The Acute Care Surgery model groups trauma and emergency surgery with surgical critical care. Conceived and extended during the last 2 decades throughout North America, the magnitude and clinical idiosyncrasy of emergency general surgery have determined that this model has been expanded to other parts of the world. In our country, this has led to the introduction and implementation of the so-called trauma and emergency surgery units, with common objectives as those previously published for the original model: to decrease the rates of emergency surgery at night, to allow surgeons linked to elective surgery to develop their activity in their own disciplines during the daily schedule, and to become the perfect link and reference for the continuity of care. This review summarizes how the original model was born and how it expanded throughout the world, providing evidence in terms of results and a description of the current situation in our country.
El modelo Acute Care Surgery agrupa bajo una misma disciplina el trauma, la cirugía de urgencias y los cuidados intensivos posquirúrgicos. Concebido y extendido durante las 2 últimas décadas por territorio norteamericano, la magnitud e idiosincrasia clínica de la urgencia quirúrgica han hecho que este modelo se haya asumido en muchos otros puntos de la geografía mundial. En nuestro país, el reflejo ha sido la creación e implantación de las denominadas unidades de trauma y cirugía de urgencias, cuyos objetivos son comunes a las publicadas para el modelo original: evitar la nocturnidad en las urgencias quirúrgicas, liberar a los profesionales vinculados a la cirugía electiva en horario laboral y convertirse en el eslabón y referente perfectos de la continuidad asistencial. En el presente artículo se resumen el nacimiento y la expansión del modelo original, la evidencia aportada en cuanto a resultados y la situación actual en nuestro país.
The caseload management associated with the treatment of surgical emergencies is very high for several reasons. Its magnitude surpasses that of other recognized healthcare problems, such as de novo presentations of cancer or diabetes. More than 3 million patients are admitted annually to American hospitals, which represents 7% of all hospitalizations and results in some 850000 surgical interventions. It is estimated that 30%–40% of hospitalizations in surgery units are related with urgent care. Regarding the associated morbidity and mortality, recent studies have demonstrated that patients with surgical emergencies are eight times more likely to die than patients undergoing the same procedure as elective surgery. 90% of deaths in the first 48h after hospital admission are related with emergencies. Up to half of patients could develop some type of postoperative complication, and this rate can vary between medical centers, even in the most common urgent surgical procedures.1–6
Sub- or super-specialization in surgical subdisciplines have shown clear improvement toward excellence in very diverse areas of patient care.7–12 In severe trauma, the regionalization and certification program for American trauma centers by the American College of Surgeons Committee on Trauma, developed in the 1950s, and the subsequent creation of the National Trauma Data Bank have led to the creation and publication of several research studies, protocols and clinical guidelines. This model, which has been adopted and adapted in several countries the world over, has had a major impact on trauma care results.1,13–17
By fusing together these 2 approaches, it is logical that specific patient care by specialists dedicated to an area of maximum complexity like urgent surgery would optimize results for many reasons. In the last 2 decades, we have witnessed the training and specialization of professionals in Emergency Surgery (ES). Different models have been used in different countries, and globalization of the model has been heterogeneous based on different prior concepts of healthcare, but clear signs of response have been observed in terms of outcome indicators. This trend has also had a clear influence in our country. This article shares a general overview of specialized ES units, their conception and extension around the world, the available evidence in terms of results, steps taken at the national level and the need for ES units to be implemented in our own medical care model.
