Bariatric surgery improves sexual function in obese individuals, although the extent to which sexual satisfaction is improved following surgery is unknown. The aims of this study were (1) to describe sexual satisfaction in severely/morbidly obese men and women candidates for bariatric surgery; (2) to assess the effects of bariatric surgery on sexual satisfaction at 12-months follow-up; and (3) to assess whether weight changes at follow-up following bariatric surgery are associated with changes in sexual satisfaction.
MethodsWe conducted a prospective observational study from February 2011 to June 2014. A total of 44 patients with severe/morbid obesity participated in the study. Sexual satisfaction was assessed (at baseline and 12-months follow-up) through the Index of Sexual Satisfaction (ISS) questionnaire.
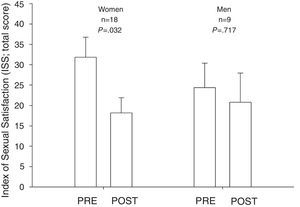
ResultsOf 44 patients who completed the ISS at baseline (mean age 40.3 [SD=9.4] years and BMI 46.9 [SD=6.2] kg/m2), 17 were lost to follow-up. The baseline ISS total scores were 32.0 (SD=20.1) in women and 24.4 (SD=16.0) in men (P>.05). The proportion of sexually satisfied men and women at baseline was 62.5% and 46.4%, respectively (P=.360). At follow-up, sexual satisfaction improved significantly in women (average difference 13.7 units; P=.032) but not in men (average difference 3.6 units; P=.717). The percentage of women with sexual satisfaction problems was reduced by 33% at follow-up (P=.038).
ConclusionsA relatively large percentage of severely/morbidly obese women and men present clinically significant sexual satisfaction problems before undergoing bariatric surgery. Sexual satisfaction improves significantly 12 months following bariatric surgery, particularly in women.
La cirugía bariátrica mejora la función sexual en pacientes obesos, aunque el alcance de mejora de la satisfacción sexual es desconocido. Los objetivos del estudio son 1) describir la satisfacción sexual en hombres y mujeres obesos severos/mórbidos candidatos a cirugía bariátrica; 2) valorar los efectos de la cirugía bariátrica en la satisfacción sexual a los 12 meses de seguimiento y 3) evaluar si los cambios en el peso tras el seguimiento se asocian con cambios en la satisfacción sexual.
MétodosEstudio observacional prospectivo desde febrero de 2011 hasta junio de 2014. Un total de 44 pacientes con obesidad severa/mórbida participaron en el estudio. Se valoró la satisfacción sexual (al inicio del estudio y tras 12 meses de seguimiento) a través del cuestionario del índice de satisfacción sexual (ISS).
ResultadosDe los 44 pacientes que completaron el cuestionario preoperatoriamente con una edad media de 40,3 años (DE = 9,4) y un IMC de 46,9 kg/m2 (DE = 6,2), 17 se perdieron durante el seguimiento. La puntuación total del ISS preoperatorio fue de 32,0 (DE = 20,1) en mujeres y de 24,4 (DE = 16,0) en hombres (p > 0,05). La proporción de hombres y mujeres con satisfacción sexual preoperatoria fue 62,5 y 46,6%, respectivamente (p = 0,360). Durante el seguimiento, la satisfacción sexual mejoró significativamente en mujeres (diferencia media de 13,7 unidades; p = 0,032), pero no en hombres (diferencia media de 3,6 unidades; p = 0,717). El porcentaje de mujeres con problemas de satisfacción sexual se redujo en un 33% tras el seguimiento (p = 0,038).
ConclusionesUn porcentaje relativamente amplio de mujeres y hombres obesos severos/mórbidos presentan problemas de satisfacción sexual antes de la cirugía bariátrica. La satisfacción sexual mejora significativamente tras 12 meses de seguimiento, sobre todo en mujeres.
