The use of a rigid tube endoscope (RTE) through a laparoendoscopic single site surgery device for intracavitary visualization during endoscopic uniportal surgery (EUS) is directly related to the fulcrum effect and physical competition (externally between surgeons and on instrumentation through the single port). These facts may have precluded a wider spread of EUS. In an attempt to separate the imaging system from the laparoendoscopic single site surgery device, a tiered project (3 models) that can help overcome these drawbacks is detailed. ZEUS1, a new non-RTE imaging system device for EUS was successfully tested in EUS surgery in a pig model. Still under investigation, ZEUS2 becomes a wired structure that serves as the basis for an endoscopic microcamera with intracavitary pan-tilt-zoom functions. ZEUS3 uses the inner ring of the surgical wound protector as a microchamber crown. Further studies are needed to materialize the ZEUS2 and ZEUS3 models and confirm their efficacy and safety.
El uso de un endoscopio de tubo rígido (RTE) a través de un dispositivo de cirugía laparoendoscópica de puerto único durante la cirugía endoscópica uniportal (EUS) está directamente relacionado con el efecto fulcro y la competencia física (entre cirujanos y a través del puerto).
En un intento de separar el sistema de imagen del dispositivo cirugía laparoendoscópica de puerto único, se describe un proyecto escalonado (3 modelos) para ayudar a superar estos inconvenientes. ZEUS1, un nuevo dispositivo de sistema de imagen sin RTE para EUS, fue probado con éxito en cirugía EUS en un modelo porcino. Aún en investigación, ZEUS2 se convierte en una estructura cableada que sirve de base a una microcámara endoscópica intracavitaria con funciones de giro, inclinación y zoom. ZEUS3 contempla el aro interno del protector de herida quirúrgica como una corona de microcámaras. Son necesarios nuevos estudios para materializar los modelos ZEUS2 y ZEUS3 y confirmar su eficacia y seguridad.
Endoscopic multiportal surgery (EMS) is currently the standard minimally invasive surgical approach for most of the surgical procedures performed, being necessary prior gas insufflation in most of them. Developed under this concept, uniportal endoscopic surgery (EUS), unlike EMS, employs a single surgical port. EUS is currently performed in surgical interventions on the abdominal cavity (Single Incision Laparoscopic Surgery (SILS)) and thoracic cavity (Uniportal Videoassisted Thoracic Surgery (Uniportal VATS) and Heart Port Surgery)1–6. Similarly, robotics has made innovation in EUS7.
Several articles have reported benefits, complications and comorbidities of EMS and EUS compared to open surgery in relation to early postoperative recovery, less pain or hospital stay2,8–13.
EUS uses a device (Endoscopic Single Site Surgery device (ESSS)) that brings together several surgical ports in a single appliance. Through a single skin incision, an ESSS device, allows an image system and several endoscopic surgical instruments to be introduced into an organic cavity while supplying and maintaining a certain CO2 pressure.
Standard image system for EUS is nowadays delivered by a rigid tube endoscope (RTE) that accesses the organic cavity through one of these ports available at the ESSS device. The combination of RTE-ESSS device during EUS conditions two main technical disadvantages. Firstly, mobility of the camcorder located at the intracavitary tip of the RTE is reduced due to a fulcrum effect. Secondly, since the RTE is held and orientated towards a common target anatomy by the assistant surgeon, physical space competition (externally between surgeons and on instrumentation through the single port) appears for both the assistant and main surgeon.
In the attempt to split the imaging system from instrumentation while preserving CO2 intracavitary pressure, previous experiences of endoscopic microcameras for endoscopic surgery (ES) have been published14–17.
In this paper and under these concepts, various EUS were feasible in an experimental study in swine with a new non RTE intracavitary imaging system (ZEUS1; standing for Zooming Endoscopic Uniportal Surgery model 1) that splits the imaging system from instrumentation and supplies intracavitary vision without employing any port of the ESSS device while maintaining intracavitary CO2 pressure. ZEUS2 and ZEUS3 models are also introduced. The author hypothesizes that this device may help addressing the aforementioned constraints.
Surgical techniqueThree large white male pigs (25.2 ± 3.7 kg) from the animal university facility were studied. These animals were euthanized before surgery following guidelines of the European Animal Protection Law (Directive 2010/63/EU of the European Parliament). The study was developed in the Anatomy and Comparative Pathology University Department. Ethical Committee animal experiment university service approval was obtained before beginning this study. All experiments were undertaken in October 2018.
ZEUS1, standing for Zooming Endoscopic Uniportal Surgery model 1, is a non RTE intracavitary imaging system that splits the imaging system from instrumentation and supplies intracavitary vision without employing any port of the ESSS device while maintaining intracavitary CO2 pressure during EUS.
