Hemocholecyst is a term introduced in 1961 that defines gallbladder hemorrhage.1 It is a rare pathology that has been associated with several disease processes, such as gallbladder neoplasia, cholecystitis,2 aneurysm of the cystic artery, hemobilia, trauma, coagulation disorders including renal failure, cirrhosis of the liver and anticoagulant treatment.3 We present a new case of hemocholecyst in a patient who had been preoperatively diagnosed and safely treated by laparoscopic cholecystectomy. We also analyze different diagnostic and therapeutic aspects of interest.
The patient is a 39-year-old male with a medical history that included consuming more than 150g of ethanol/day, hypertriglyceridemia, chronic ethyl-toxic hepatopathy and implantation in December 2009 of a metallic aortic prosthesis due to aortic failure, with anticoagulation therapy since then with acenocoumarol. He came to the Emergency Department due to symptoms that had been developing over the previous 3h after trauma that included “dark-colored vomit and dizziness”; he also reported having “dark-colored feces”. On physical examination, the patient was hemodynamically stable. Mild jaundice of the skin and mucus membranes was observed, as well as abdominal pain and abdominal wall hematomas located in the left flank. A mass was also detected in the right hypochondrium, with no guarding or rebound tenderness. The rectal exam demonstrated dark, bloody feces. Laboratory analysis showed: leukocytosis 18,500; 91.1% neutrophils; Hb 9.82; platelets 209,000; prothrombin rate 65.8%; urea 116; GOT 127; GPT 108; GGT 1.229; FA 786 and BT 2.7.
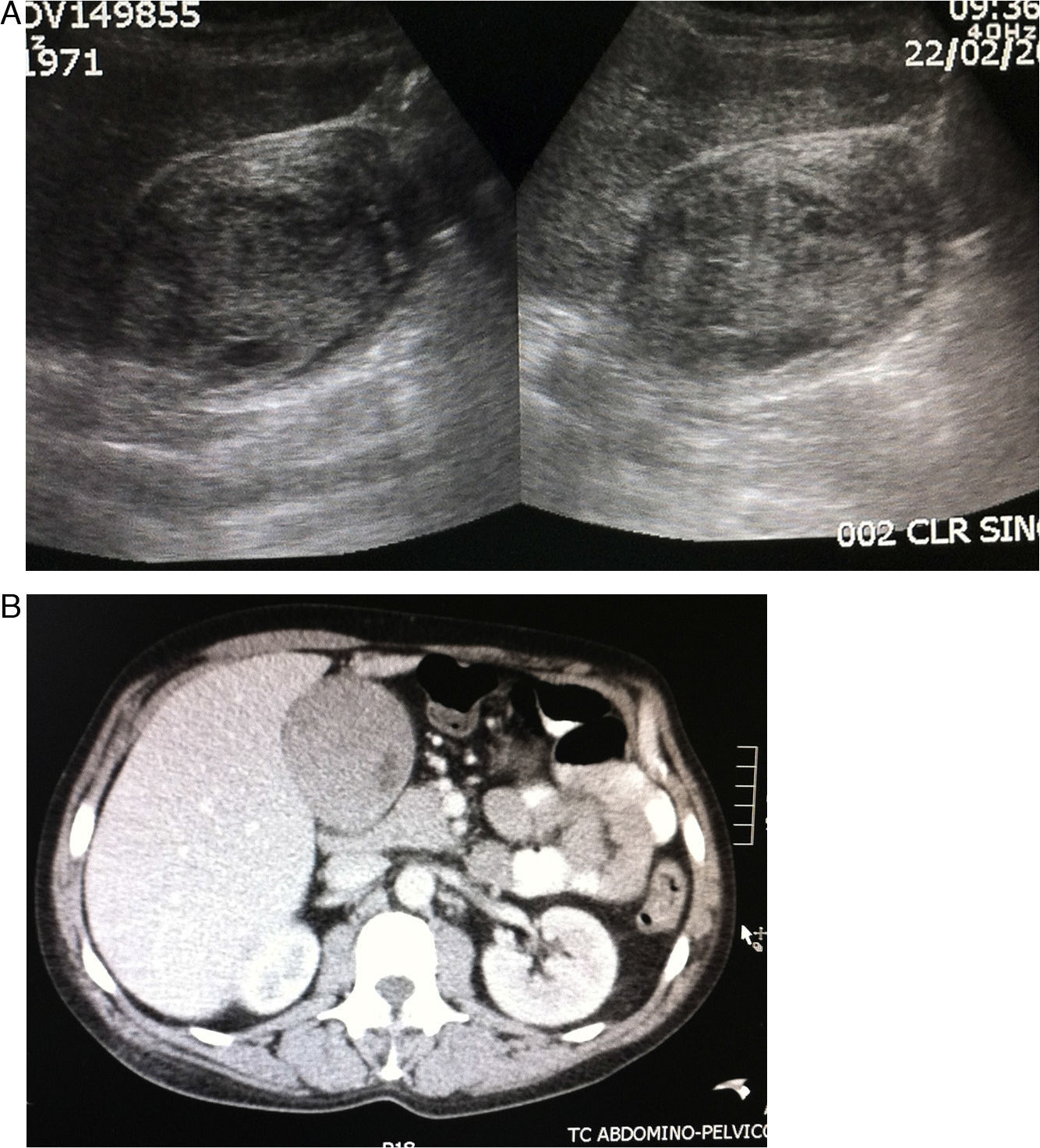
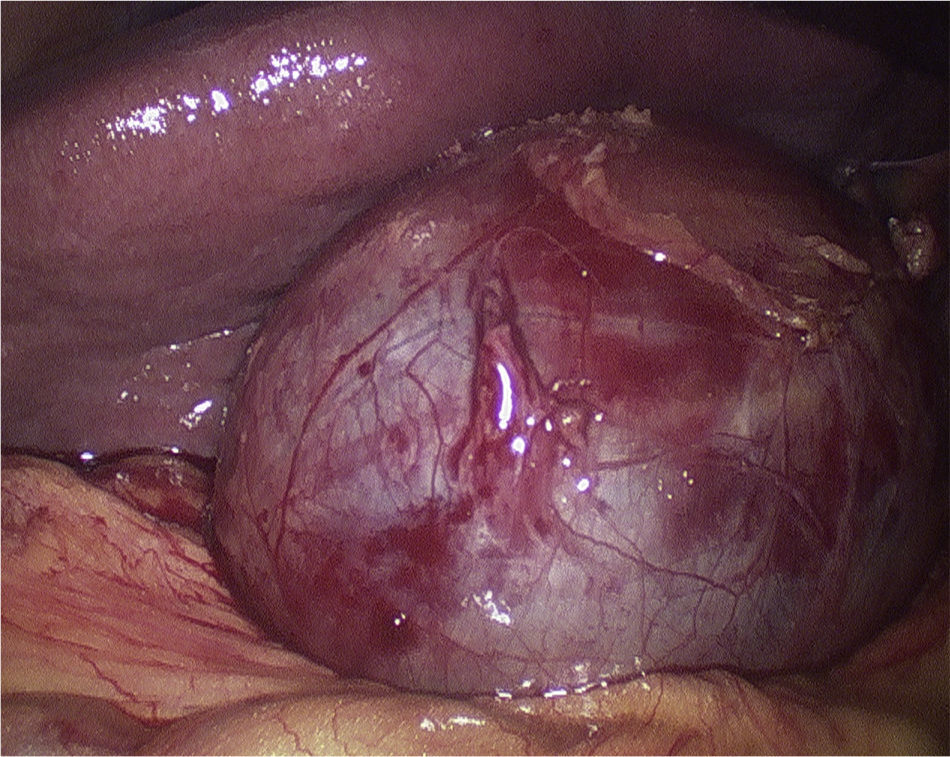
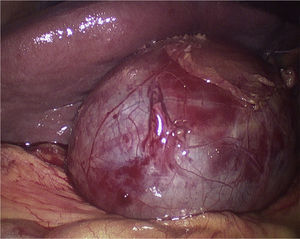
Gastroscopy diagnosed esophagitis, cardial incompetence and duodenitis, with no signs of bleeding during the examination. Abdominal ultrasound revealed a distended gallbladder with solid heterogeneous content, which ruled out hematoma in the gallbladder (Fig. 1A). Computed tomography (CT) demonstrated collateral circulation and distended gallbladder with abundant heterogeneous content in its interior, probably related with internal gallbladder bleeding, with no dilation of the bile duct (Fig. 1B). The patient then underwent laparoscopy, which revealed a hemocholecyst (Fig. 2), and laparoscopic cholecystectomy was performed with no complications. The patient was discharged on the seventh day after the analytical parameters had improved. The pathology study reported that the mucus membrane of the gallbladder wall had extensive ulcers and bloody material on its surface.