OverviewIn 2003, so-called Acute Care Surgery (ACS) committee was developed from a meeting between members of the American Association for the Surgery of Trauma, the American College of Surgeons Committee on Trauma and trauma associations from the east and west. This committee arose from the identified need to promote a specialty that would unite trauma care, ES and surgical intensive care. Several situations reinforced this need: first, the significant decrease in the resources needed to treat severe trauma due to the decrease in incidence and the increase in indications for non-operative management of different injuries, which implied the potential reconversion of trauma surgeons; and, second, the demand for specialized professionals published by the Administration, faced with the progressive and foreseeable increase in the senior population and the decreasing interest of surgeons dedicated to elective surgery for the care of emergency-related situations. These efforts culminated in the publication of a curriculum that included training in not only abdominal surgery, but also thoracic, vascular, orthopedic and even neurosurgical, with the recognition of the American Board of Surgery. Proof of its solid establishment was observed in the renaming of the Journal of Trauma as the Journal of Trauma and Acute Care Surgery.1,18 Likewise, through the American Association for the Surgery of Trauma, a study was conducted to define processes and procedures for the management of emergency surgical patients. In 2013, a list of 621 diagnostic codes was published for the first time in the 9th Edition of the International Classification of Diseases in order to convert ES into a specific research field. Subsequently, in an attempt to facilitate this definition, a review was published that reduced the 621 codes to 149.19 Likewise, 7 groups of procedures were identified that would classify about 80% of the surgical techniques developed for urgent cases.20,21
The diffusion of ACS throughout America has been progressive. In 2001, only 2% of the hospitals that treat surgical emergencies had implemented an ACS model, and by 2015 that percentage was up to 16%. The creation of ACS units in the United States continues to be influenced by its vast size, heterogeneity of distribution and population chracteristics; meanwhile, there is ongoing work toward clearly defining clinical protocols, pathways and indicators.22 Despite this, data from the National Inpatient Sample have shown significant differences in terms of hospital stay, complications and cost, and a clear trend in mortality rates in favor of trauma centers that had incorporated the ACS program compared to those without ACS or uncertified units.23
Other regions have taken the American model and adapted it to their own needs, and the worldwide implementation of this treatment concept is an established fact. Several national healthcare administrations have identified this need,24,25 resulting in the extension of the model to territories such as Canada (where in 2009 at least 13 hospitals had created an ACS unit),26 Australia/New Zealand (with an exemplary program and its 12-point plan for the foundation of ES)27,28 and several areas of Latin America,29,30 to finally begin to spread in Asian countries.31 In Europe, the design and implementation of ACS is heterogenous.32,33 A survey published in 2008, with participation representing approximately 60% of European countries, demonstrated great differences between different regions. In none of the participating countries was the ACS accepted as a subspecialty, but, nevertheless, all the respondents recognized a need and the possibility of its definition and implementation.34 The closest thing to a specific degree is probably the one recently developed by the European Union of Medical Specialists with the creation of the ES Board. In countries such as Finland, Germany, Italy, Romania or Croatia, there is support for the recognition of this discipline. In fact, professionals specifically dedicated to ES in Ireland, England, Italy, Norway or Finland are opinion leaders and coordinate units in their respective countries.
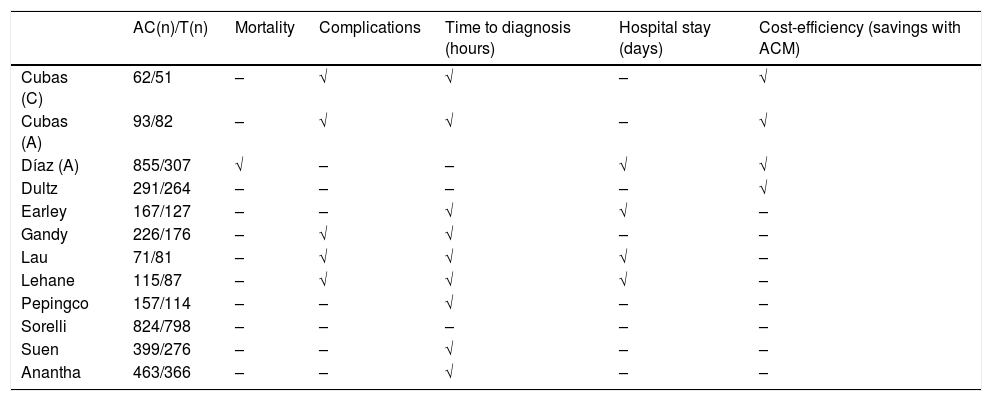
In short, although there is a clear international interest in ES and a clearly identified need for a professional collective responsible for its management, current institutional differences between political and economic systems create dispersion in the model. Moreover, on too many occasions the optimization of urgent care falls on interested physicians more than professionally trained and certified medical professionals. It has already been demonstrated that a single model (the so-called ‘one-size-fits-all’) would not work for ES if it is not adapted to a specific current and geographic reality.2,5 However, whatever the model implemented, as they distance themselves from the traditional on-call system of surgeons with no specific interest or training, these units demonstrate excellent results based on indicators in different areas of urgent care, including economic aspects, as has been concluded in different systematic reviews (Table 1).35,36
Variables Showing a Significant Impact of the Implementation of the Acute Care Model Over the Traditional Model.
