The prevalence of adrenal incidentalomas is increasing with the ageing of the population and the use of high resolution imaging techniques. Current protocols propose a comprehensive monitoring of their functional and morphological state, but with no conclusive clinical evidence that endorses it.
MethodRetrospective study of 96 patients diagnosed with adrenal incidentaloma between 2008 and 2012. We evaluated clinical, functional, and imaging at baseline and during follow-up.
ResultsInitially, 9 cases were surgically removed: 4 due to hyperfunction (2 Cushing syndromes and 2 pheochromocytomas) and 5 due to size larger than 4cm. During follow-up one case of pheochromocytoma was diagnosed and another grew more than 1cm, needing surgery. In 98.86% of nonfunctional and benign lesions, there were no functional and/or morphological changes in the final evaluation.
ConclusionsThe results of our study challenge the validity of current diagnostic–therapeutic protocols of incidentalomas, which should be reassessed in prospective studies taking into account efficiency characteristics.
La prevalencia de los incidentalomas suprarrenales está aumentando por el envejecimiento de la población y el empleo de técnicas de imagen de alta resolución. Los protocolos actuales proponen un seguimiento de su estado funcional y morfológico exhaustivos, sin una evidencia clínica concluyente que lo avale.
MétodoEstudio retrospectivo de 96 pacientes diagnosticados de incidentaloma adrenal entre 2008 y 2012. Se evalúan características clínicas, funcionales y de imagen, basales y durante el seguimiento.
ResultadosInicialmente, 4 casos fueron intervenidos por hiperfunción (2 síndromes de Cushing y 2 feocromocitomas) y 5 por tamaño superior a 4cm. Durante el seguimiento, tan solo se diagnosticó un caso de feocromocitoma y otro creció más de 1cm, indicándose cirugía. En el 98,86% de los incidentalomas diagnosticados inicialmente como benignos y no funcionantes, no se objetivaron modificaciones funcionales y/o morfológicas en la evaluación final.
ConclusionesLos resultados de nuestra serie cuestionan la validez de los protocolos de seguimiento de los incidentalomas adrenales vigentes en la actualidad, que deberían ser revaluados atendiendo a características de eficiencia mediante estudios prospectivos.
An adrenal incidentaloma (AI) is a mass with a diameter larger than 1cm, discovered unexpectedly in an imaging test performed on a patient not suspected to have any adrenal disease. The strictest definitions exclude patients undergoing imaging tests as part of an extension or follow-up study for cancer.1 Its prevalence increases with age: less than 1% in young subjects, 3% in subjects in their 50s, and more than 15% in people older than 70 years.2,3 This incidence has greatly increased in recent years, probably in relation to the widespread use of high-resolution imaging tests and the progressive ageing of the population.
The initial management of these lesions should be focused on ruling out hormonal hypersecretion and/or malignancies susceptible to surgical treatment.4 However, most cases consist of benign non-functioning lesions for which the follow-up recommendations are controversial. Both the lack of prospective trials and the high financial and emotional costs incurred by patients question the current exhaustive recommendations for the assessment and follow-up of adrenal incidentalomas.
The objective of this study was to analyse the diagnostic–therapeutic strategies used in our field and to assess the usefulness of the evaluation and follow-up protocols for adrenal incidentalomas with an initial benign diagnosis and normal hormonal function.
Materials and MethodsA retrospective, descriptive study was conducted on 96 patients diagnosed with adrenal incidentaloma who were seen at the outpatient Endocrinology unit of Hospital Universitario Puerta del Mar de Cádiz [Puerta del Mar University Hospital of Cádiz] from 2008 to 2012. Those patients with active cancer in the last 5 years were excluded.
The epidemiological and anthropometric variables, the metabolic comorbidities and the morphological and functional characteristics at the time of diagnosis of incidentaloma and during its follow-up were collected.
Urinary free cortisol (electrochemiluminescence, Roche Diagnostics, Mannheim, Germany), catecholamines (high performance liquid chromatography, Chromsystems GMBH, Gräfelfing, Germany), and 24-h urine metanephrines (high performance liquid chromatography, Chromsystems GMBH, Gräfelfing, Germany) were determined in all patients. Plasma cortisol (electrochemiluminescence, Roche Diagnostics, Mannheim, Germany) after 1mg of nocturnal dexamethasone, corticotropin (IRMA, DIAsource ImmunoAssays, Louvain, Belgium), and the cortisol secretion circadian rhythm were assessed in those cases with urinary free cortisol above the upper limit of normal. The serum aldosterone and the plasma renin activity (PRA) (radioimmunoassay, Beckman Coulter, Marseille Cedex, France) were measured only in patients with hypertension and/or hypokalemia.