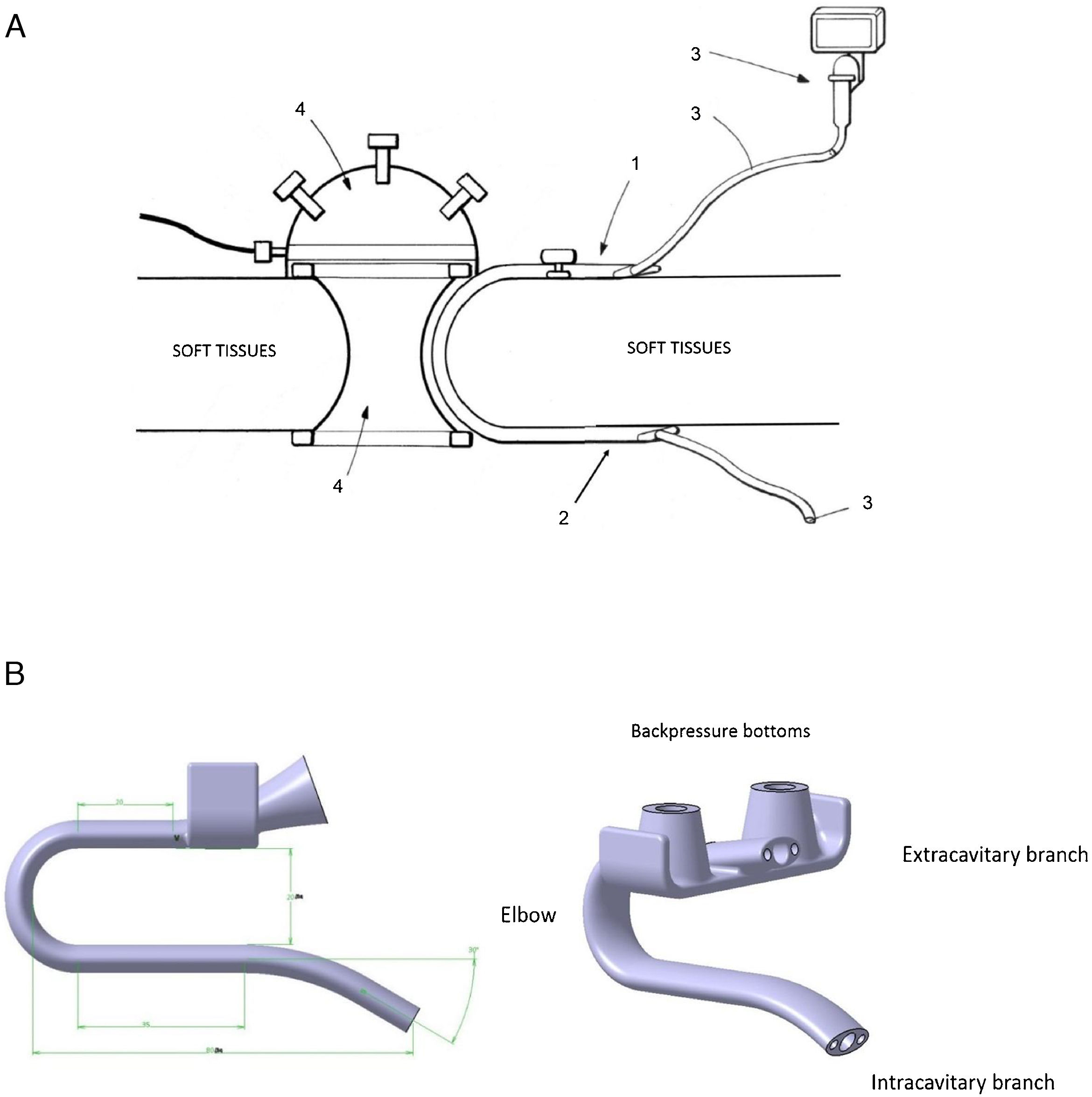
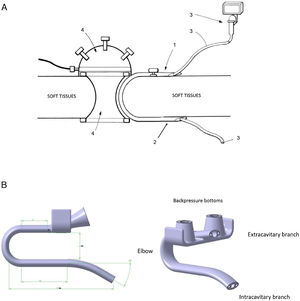
ZEUS1 was designed as a U-shaped device that runs between the wound protector-ESSS system and the soft tissues so as to preserve CO2 intracavitary pressure. Its hollow section allows for the introduction of a videofibrebronchoscope (VFBC) through it (Fig. 1.1, 1.2).
The intravitary branch of ZEUS1 is introduced through de single incision prior to the ESSS device placement. ZEUS1’s capability to pivot by manipulation and the flexibility of the VFBC provides broad image angles towards a target anatomy (Fig. 2. Videoclips 1–2). Back pressure buttons were added for wall attachment (videoclip 3). Distance between branches of ZEUS1 could be modified based on the thickness of the soft tissues.
The current material of the ZEUS1 model device is polyamide PA12. This material is sufficiently rigid but flexible enough so as not to break while allowing its manipulation and stretching.
