We have read the article by Gómez et al.1 discussing the importance of high-quality clinical reports in surgical departments. After analyzing the 24 clinical reports of the cases considered outliers by the hospital codification system, the paper reached the conclusion that 58% of the reports either presented insufficient data or are clearly invalid for proper codification. Similar data have been documented on reiterated occasions.2–5
First of all, we would like to congratulate the authors for dealing with an aspect of our healthcare system that is as fundamental as it is generally overlooked. And, although the authors only refer to the discharge reports after a period of hospitalization, we would also like to insist that the comments they make are likewise almost entirely applicable to outpatient consultation reports, which includes approximately 27 million primary consultations annually, a figure that is five times greater than the number of hospital admittances in the Spanish National Healthcare System (SNHS) in 2007.6
We support most of the authors’ affirmations, both with regards to the importance of medical reports as well as the quality issues detected in them. Nonetheless, we would like to make some comments on what we find interesting.
First of all, it is true that the Ministerial Order 221/1984 (6 September)7 established that it is mandatory to fill out discharge reports (including its minimum requirements) after hospitalization for all those patients treated at Spanish healthcare centers. Consequently, this excluded the mandatory requirement for clinical reports in other situations, which are becoming more and more frequent (outpatient consultations, emergency department visits, day hospitalization, ambulatory surgery, etc.).
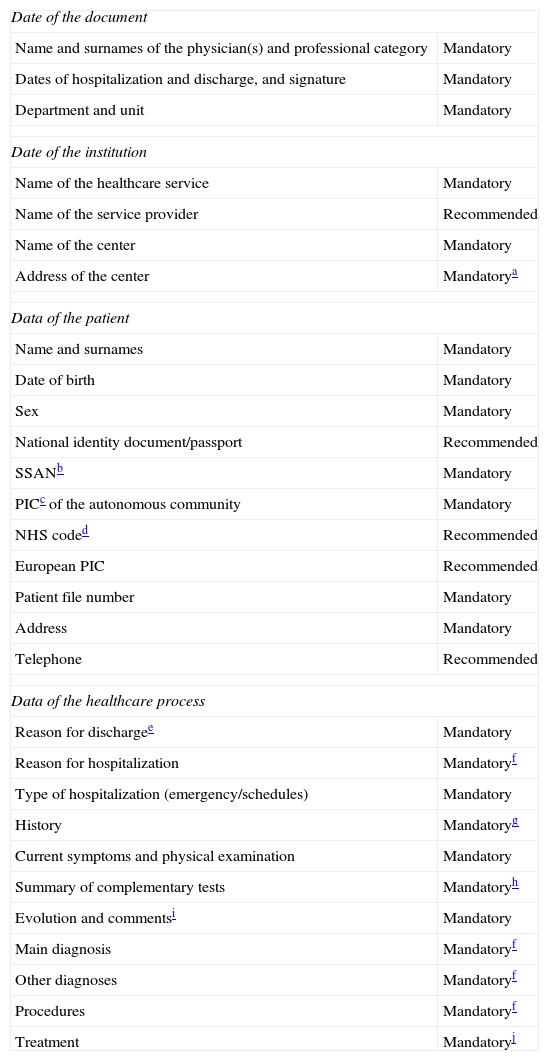
On the other hand, we feel that what was not made sufficiently clear was the fact that the minimum information that all discharge reports should contain (as well as those from outpatient consultations, the emergency department, etc.) are explicitly defined in Royal Decree 1093/2010,8 which makes their completion mandatory. In addition, this regulation does not regulate (as indicated by the authors in the references) the mandatory completion of the discharge report, but it instead establishes the minimum overall data requirement for clinical reports in the SNHS, which are shown in Table 1 for cases of hospital discharge reports. Furthermore, the regulation in question was the result of professional and institutional consensus.
Data to be Included in Clinical Reports at Discharge After Hospitalization (RD 1093/2010).
| Date of the document | |
| Name and surnames of the physician(s) and professional category | Mandatory |
| Dates of hospitalization and discharge, and signature | Mandatory |
| Department and unit | Mandatory |
| Date of the institution | |
| Name of the healthcare service | Mandatory |
| Name of the service provider | Recommended |
| Name of the center | Mandatory |
| Address of the center | Mandatorya |
| Data of the patient | |
| Name and surnames | Mandatory |
| Date of birth | Mandatory |
| Sex | Mandatory |
| National identity document/passport | Recommended |
| SSANb | Mandatory |
| PICc of the autonomous community | Mandatory |
| NHS coded | Recommended |
| European PIC | Recommended |
| Patient file number | Mandatory |
| Address | Mandatory |
| Telephone | Recommended |
| Data of the healthcare process | |
| Reason for dischargee | Mandatory |
| Reason for hospitalization | Mandatoryf |
| Type of hospitalization (emergency/schedules) | Mandatory |
| History | Mandatoryg |
| Current symptoms and physical examination | Mandatory |
| Summary of complementary tests | Mandatoryh |
| Evolution and commentsi | Mandatory |
| Main diagnosis | Mandatoryf |
| Other diagnoses | Mandatoryf |
| Procedures | Mandatoryf |
| Treatment | Mandatoryj |
E-mail address and website are recommended if they provide information of interest for the patient.
Hospital discharge or transfer to another department, hospital, rehabilitation center, voluntary discharge, death, etc.
Recommended classification in subsections (family history of disease, previous diseases, neonatal, obstetric and surgical history, allergies, addictions, vaccinations, previous medication, social/professional history and functional status).
In a recent article,9 we discussed the responsibilities that are required by all implicated parties (physicians, department/unit heads, politicians, etc.) if what truly matters is quality healthcare and not just apparent formality.
Unfortunately, in light of the article by Gómez et al. as well as others, and more than one year after the autonomous communities should have laid the groundwork to make compliance with the requirements of Royal Decree 1093/2010 possible, it seems that we have not been able to properly respond to what society demands from us.
Thus, we thank the authors for their paper because its objective is to improve the quality of clinical reports and, therefore, the healthcare that we provide. Nonetheless, and regardless of the desirable actions that each healthcare center should carry out to improve the quality of clinical reporting, it is necessary to conclude that by merely complying with the regulations in place, most of the observed deficiencies would not be averted. And this is something that, in addition to being a requirement, we should reflect upon.
We therefore insist that physicians should comply with the legal requirements with regards to clinical reporting, and we concur with the authors about the need for more structured teaching of reporting and greater supervision during the residency period. Along these same lines, it seems important that when the Spanish Society of Internal Medicine workgroup10 defined the competencies for internists, it has included among the core competencies of internal medicine the correct completion of hospital discharge, emergency and outpatient consultation reports in accordance with established standards.
Please cite this article as: Prieto De Paula JM, Sanmamed Salgado N, Otero Rodríguez JA, Franco Hidalgo S, Romo Gil JM. Sobre la importancia del informe clínico en la gestión de una unidad clínica quirúrgica. Cir Esp. 2013;91:617–618.