Since 1948, when Sandblom4 published the cases of 9 patients with post-traumatic hemobilia, there have been few manuscripts about hemocholecyst published in the literature. In clinical practice, it can be difficult to differentiate between hemocholecyst and hemobilia; moreover, hemocholecyst may cause hemobilia, or vice versa.1
Gallbladder trauma is a rare entity (particularly when it is not associated with other lesions) that represents only 0.5–0.6% of intra-abdominal trauma. Factors that predispose patients toward these gallbladder lesions include a thin gallbladder wall, postprandial distension and alcohol consumption.5 In our patient, there were several possible causes leading to the pathology: treatment with anticoagulants, cirrhosis of the liver and previous trauma. Hemocholecyst is a rare cause of abdominal pain, and its characteristic clinical findings include abdominal pain in the right hypochondrium, fever and leukocytosis in addition to symptoms indicating gastrointestinal hemorrhage due to hemobilia, such as melenas or hematemesis after the blood drains from the gallbladder into the gastrointestinal tract.6 Furthermore, it can exceptionally cause obstruction of the main bile duct, inducing cholangitis.3
The diagnosis of hemocholecyst can be difficult and evaluation with imaging tests plays a crucial role. Ultrasound findings include gallbladder wall thickening and non-mobile intraluminal echogenic material,7 which is difficult to distinguish from gallbladder neoplasm or gangrenous cholecystitis.8 Few studies have evaluated the role of CT in the diagnosis of hematoma in the gallbladder. Hemorrhage inside the gallbladder is seen on CT as a high-density fluid and may demonstrate extravasation of the contrast in the lumen during the arterial phase.9 Eco-Doppler may help distinguish a clot from a neoplasm since the presence of flow within a mass usually indicates tumor neovascularization.10 ERCP can show evidence of bleeding in the ampulla of Vater in only 30% of patients.1
There are several therapeutic options for hemocholecyst described in the literature. They range from simple observation to cholecystectomy, depending on the severity of the damage.5 Hemocholecysts caused by trauma or by coagulation disorders can be treated conservatively as long as the patient is hemodynamically stable, symptoms improve and there are no signs of bleeding. Nonetheless, emergency cholecystectomy should be performed in cases of associated gangrenous cholecystitis in order to avoid complications such as perforation. If there is a suspected tumor, surgical treatment is indicated.3
We conclude that hemocholecyst is a rare gallbladder pathology that must be considered in the differential diagnosis of right upper quadrant pain, especially in patients with anticoagulation therapy. It can be safely resolved with laparoscopic techniques in hemodynamically stable patients.
Please cite this article as: Barbon Remis E, Martínez Menéndez A, Alexandre Hurle E, Del Casar Lizcano JM, Díez Santesteban MC. Tratamiento laparoscópico de un hemocolecisto. Cir Esp. 2014;92:293–295.