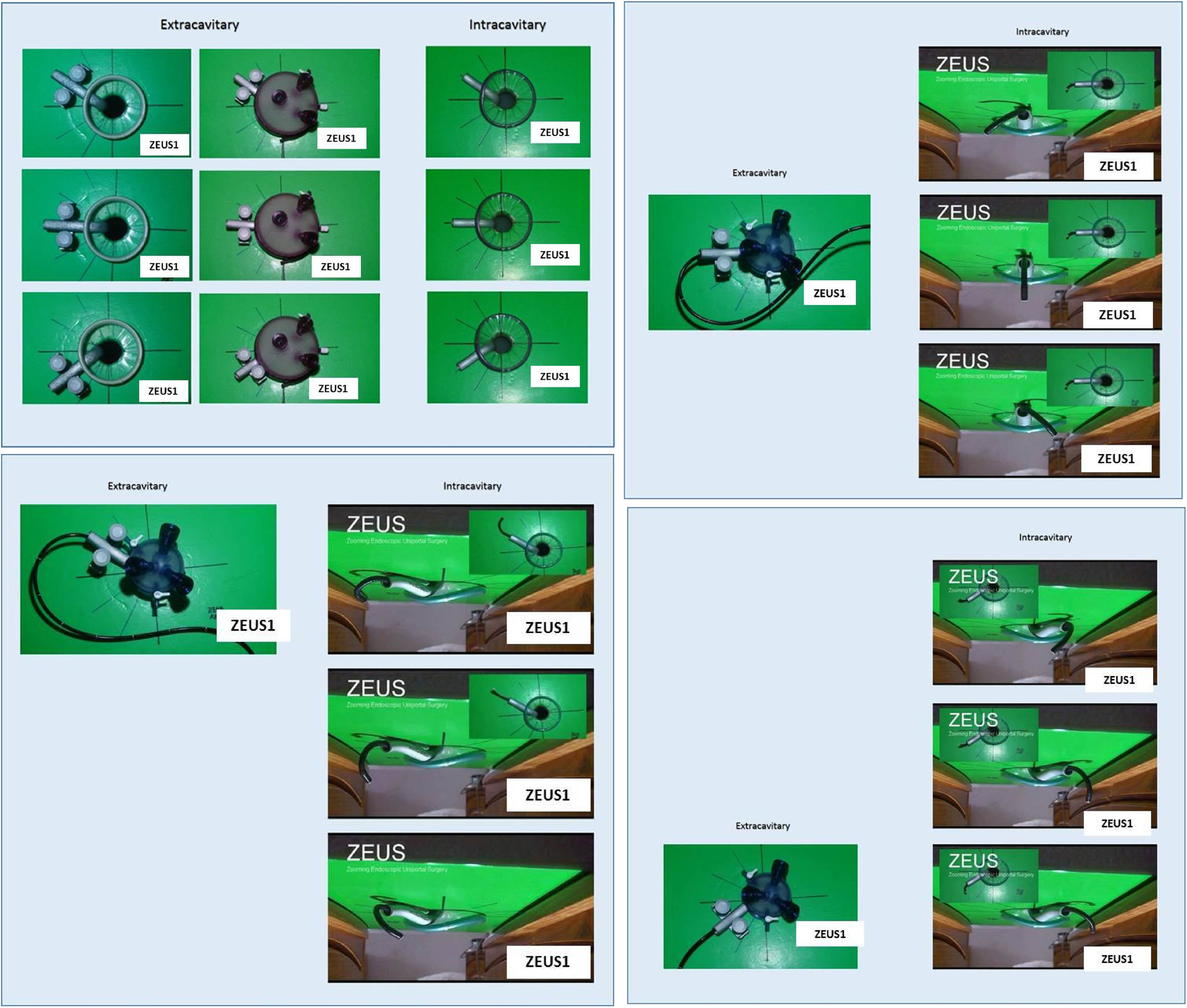
In order to evaluate the functionality of the device, surgery was recorded simultaneously with four cameras:
- •
Two of them intracavitary: Camera 1: a VFBC that peeked through ZEUS1. Camera 2: a RTE was responsible for showing the movements of the VFBC and ZEUS1 during surgery. At no time was it used to guide surgery to the main surgeon.
- •
Two of them extracavitary: Camera 3: zenital on the operating table. Camera 4: extracavitary perimeter that recorded surgical gestures.
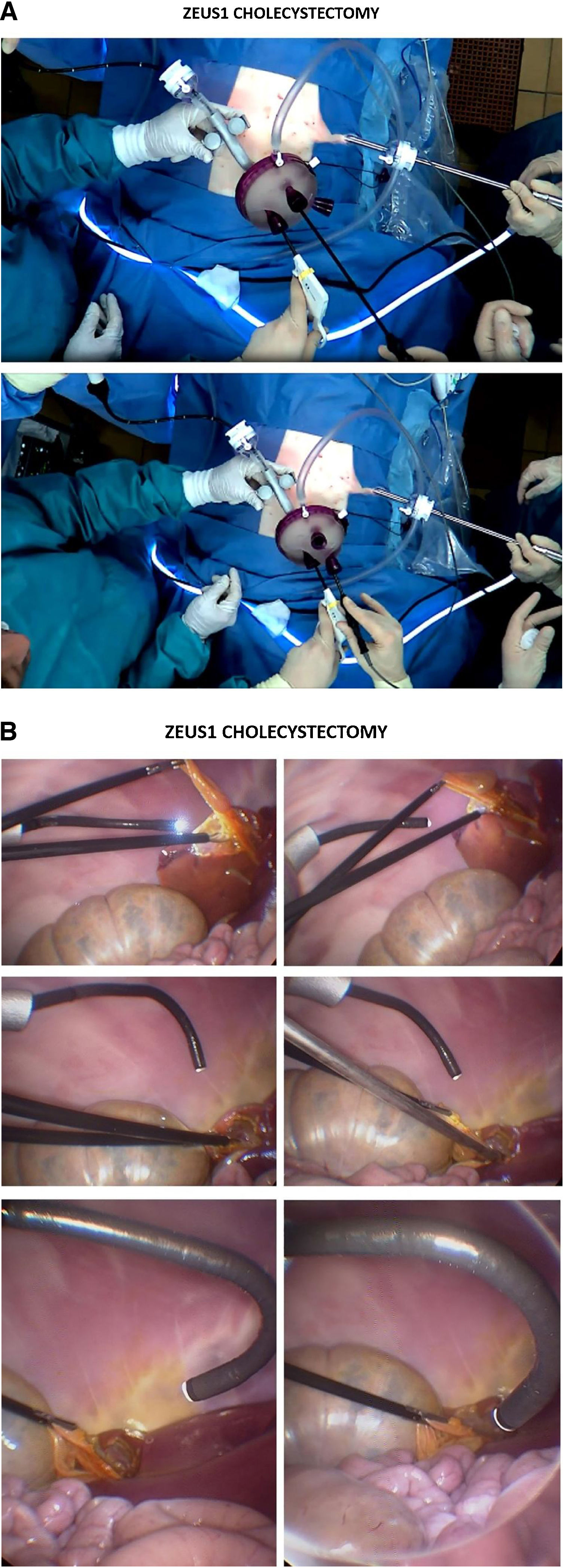
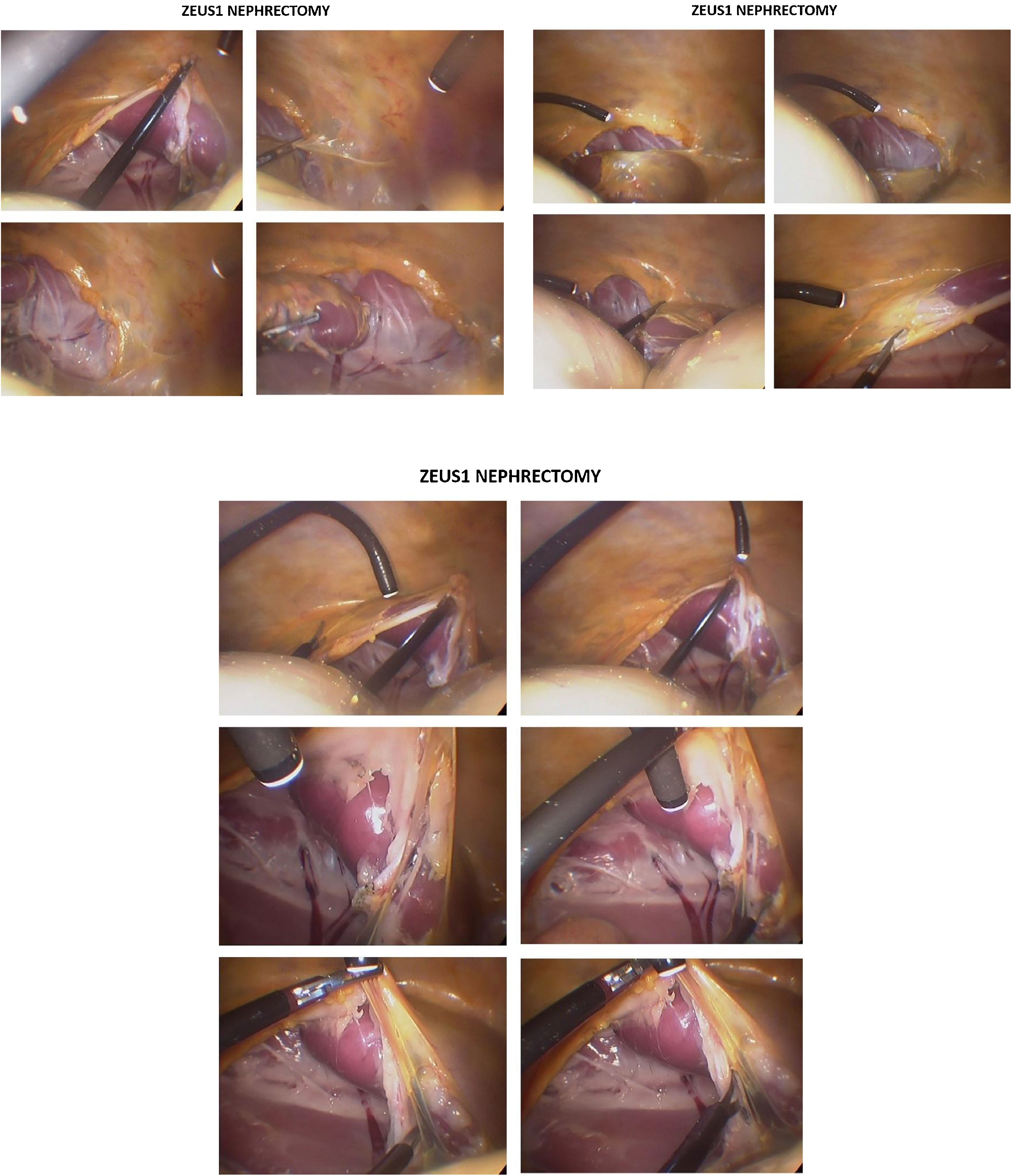
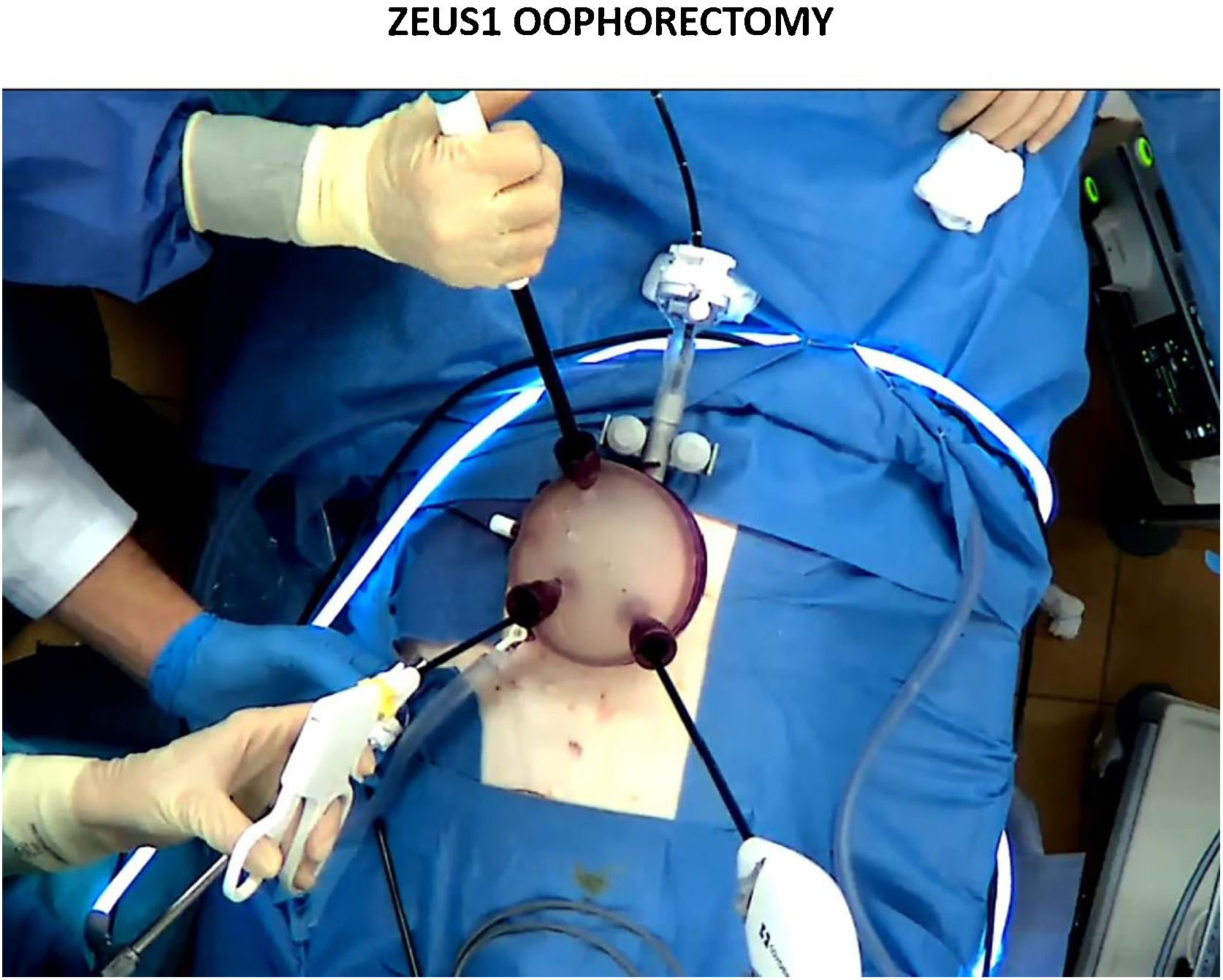
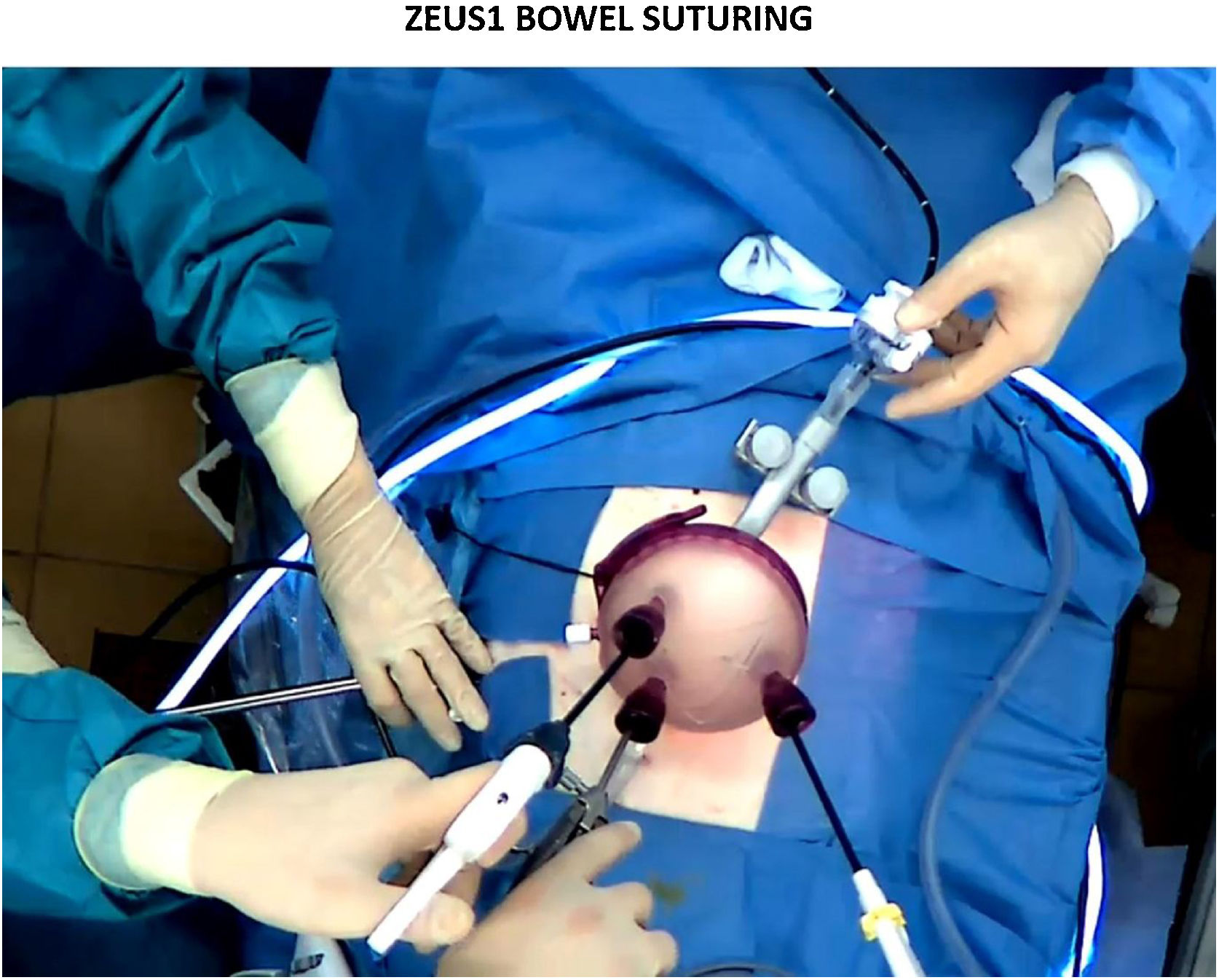
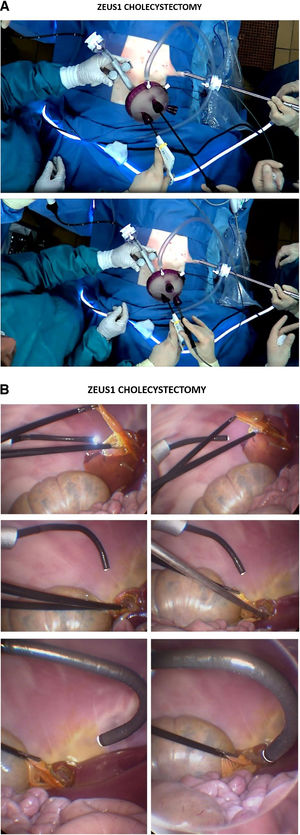
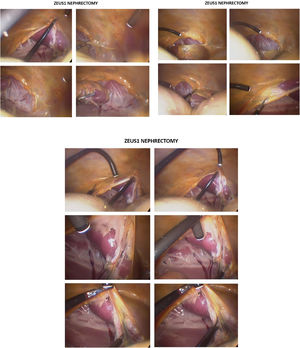
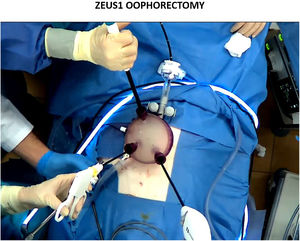
Surgical procedures of cholecystectomy (Fig. 3.1, 3.2, videoclip 4), nephrectomy (Fig. 4, videoclip 5), oophorectomy (Fig. 5, videoclip 6) and bowel suturing (Fig. 6, videoclip 7) in a porcine model were completed by uniportal laparoscopic surgery implemented with ZEUS1. The VFBC employed (the only one available for experiments with cadaver animals), with a diameter