and alopecia. She reported intermittent abdominal pain, early satiety and nausea with sporadic vomiting. Upon examination, we found evidence of a large tumor formation that protruded from the epigastrium under the costal edge that was non-painful and well-outlined, and which the patient said to have noticed about a year before. Abdominal radiograph (Fig. 1A) showed that the intestinal loops had been displaced to the lower hemiabdomen, along with an opaque epigastric image. Abdominal CT (Fig. 1B) demonstrated evidence of a large gastric bezoar, but the patient denied having trichotillomania and trichophagia. We decided to study the mass endoscopically (Fig. 1C) to reach a definitive diagnosis and attempt therapy, which was unsuccessful due to the large size and consistency of the mass. In the end, the gastric trichobezoar was removed surgically (20×8cm) by means of vertical gastrostomy (Fig. 1D).
(A) Radiographic image with mixed density located in the epigastrium. (B) CT showing the stomach totally occupied by a heterogenous mass. (C) Endoscopic image of the trichobezoar. (D) Compact trichobezoar removed by gastrostomy (made up of hair, mucus and decomposing food) that had occupied the entire stomach.
Bezoars are accumulations of undigested material in the lumen of any segment of the gastrointestinal tract, frequently the stomach.1–4 They can remain asymptomatic for long periods or cause symptoms such as early satiety, halitosis, iron-deficiency anemia, weight loss, abdominal discomfort and obstructive symptoms.
Trichobezoars are bezoars made up of hair that may descend from the stomach toward the small bowel and even reach the transverse colon, known as Rapunzel syndrome.1 It is caused by trichotillomania (compulsive urge to pull out one's own hair), associated with trichophagia (compulsive eating of hair, not necessarily one's own) in less than 50% of cases. It is estimated that one out of every 2000 children have trichotillomania and 5%–20% trichophagia, but few present with trichobezoars.5 90% of cases are seen in females, with a maximum incidence in the 9–13-year-old age range. Most patients present some type of neuropsychiatric disorder.1,6
Palpation of the abdomen and patient interviews may be of great help in making a diagnosis, even though it is not common for patients to openly admit this habit. Imaging tests can confirm this suspicion and abdominal CT is the technique of choice4 although only upper gastrointestinal endoscopy is able to determine its composition and can be used for treatment.5,7
There are 3 treatment modalities for bezoars, which depend on their type, size and location: chemical or enzymatic dissolution, endoscopic extraction or surgical removal.4–7 The treatment of choice in the largest and most compact forms is surgery, preferably laparoscopic,7 accompanied by psychiatric treatment of the underlying disease and follow-up to reduce the frequency of recurrences.8
Please cite this article as: Fernández-López A-J, González-Valverde FM, Rodenas-Moncada J, Albarracín Marín-Blazquez A. Tricofagia y tricobezoar. Cir Esp. 2014;92(6):448–449.