| AC(n)/T(n) | Mortality | Complications | Time to diagnosis (hours) | Hospital stay (days) | Cost-efficiency (savings with ACM) | |
|---|---|---|---|---|---|---|
| Cubas (C) | 62/51 | – | √ | √ | – | √ |
| Cubas (A) | 93/82 | – | √ | √ | – | √ |
| Díaz (A) | 855/307 | √ | – | – | √ | √ |
| Dultz | 291/264 | – | – | – | – | √ |
| Earley | 167/127 | – | – | √ | √ | – |
| Gandy | 226/176 | – | √ | √ | – | – |
| Lau | 71/81 | – | √ | √ | √ | – |
| Lehane | 115/87 | – | √ | √ | √ | – |
| Pepingco | 157/114 | – | – | √ | – | – |
| Sorelli | 824/798 | – | – | – | – | – |
| Suen | 399/276 | – | – | √ | – | – |
| Anantha | 463/366 | – | – | √ | – | – |
AC and ACM: Acute Care and Acute Care Model; C: cholecystectomy group; A: appendectomy group: N: number of patients.
Several international medical societies are trying to develop structure and support for ES with the aim to minimize these implementation biases. The World Society of Emergency Surgery has developed several programs, such as the appointment of national delegates, providing courses related to several different aspects of ES (all of them united in a single training program called Full Immersion in Acute Care Surgery and Trauma), the creation of several international registries (World Society of Emergency Surgery International Registry of Emergency General Surgery or WIRES Project; International Registry of Open Abdomen; International Registry of Biological Prosthesis) or the creation of a certification program of hospitals linked to the society.37 The evolution and results of all these initiatives, as well as other studies with different formats related to clinical activity, can be consulted in its official publication, the World Journal of Emergency Surgery. Their invaluable work has also led to the definition of 119 indicators for 20 processes, which has set the current bar for other units or medical professionals involved in urgent surgical activity.38 Other societies are also involved in this area of care management: the World Society of Abdominal Compartment Syndrome, the International Association for Trauma Surgery and Intensive Care, associated with the International Society of Surgery, or the European Society for Trauma and Emergency Surgery European, also with its own journal, the European Journal of Trauma and Emergency Surgery.
Results Associated With the Acute Care Surgery ModelThe clinical and economic impact of urgent care at American trauma centers with ACS programs has been previously discussed.23 These results have been reproduced in hospitals without trauma care but with ACS units, reporting significant reductions in hospital stay, morbidity and costs after the creation of the unit, both globally (morbidity 21% vs 12%, P<.0001; hospital stay 6.5 vs 5.7 days, P<.0016; hospital costs $12009 vs $8306, P<.0001) as in the focal analysis of diseases like appendicitis or cholecystitis.39 The results of a systematic review support the implementation of any specific dedication system for emergency surgical treatment over the traditional model in both clinical and economic terms.36 They have managed to significantly increase the number of patients treated, surgical procedures performed and the displacement of these surgeries to the morning shift, avoiding night surgeries except for emergencies. Miller et al. reported an increase in the number of urgent surgeries performed in a period of 2 years of more than double after the creation of an ACS unit, with no impact on elective activity.40 The Canadian experience of Anantha et al. demonstrates the change in the time distribution that these units provide: before its creation, the authors reported 366 urgent operations, 24% during the day, 55% during the afternoon/evening and 21% at night, while after the creation of the unit, 463 surgeries were performed during a predominantly daytime schedule (55% during the day, 36% in the afternoon/evening and 9% at night), with statistically significant results in terms of overall quantity and distribution (P<.001).41 Diagnostic times are significantly reduced and, therefore, pressure is reduced in the emergency department.42 These are just some of the aspects that justify the economic impact associated with the creation of these units, as previously discussed.