of 5.5 mm, conditioned a ZEUS1 section of 1.2 cm in diameter (a VFBC of 3.4 mm would have reduced this diameter). Some non-significant pneumoperitoneal leakage was observed but did not make surgery any difficult. Limited image performance of the flexible endoscope employed (compared to a rigid one) did not hinder surgery.
We employed the available VFBC for animal experiments (TJF 180 Olympus Tokyo, Japan) which conditioned a section ZEUS1 diameter of 1.2 cm (a 3.4 mm VFBC would have reduced this diameter). Surgical endoscopic tools employed during surgery were: LESS device (Gelpoint® Advanced Access Patform, Applied Medical, CA, USA), bipolar energy (Maryland LigaSure™, Medtronic, Ireland), staplers (Endo GIA™ Tri-Staple™ Vascular/Medium, Medtronic, Ireland) and other endoscopic instruments (Endo Clinch™, Endo Shears™, Endo Retract™, Versaone™ Optical Trocars, Medtronic, Ireland).
The primary endpoint of the study was to evaluate the quality and degrees of exposition of image achieved with ZEUS1. The secondary endpoints were the evaluation of the facility of insertion, placement and pivoting displacement of ZEUS1 during EUS surgeries.
So as to the primary endpoint, while preserving the standards, ZEUS1 offered some new not previously achievable intracavitary images (mainly angles of entrance and exit while dissection) compared to those of EUS with RTE.
Some secondary endpoints were observed:
- •
ZEUS1 allowed triple endoscopic instrumentation without interfering with the imaging system during EUS. Three endoscopic trocars aiming at different directions were used while the imaging system was provided by ZEUS1. Competition for external physical space was eliminated and that for internal, considerably reduced.
- •
By pivoting, ZEUS1 allowed for lateral displacement of the imaging system. The workshop has shown that its internal branch can be displaced 30–45° in both directions with respect to the axis of attack of the surgical instruments towards the anatomical target. Device displacement together with the turning capacity of the VFBC allows for a correct visualization of the anatomical target.
Most major surgeries are nowadays performed through a minimally invasive approach (SILS, Uniportal VATS or HeartPort)1–6,18. Scientific literature has been published on its benefits and complications2,8–13,19.
There are several factors that influence the penetration of EUS into the surgical community. Some of them are directly related to the institution such as the existence of a training program to tutor the acquisition of skills on surgical technique and decision until the completion of the learning curve minimizing the risks to the patient. Others, however, depend directly on the surgeon’s skills, available resources or physical conditions during surgery.
The fact that the current imaging system during EUS is supplied by an RTE, which uses one of the ports of the ESSS device, determines physical competition (externally between surgeons and on instrumentation through the single port) and a fulcrum effect during surgery. ZEUS1 was designed with the intention of splitting the image system from instrumentation during EUS with an ESSS device while preserving CO2 intracavitary pressure.
ZEUS1 image system was tested in 3 animals and guided procedures of cholecystectomy, nephrectomy, oophorectomy and bowel suturing with excellent technical success, proof of feasibility and pivoting capacity. However, ZEUS1 is an initial product of a research project still in development.
