The consolidation of distal pancreatectomy (DP) in laparoscopic surgery is supported by several published studies that demonstrate the safety and efficacy of this technique.1–3 At the same time, the current trend toward being less and less aggressive has led to the development of single-port surgery. These techniques are being applied in new diseases and organs each day, while increasingly complex techniques are being developed.4–6 Some authors suggest that single-port DP may become a reality in the not-too-distant future. However, the current experience in single-port DP is limited, and only a few cases have been reported in the literature.7–9 Nevertheless, we believe that in the hands of experienced laparoscopic surgeons, single-port DP is a promising surgery that will increasingly develop in coming years. We present our initial experience with single-port distal spleno-pancreatectomy.
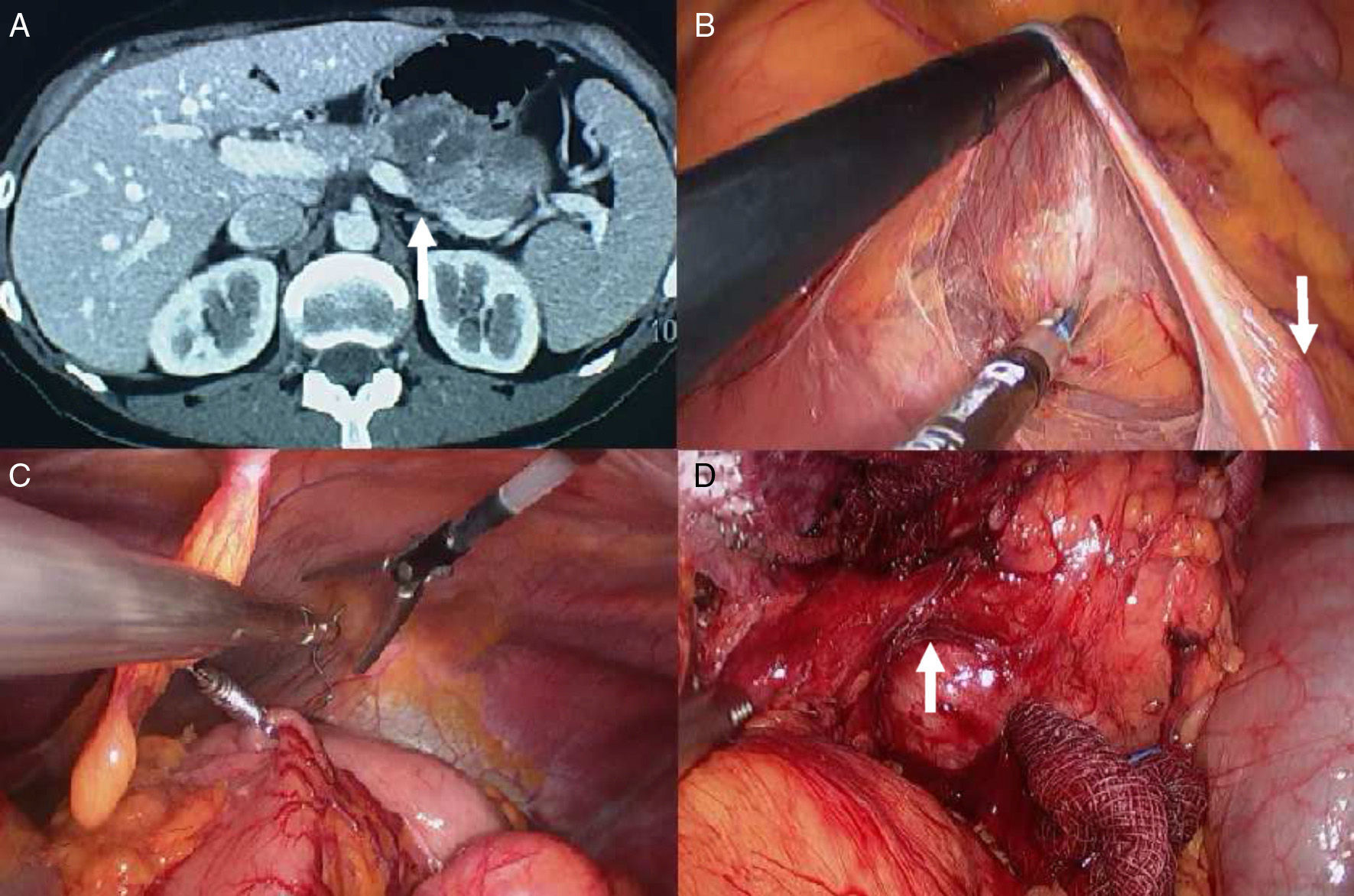
This case is a 39-year-old patient, with no prior history of interest, who came to our consultation due to abdominal discomfort. Abdominal ultrasound detected a lesion measuring 45×43mm in the body/tail of the pancreas. The preoperative evaluation included a CT scan with IV contrast and oral endoscopic ultrasound, which showed a 5×5cm mass at the junction of the body and tail of the pancreas, consistent with a possible pseudopapillary tumor with inner necrosis that infiltrated the splenic vein (Fig. 1A). No lymphadenopathies were identified. FNA confirmed an epithelial neoplasm suggestive of malignancy. Subsequently, the patient was scheduled for single-port distal spleno-pancreatectomy.