As for indicators for diseases, the available evidence confirms that the implementation of an ES unit leads to a clear improvement in outcomes in the most prevalent pathologies in the field of surgical emergency: acute appendicitis and cholecystitis.43,44 A recent meta-analysis including 14 studies and 7980 patients concluded that patients with acute appendicitis treated in hospitals with ACS units have a shorter delay before surgery (−0.4; 95% CI −0.65 to −0.15; P<.02), a shorter postoperative hospital stay (−0.25; 95% CI −0.46 to −0.05; P<.02) and a lower rate of complications (OR 0.76; 95% CI 0.59 to 0.99; P<.04).45 In the meta-analysis by Murphy et al. these results likewise construct a reality in which patients with appendicitis and biliary disease show a decrease in both postoperative stay (0.51 days for appendicitis, 95% CI −0.81 to −0.20; 0.73 for biliary disease, 95% CI 0.09 to 1.36) as well as complications (OR 0.65 for appendicitis, 95% CI 0.49 to 0.86; OR 0.46 for cholecystitis, 95% CI 0.34 to 0.61) when they are treated at medical centers with specific emergency care programs.46 This same publication reveals a very important fact: only those hospitals with an operating room specifically designed for urgent activity have the change in trend in terms of night surgery. Some studies have reported significant reductions in the conversion rate in laparoscopic cholecystectomy due to acute cholecystitis.43 In intestinal obstruction, more aggressive approaches have been described in ES units for CT diagnosis, early surgical indication (if it exists) as well as shorter time to surgery, which have significantly reduced the associated mortality (5.8% before vs 2% after the creation of the specialized unit, P<.02).43,47 Several articles have advocated the care provided by these units in malignant bowel obstruction,48,49 and very diverse literature references have been used to develop clinical guidelines for different diseases by ES professionals worldwide.50,51 These results have been supported by studies in our country.52–54
The Situation in Spain: Trauma Units and Emergency SurgeryWith a solid training program to back it up, the ES care model in our country with a format of 24h in-hospital on-call shifts probably does not require a complex structural change. However, there are several undeniable problems associated with our model. Surgeons designated for these shifts are those who, during scheduled work hours, are dedicated to subspecialties related to elective surgery and would prefer to operate during the morning, without the need to reschedule the activity in their respective divisions. Their dedication to a specific area, such as breast or thyroid surgery, partially disassociates certain physicians from urgent abdominal surgery. Occasionally, problems with the availability of an operating room for the resolution of daytime emergencies make nighttime surgeries necessary. With these interferences, sometimes certain surgical emergencies suffer an excessive delay in their resolution, with the potential risk of complications developing.
With units comprised of professionals who are selectively dedicated to working in the ES, a double benefit is obtained: first, it frees up the schedule of designated on-duty surgeons during the work day and, second, night surgery can be delayed, with the guarantee that it will be carried out first thing in the morning by a specifically dedicated team. However, these units should meet another unavoidable objective: they become the central axis around which all the urgent surgical activity of a surgical department pivots and opinion leaders based on specific training and dedication, while being a reference for other surgeons who share this activity during their shifts. The scope of ES also enables surgeries to be done during daytime hours, which reduces the caseload throughout the rest of the day.
The setting in which these units should be created is a reference hospital with a high demand for urgent care. Most medical centers where care management is organized by subspecialties are appropriate. The staff of the unit should include a coordinator with interest and experience in surgery, along with a sufficient number of physicians to ensure coverage of treatment requirements. At least one operating room, a specific hospitalization area and at least one consultation for office visits should be selectively assigned for the activities of the emergency surgery unit, as defined through a portfolio of services agreed with other surgical units and adapted to the needs of the department and hospital.
Furthermore, these units are the ideal situation for physicians expressly trained in severe trauma care. Although there are other formats, in Spain this training is intrinsically linked to the Advanced Trauma Life Support programs of the American College of Surgeons and Definitive Surgical Trauma Care of the International Association for Trauma Surgery and Intensive Care, organized through the Spanish Association of Surgeons. The components of the ES units must be specifically trained and later become involved in the programs as unit heads or instructors, thereby ensuring continuous recycling. These surgeons are also leaders in their own surgical service and hospital, involved in the development of adapted diagnostic and therapeutic algorithms and actively participating in specific commissions.
With this philosophy, these professional groups should be denominated the Trauma and Emergency Surgery Unit (TESU). Daily clinical sessions are held for incoming on-call physicians, centralizing the resolution of both acute processes and deferred urgent surgery. The Unit also works in close association with other departments, such as Radiology, Intensive Care, Emergency or Gastroenterology, both in multidisciplinary treatment schemes and for making diagnostic or therapeutic decisions. All of this occurs during daytime working hours to become the perfect link in the continuity of urgent care between the previous night and the following evening.