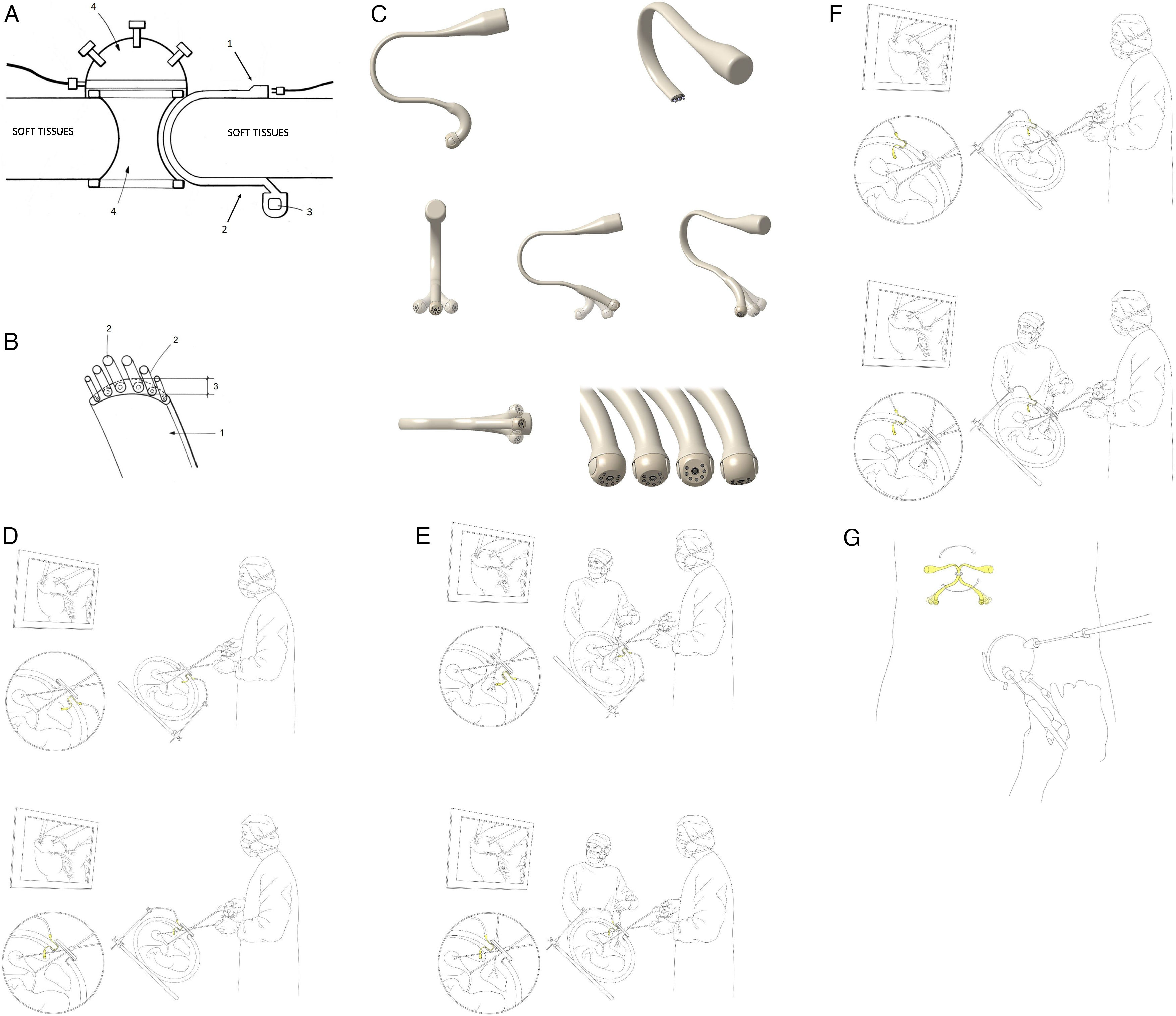
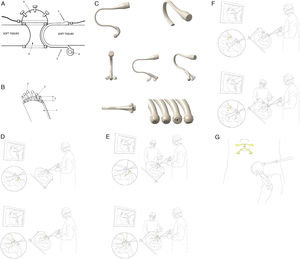
ZEUS2 model reduces its diameter since its section will only contain wiring (for energy, cold light, video signal or articulating/telescopic wires) (Fig. 7.1 y 7.2). Image system is delivered by a pan-tilt-zoom (PTZ) microcamera/s located at the distal end of its intracavitary branch. ZEUS2 image angles will be obtained by firstly, pivoting movements of the device, secondly, complemented with intracavitary articulated or telescopic displacement of the inner branch and, finally, by PTZ microcamera functions (Fig. 7.3). ZEUS2 attachment will rely on an articulating surgical support and location of the device may switch proximal or distal from main surgeon (Fig. 7.4). ZEUS2 will allow for triple endoscopic instrumentation without interfering with the imaging system (Fig. 7.5). Remote control functions (e.g. oral, eye-movement, target tracking capability) may progressively replace wiring in ZEUS2.
(A). ZEUS2 scheme. (1) ZEUS2 extracavitary branch. (2) ZEUS2 intracavitary branch. (3) PTZ microcamera. (4) LESS device. (B). ZEUS 2 section. (1) ZEUS2 section. (2) Wiring. (3) ZEUS2 diameter, 3 mm. (C) ZEUS2 design. (D) ZEUS2 surgical field sections. Positioning of ZEUS2 proximal or distal to main surgeon. (E) ZEUS2 surgical field sections. Triple instrumentation with assistant surgeon. (F) ZEUS2 surgical field sections. Biportal endoscopic surgery.
Although ZEUS2 has been designed to address the technical disadvantages of EUS, it does not exempt its use in EMS, also offering the possibility of replacing the RTE to implement the imaging system during EMS (Fig. 7.6). To this respect, ZEUS2 will address factors that influence the ergonomics of minimally invasive surgery, freeing the assistant surgeon from imaging system control20.