Obesity represents a pathological process that has been exponentially increasing in recent years, becoming a pandemic with serious consequences for health.1,2 Severe and morbid obesity are linked to higher risk of diabetes and altered cardiovascular risk factors,3 as well as higher cardiovascular and all-cause mortality.4 Considering that obesity is both a physical (accompanied by different comorbidities and hormonal changes) and psychological disorder, the sexual life of obese (and particularly morbidly obese) patients can be significantly altered.5–7 In fact, a number of recent studies show a close relationship between obesity and sexual dysfunction.6,8,9
Previous studies show that, regarding the sexual sphere, obesity has greater negative consequences in women compared to men.5 Several studies have related the negative consequences of obesity in sexuality to the effect on the body image that obesity involves. In this sense, most studies have shown that women are more dissatisfied with their body image than men,10 which could result in a greater affectation of sexuality. Women might have suffered a higher social stigmatization regarding the deviations of the female normative or socially idealized body. This is also possibly starting to change for men. In fact, some studies have found that body image in men is related to masculinity,7 and recent studies show that men would have a double effect caused by body image (weight, and lack of bodybuilding and physical shape11,12).
The study of sexual satisfaction has gained relevance since, in 2002, the World Health Organization (WHO) included pleasure as a key factor of sexual health.13 Sexual satisfaction has been shown to be a major factor in individual sexual health, general well-being and quality of life.14 However, it is an aspect that has hardly been studied in people with obesity6 and there are no research studies using standardized questionnaires such as the Index of Sexual Satisfaction (ISS)15 to measure physical or emotional sexual satisfaction. In the few studies on this subject, either satisfaction is studied as a part of the sexual function, or through a single ad hoc question.7 However, sexual function and sexual satisfaction are different concepts. While sexual function is related to physiological concerns of sexual response, as Masters and Johnson stated in the 1960s,16 sexual satisfaction can be defined as the degree of satisfaction with the sexual aspects of a relationship,17 or a global appraisal of the quality of one's sex life.18 No single model of sexual response considers sexual satisfaction even when it is included in usual questionnaires to measure sexual function. As long as we consider sexual satisfaction separate from sexual response, it is important to evaluate it in obese patients before and after bariatric surgery.
In recent years, bariatric surgery has become the main treatment for patients with morbid obesity, with favorable results in the short and long terms in weight loss, associated comorbidities and quality of life.19–21 Several studies have reported that bariatric surgery leads to an improvement in the sexual sphere. Specifically in men, Dallal et al.22 found improvement in all sexual aspects after bariatric surgery. Importantly, weight loss partially explained this improvement in all sexual domains assessed. In women, most studies have shown improvements in all sexual domains measured by the Female Sexual Functioning Index (FSFI).23,24 There was only one study that did not report any changes in sexual desire and lubrication 6 months after surgery, and another that did not find any differences between pre- and postoperative measures.25 Some authors have raised the need for studies using global assessment measures of sexual satisfaction in various populations.26 Understanding how sexual satisfaction evolves in the obese patient following bariatric surgery is of clinical and public health interest. Nevertheless, to the best of our knowledge, no prior research has addressed this important topic.
The aims of the present study were (1) to describe sexual satisfaction in severely/morbidly obese men and women before bariatric surgery; (2) to assess the effects of bariatric surgery on sexual satisfaction at 1-year follow-up; and (3) to assess whether weight changes following bariatric surgery are associated with changes in sexual satisfaction.
MethodsWe conducted a prospective observational study from February 2011 to June 2014 in which sexual satisfaction, as well as all the studied variables were measured at baseline (the day before bariatric surgery) and 12 months after surgery. The local Ethics Review Board reviewed and approved the study protocol.