The Trauma and Surgical Intensive Care Division of the Spanish Association of Surgeons was aware of the change in strategy worldwide in the management of surgical emergencies and changed its name to Trauma and Emergency Surgery Division. Initially, attention was given to severe trauma (with the training courses Advanced Trauma Life Support and Definitive Surgical Trauma Care). Coinciding with this reality and with the birth in Spain of TESU, we have been promoting ES in our country, and the topics chosen for 2 roundtables at medical conferences and national meetings have addressed this. Recently, its ES guide has been completed in collaboration with other divisions. It has also promoted and endorsed related courses to be implemented at the national level (Modular Ultrasound European Society for Trauma and Emergency Surgery Course – an ES course for surgery residents, responsible for the scientific diffusion with residents in their second year, whose first edition was held this year), as well as various scientific meetings related with trauma and ES. Meanwhile, logistic issues are being resolved to organize a regular meeting of the division. A national registry for serious trauma open to all hospitals has been set up, and different agreements with top-level trauma centers have been reached (NYU Winthrop Hospital, in New York, and Chris Hani Baragwanath Academic Hospital, in Johannesburg). These training stays at trauma centers also include other activities in Colombia, Ecuador, Finland, Los Angeles, Boston and Pittsburgh, and are widely solicited by residents and need to be requested more in advance.
In 2014, as an initiative of the division, a nationwide emergency care survey was conducted in our country, sent by e-mail to all members of the Spanish Association of Surgeons. The most notable data of that survey was that in 307 responses obtained from 45 provinces in 16 different autonomous communities (which ensured representation of a significant portion of the national territory), some 54.1% reported the need to operate on non-life-threatening emergencies at night, and that hospitals with a fully established TESU reported a lower need for this type of surgery (22.2% vs 57.1%, P<.00) and a greater use of the operating room during the morning for urgent surgeries (69.3% vs 29.5%, P<.00). More than 75% of responding hospitals had positively integrated a TESU; these results transmit a perceptible reality.55
Currently, there are only 7 TESU at hospitals of the highest level in Spain, 5 of which are in Andalusia. The TESU at the Hospital Virgen del Rocío in Seville was the first in our country, followed by the Hospital Regional Universitario in Malaga and Virgen Macarena, also in Seville. The Complejo Hospitalario in Jaén and the Hospital Universitario Reina Sofía in Córdoba complete the list of hospitals in Andalusia, a community that is especially active in the field of surgical emergency. The 5 share common concerns and guidelines under the auspices of the Andalusian Association of Surgeons in the Andalusian Group of Trauma and Emergency Surgery. Two more TESU have been established with the same care premises and structure at the Hospital Universitario Nuestra Señora de Candelaria in Tenerife, and at the Hospital Universitario Donostia. Many other professionals with special interest and great preparation in ES are linked to the division, but their daily caseload is not organized under such a clearly established unit structure or in other disciplines. Several hospitals have shown interest and have started to design TESU without complying with the minimum requirements, resulting in a lack of continuity. A certification program is currently under evaluation, as proposed by the division, in order to verify the foundation and quality standards of the existing TESU and newly created TESU, which will be designed prospectively and continuously.
ConclusionThe concept of emergency surgical care as ACS is here to stay. Whatever the implementation model chosen, exclusive dedication to trauma and ES leads to improved clinical-care outcomes for other surgical subspecialties. However, the road is long and progress is slow,56 and our country is a clear reflection of the global situation around the world. In our own setting, TESU should be incorporated a unit of the Surgery Department, with adequate resources and full support. The TESU should be included in the program of sessions or resident rotations, providing surgical management during standard work hours. As a result, night surgeries would decrease, on-call staff would be able to carry out their elective work and, above all, the treatment of urgent surgical patients would be optimized throughout the entire department. All referral centers with a high number of physicians and a large caseload requiring urgent treatment should work toward creating a TESU that, once it is functioning and in continuous training and recycling, will be able to structure, protocolize and record the urgent surgical activity of the hospital.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Aranda-Narváez JM, Tallón-Aguilar L, López-Ruiz JA, Pareja-Ciuró F, Jover-Navalón JM, Turégano-Fuentes F, et al. El modelo Acute Care Surgery en el mundo y la necesidad e implantación de unidades de trauma y cirugía de urgencia en España. Cir Esp. 2019;97:3–10.