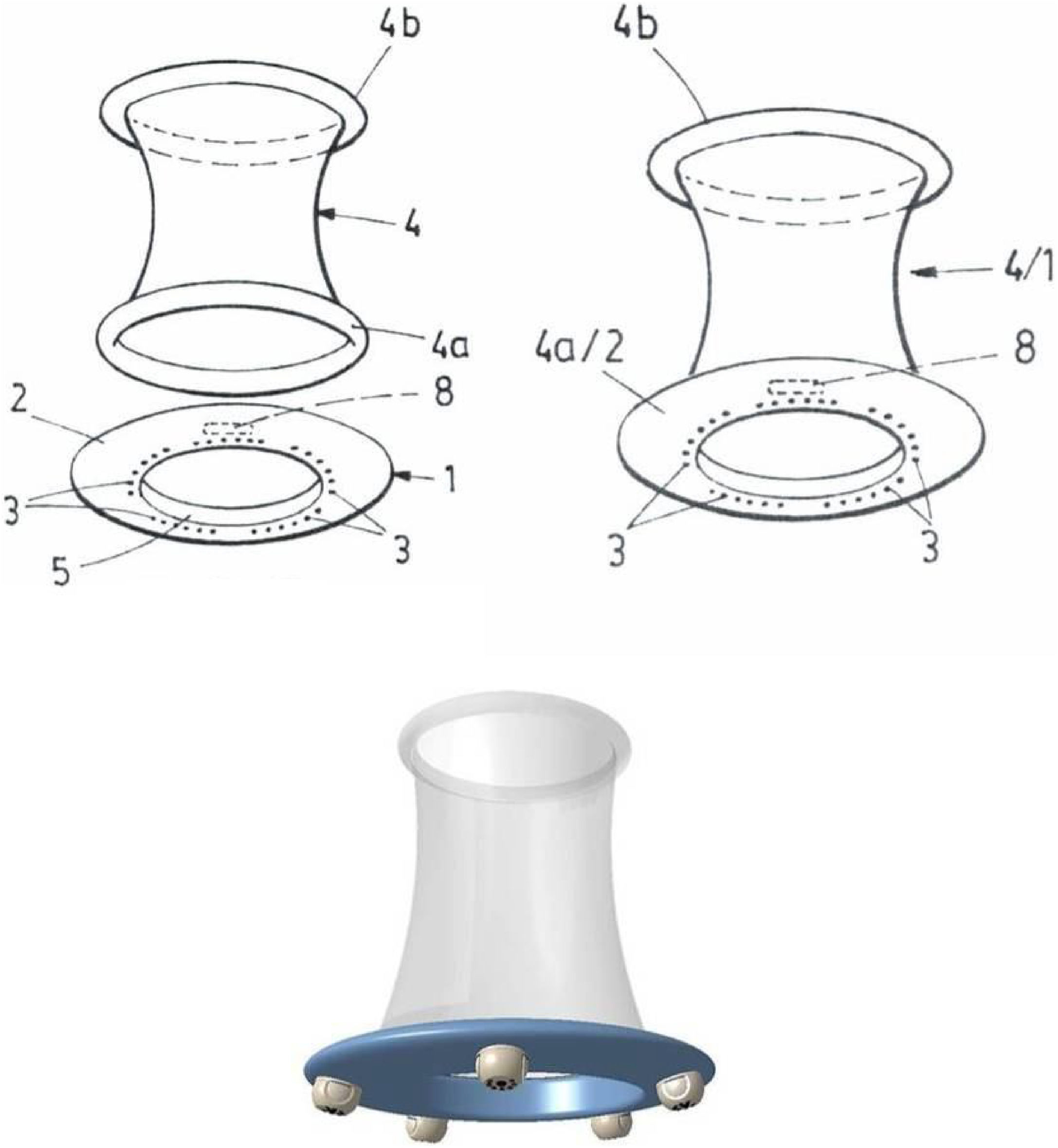
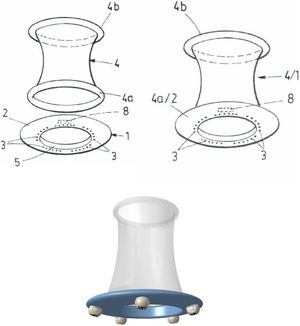
ZEUS3 is designed as a device where the intracavitary ring of the surgical wound protector would serve as a support or would be in itself a crown of endoscopic microcameras with PTZ functions (Fig. 8). The introduction through the single port of this type of crown with microcameras will be a challenge, but there already exist published papers on insertable endoscopic microcameras14.
ZEUS1 has successfully helped addressing the two main drawbacks (fulcrum effect and physical competition (externally between surgeons and on instrumentation through the single port) associated with EUS. Further investigation is necessary to determine whether ZEUS2 and ZEUS3 may play a role in totally or partially replacing the actual RTE imaging system during EUS and/or EMS.
Conflict of interestsThe authors declare that they have no conflict of interests.
AcknowledgementsThe author would like to thank the following for their contributions: Jesús Martínez Baños, MD; Dr Patricia Martínez Martínez, MD, PhD; Dr María José Roca Calvo, MD, PhD; and, Dr Juan Torres Lanzas, MD, PhD. Likewise, he would like to express his gratitude to the following people from the Department of Comparative Anatomy and Pathology: Dr Nuria García Carrillo, PhD and Dr Rafael Latorre Reviriego, PhD.
Please cite this article as: Arroyo Tristán A. Separación del sistema de imagen del dispositivo de cirugía laparoendoscópica de puerto único en cirugía endoscópica uniportal: proyecto ZEUS. Cir Esp. 2022;100:161–170.