A total of 60 patients with severe/morbid obesity were initially invited to participate in the study. Before the surgical procedure, all patients were evaluated by a multidisciplinary team composed by endocrinologists, nutritionists, anesthesiologists, and surgeons to ensure that patients met inclusion criteria and the appropriateness of the intervention. The Bariatric Surgery Unit of a hospital in Southern Spain was in charge of surgery. The patients underwent either gastric bypass (GBP) or laparoscopic sleeve gastrectomy (LSG), depending on the protocol of the unit itself. The inclusion criteria for the study were: being candidate for bariatric surgery with a Body Mass Index (BMI)≥40kg/m2, or BMI≥35kg/m2 with associated comorbidities; age between 18 and 60 years; obesity maintained for more than 5 years; failure of other non-surgical treatments to treat obesity; signing of the informed consent to participate in the study.
On admission (the day before surgery), the patients were informed about the study aims and protocol and signed written informed consent. Thereafter, they were given several questionnaires through personal interview undertaken by a previously trained nurse.
Sexual satisfaction was assessed at baseline and 12-month follow-up through the Spanish version of ISS.27 It is a questionnaire designed to measure the degree of satisfaction in sexual intercourse. The questions are answered on a Likert scale ranging from 1 (never) to 5 (always). It consists of 25 items and a score ranging from 0 to 100. A total score ≤30 indicates satisfaction with sexual life, while a total score >30 suggests the possibility of a clinically significant problem. This questionnaire has been previously used14,15,27 showing good psychometric properties (Cronbach alpha of 0.8927). In the Spanish version, the questions were inverted in order to measure satisfaction, rather than dissatisfaction as the original did. In our study, we kept the original order to be able to conveniently use the cut-off points raised by the authors. The original instrument has an internal consistency reliability (Cronbach's alpha) ranging from 0.86 to 0.9515,27 and a test-retest reliability equal to 0.93 after an interval of one week.27 In addition, it shows adequate evidence of discriminant validity, since it detects differences between people with and without sexual problems, and construct validity due to its relationship with sexual desire, marital satisfaction, depression, self-esteem, double sexual morality15,27 and sexual functioning.28
Among the variables studied were age, gender, marital status, weight, BMI, waist-to-hip ratio (WHR), comorbidities, type of surgery, intra- and postoperative complications and percentage of excess BMI loss (%EBMIL).
Following the surgery a methylene-blue test was performed at 24h and, if the results were negative, the patient received a liquid diet to assess their tolerance. The patient was discharged between 48 and 72h after surgery. All patients received a semi-liquid diet during the first four postoperative weeks and were evaluated at outpatient clinics at 1, 3, 6, and 12 months after surgery. A regular follow-up was also maintained by contact with the nutrition team.
Statistical AnalysisNormality of baseline BMI and sexual satisfaction was checked through histogram and the Shapiro Wilk test. Sociodemographic and clinical baseline characteristics, including baseline levels of sexual satisfaction (objective 1) are presented as mean (standard deviation; SD) for quantitative variables, and number and percentage for categorical variables (e.g. sexual satisfaction if ISS total score ≤30 or sexual satisfaction problems if ISS total score >30). We compared sexual satisfaction (i.e. the total score of the ISS questionnaire) by sex using linear regression adjusted for age and marital status. As there is evidence of sex-related differential effects of obesity on sexual function, and there were sex-related differences in the ISS total score at baseline, we assessed the effects of bariatric surgery on sexual satisfaction at 1-year follow-up (objective 2) separately for men and women. We performed repeated-measures analysis of covariance after adjustment for age and marital status. Additionally, we assessed the odds of presenting a clinically relevant problem regarding sexual satisfaction (ISS total score >30) at 1-year follow-up (in comparison to baseline) using logistic regression adjusted for age and marital status. To assess whether %EBMIL following bariatric surgery is associated with changes in sexual satisfaction (objective 3), linear regression was performed.