(A) Abdominal CT scan with contrast. The arrow indicates the tumor in the tail of the pancreas infiltrating the splenic vein; (B) dissection of the transverse mesocolon. The arrow indicates the inferior mesenteric vein; (C) placement of EndoGrab; (D) dissected tumor; the arrow indicates the splenic vein infiltrated by the tumor.
Under general anesthesia, the patient was placed supine decubitus in the French position. After extensive lavage of the navel, access to the abdominal cavity was performed through a transverse transumbilical incision measuring 2.5cm. A SILS port device (Covidien Ltd., Norwalk, CT, USA) was inserted, large enough for two 5-mm and one 12-mm trocars. Subsequently, pneumoperitoneum was created with carbon dioxide at a pressure of 14mmHg. Through one of the 5-mm trocars, rigid 30° optics were introduced (Olympus Ltd., Hamburg, Germany), providing direct visualization for the insertion of the two remaining trocars. Through the free 5-mm trocar, roticulator-grasper forceps were inserted (Roticulator™ Endo Dissect™, Covidien Ltd., Norwalk, CT, USA) and held in the left hand of the surgeon. The 12-mm trocar was used to insert the remaining instruments. The patient was placed in an anti-Trendelenburg position and right lateral decubitus to facilitate the exposure of the pancreas.
The first step was to dissect the inferior side of the pancreas, accessed through the left transverse mesocolon, just below the inferior mesenteric vein (Fig. 1B). To do this, we used a LigaSure Advance® 5mm (Covidien Ltd., Norwalk, CT, USA). This maneuver allowed us to assess the infiltration of neighboring structures before any irreversible maneuver was performed and to continue with single-port surgery safely.
Afterwards, we sectioned the gastrocolic ligament to access the lesser sac and ligate the short vessels of the spleen. To facilitate the exposure of the pancreas and the tumor, we used an EndoGrab® device (Virtual Port Ltd., Caesarea, Israel), which was anchored on one side to the posterior gastric body and on the other to the anterior abdominal wall. With this maneuver, the pancreas was fully exposed.
We then located the celiac trunk and splenic artery. Gently, an outline was created of a retropancreatic tunnel above the splenic artery and vein at the junction of the head with the body of the pancreas, which was completed with the Goldfinger dissector.
Thus, we found sufficient space to perform the pancreatic resection with a 60-mm roticulator-endostapler (EndoGIA roticulator, Covidien Ltd., Norwalk, CT, USA) with a reinforced purple load covered with Seamguard absorbable material (WL Gore & Associates, Flagstaff, AZ, USA).
Finally, the splenic vein was ligated with a 45-mm roticulator endostapler loaded with white staples, as was the splenic artery at the celiac trunk. The tail of the pancreas and spleen were mobilized, and the surgical specimen was extracted in a 15-mm Endocatch II Specimen Pouch (Covidien Ltd., Norwalk, CT, USA) through the transumbilical incision.
The closure of the fascia was done with Maxon loop 1/0 and the skin with Vicryl Rapide 2/0 sutures.
It was not necessary to insert drain tubes. Total operative time was 140min and blood loss was minimal, at just barely 35cc. The final incision after removal of the surgical specimen measured 3.4cm.
The postoperative period was uneventful. The patient began a liquid diet on the first day post-op and progressed to a fat-free diet on the second day. The patient was able to walk independently on the first day post-op and was discharged on the second day. The pathology study showed the presence of a well-differentiated endocrine tumor with a maximum diameter of 6cm, with no infiltration of the resection margins.
Currently, multiple studies report the superiority of laparoscopic surgery in DP when compared to open surgery and demonstrate lower morbidity and shorter hospital stays.10 Therefore, whenever possible, minimally invasive surgery should be our first choice when faced with DP.
Recently, there has been growing interest in single-port surgery in various diseases.4–6 However, single-port distal pancreatectomies are not common surgeries due to the technical difficulties involved. Such difficulties can be more manageable with the development of new surgical instruments, along with extensive experience in laparoscopic surgery. Furthermore, in order to perform this technique with guarantee, patients should be appropriately selected. Lesions larger than 5cm should be assessed since it will probably be necessary to extend the incision to be able to remove the surgical specimen.7
We believe that single-port DP is a promising technique that will be able to be performed with guaranteed safety and efficacy in coming years, provided that patients are properly selected and referred to hospitals with high-level performance in advanced laparoscopic surgery with single-port experience.
Please cite this article as: Morales-Conde S, Rubio-Manzanares M, Alarcón I, Barranco A, Socas M. Esplenopancreatectomía corporocaudal por puerto único. Cir Esp. 2013;91:541–543.