The diagnosis of subclinical Cushing syndrome was established in the absence of clear symptoms of hypercortisolism but with at least two positive screening tests (urinary free cortisol above the upper limit of normal, loss of the circadian rhythm, plasma cortisol following inhibition with 1mg of dexamethasone >1.8¿g/dL).5
Hydrocarbonate metabolism abnormalities were defined according to the criteria proposed by the American Diabetes Association6 and high blood pressure was defined when values exceeded 140/90mmHg or a hypotensive treatment was prescribed. Obesity was considered when body mass index (BMI) was ≥30kg/m2, and osteoporosis when T-score was <−2.5 SD by bone densitometry.
The coding and analysis of data were performed with the statistical SPSS programme version 15.0 for Windows. The quantitative variables were expressed by mean±SD, median and range. The Student's t-test was used for the comparisons among groups and the Wilcoxon test was used to compare the maximum diameter. The qualitative variables were expressed by percentages and were compared by chi-square test. The statistical significance was considered in all cases for P-values <.05.
ResultsOut of the patients studied, 55.2% were males, with a mean age of 61.38±12.2 years and a BMI of 29.66±4.9kg/m2. Sixty-six cases (70.2%) were detected by computerised tomography, 18 (19.1%) by magnetic resonance imaging and 10 (10.6%) by ultrasound. The reason why the imaging test was performed was: digestive disease in 17 cases (21%), a genitourinary test in 17 (21%), lung involvement in 12 (14.8%), vascular disease in 11 (13.6%), low back pain in 6 (7.4%), infectious or autoimmune disease in 6 (7.4%), and other reasons in 8 (14.7%).
In the baseline evaluation, 42 patients (43.8%) were overweight or obese, 49 (51%) had arterial hypertension, 32 (33.3%) dyslipidemia, 24 (25%) abnormal hydrocarbonate metabolism, and 20 (20.8%) osteoporosis.
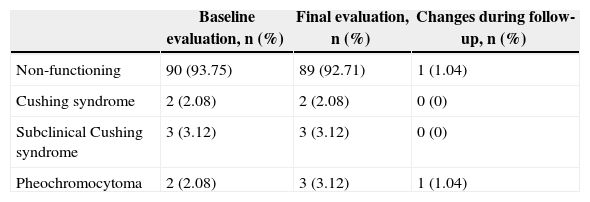
In the functionality study, 89 cases (92.70%) were catalogued as non-functioning. Two cases (2.1%) of Cushing syndrome and two cases (2.1%) of pheochromocytoma, which underwent surgery, were diagnosed. Three cases (3.12%) were diagnosed with subclinical Cushing syndrome based on a urinary free cortisol value above the upper limit of normal, plasma cortisol >1.8¿g/dL (none >5¿g/dL) following administration of 1mg of nocturnal dexamethasone and loss of the cortisol secretion circadian rhythm. None of those cases progressed to overt Cushing syndrome during follow-up.
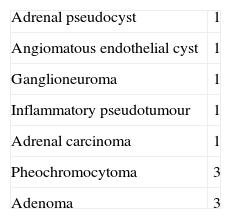
The radiological evaluation detected 46 (47.9%) incidentalomas in the left adrenal gland, 42 (43.7%) in the right adrenal gland, and 8 (8.4%) were bilateral. The mean size at the time of diagnosis was 26.6±20mm. Five patients (5.4%) were operated on due to a size larger than 4cm. The radiological characteristics of one of these cases (1.04%) indicated malignancy and the pathology examination confirmed an adrenal carcinoma.
The mean follow-up period was 31.21±18.1 months. In the next evaluation, 88 (98.87%) of the adenomas initially diagnosed as non-secreting tumours maintained their normal function; only one case of pheochromocytoma was diagnosed six months after the diagnosis (Table 1). The aldosterone/PAR ratio, which in two cases (6.12%) was >25, was measured in all patients with high blood pressure; no case of primary hyperaldosteronism was confirmed after the saline infusion test. Diagnoses at the end of the follow-up period are shown in Table 1. As for the morphological progression, no significant changes in size were observed: the difference between the maximum diameter at baseline and after 2 years was 0.56±2.3mm (P=.103). Only 1 case (1.08%) showed growth >1cm in 1 year: surgery was indicated and the pathology examination was consistent with an inflammatory pseudotumour. In summary, of the 96 adrenal incidentalomas included in the study, 11 (11.46%) underwent surgery: 5 for overt hyperfunction, 5 for size larger than 4cm and 1 for growth >1cm (Table 2).
Diagnosis of Functionality of Adrenal Incidentalomas.
| Baseline evaluation, n (%) | Final evaluation, n (%) | Changes during follow-up, n (%) | |
|---|---|---|---|
| Non-functioning | 90 (93.75) | 89 (92.71) | 1 (1.04) |
| Cushing syndrome | 2 (2.08) | 2 (2.08) | 0 (0) |
| Subclinical Cushing syndrome | 3 (3.12) | 3 (3.12) | 0 (0) |
| Pheochromocytoma | 2 (2.08) | 3 (3.12) | 1 (1.04) |
P=.68.
The increased demand of radiological tests performed for various reasons and the higher resolution power of imaging tests have exponentially raised the prevalence of incidentally discovered adrenal masses. As a result, adrenal incidentalomas represent a frequent reason for consultation, and adopting an adequate follow-up plan in clinical practice is paramount.
In our study, the frequency of non-functioning adenomas was 92.70% of the total of incidentalomas analysed. This prevalence is higher than those described in surgical or histological series, as well as in other clinical series that include patients with a history of cancer.7 On the contrary, the incidence of adrenal carcinoma (1.04%) was lower than in other series,8 probably in relation to the referral of potentially malignant lesions directly to surgical units.
Following the initial evaluation, the presence of subclinical Cushing syndrome was confirmed only in 3 cases (3.12%). No case progressed to overt Cushing syndrome and no new cases were diagnosed during follow-up. Although some studies support surgery,9 intervention was not chosen because the patients were older than 60 years, had diabetes and hypertension, were well-controlled on pharmacological treatment, and there was no evidence of the potential benefit that surgery would provide. The prevalence of subclinical cortisol hypersecretion reported in other series is significantly higher, between 5% and 20%,10 probably because the cortisol determination following 1mg of nocturnal dexamethasone has been systematically used; that test has higher sensitivity (close to 95%), but also a higher rate of false positive results.
As for the radiological characteristics, both the mean size (26.6mm) and the frequency of bilaterality (8.4%) coincide with the data published in other studies.11 Only 1 case showed growth >1cm during follow-up and it was a benign lesion. The risk for a lesion previously diagnosed as benign of becoming malignant is very low (<1/1000)12 despite its growth.
The optimal follow-up frequency and duration for patients with adrenal incidentalomas are uncertain. At present, most consensus and clinical practice guidelines recommend repeating the imaging tests at 6, 12 and 24 months (earlier if the phenotype is suspicious) and the hormone evaluation test (with the suppression test with 1mg of dexamethasone, catecholamines, and 24-h urine fractionated metanephrines) annually for 4 years.1,13 After a 2-year follow-up period in a prospective multicentre study including 226 cases of adrenal incidentalomas, the Adrenal Study Group of Western Sweden did not detect the development of malignancy or hypersecretion in any case initially diagnosed as benign and non-functioning; they recommended performing longer-term prospective studies to assess the profitability of the current recommendations.14 In this sense, in our series, 98.86% of the lesions initially diagnosed as benign and non-secreting remained without changes and only 1 case of pheochromocytoma was diagnosed in the first 6 months of follow-up. As for the morphological evaluation, when the baseline radiological image showed suspected malignancy, the suspicion was confirmed histologically; on the contrary, in the cases where the image suggested a benign tumour, the histological exam proved to be benign even though the lesions were operated on due their size or growth. Based on the absence of cost-effectiveness studies and the lack of long-term prospective studies, some authors have indicated that the current recommendations (prolonged follow-up with frequent visits and diagnostic tests) should be revised since they involve a significant financial cost, the potential risk of cancer induction due to repeated exposure to high doses of ionising radiation and the emotional impact derived from the high rate of false positive results.15,16
The main limitations of our study include its retrospective, observational design and the fact that it was conducted in a single site with a limited sample size. Additionally, only the cases seen in the outpatient Endocrinology unit were analysed, excluding the adrenal masses referred directly to the surgical units, where the prevalence of morbidity is potentially higher.
In conclusion, in our setting we did not detect significant changes in the size or in the long-term hormonal function of adrenal incidentalomas initially diagnosed as non-functioning. Consequently, we consider that the efficacy and efficiency of the systematic application of the currently recommended diagnostic, therapeutic and follow-up protocols should be reassessed with long-term prospective studies and a larger population.
Conflicts of InterestThe authors declare that they do not have any conflicts of interest.
The authors thank Doctor Ana Sáez-Benito Godino for her cooperation with the laboratory tests.
Please cite this article as: Mateo-Gavira I, Vilchez-López FJ, Larrán-Escandón L, Ojeda-Schuldt MB, López Tinoco C, Aguilar-Diosdado M. ¿Deberían modificarse los protocolos diagnóstico-terapéuticos de los incidentalomas suprarrenales? Cir Esp. 2015;93:30–33.
Information presented at congresses: part of the manuscript information has been presented as a poster presentation at the “16th International Congress of Endocrinology and 15th European Congress of Endocrinology”, held in Copenhagen, from 27 April to 1 May 2013.