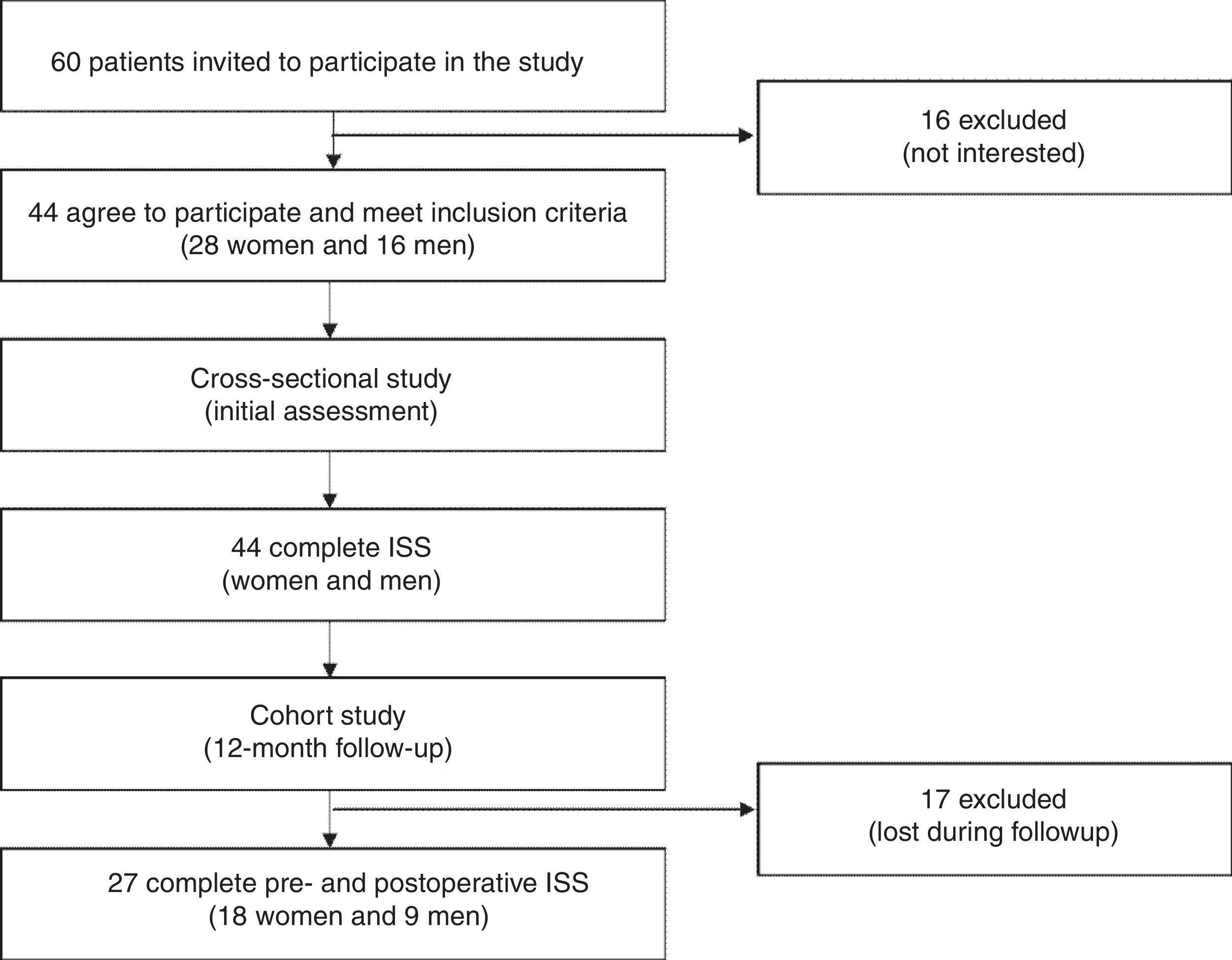
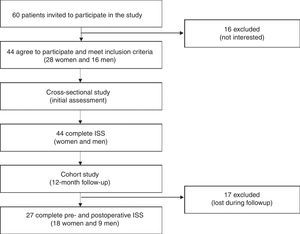
ResultsA total of 60 patients underwent surgery between February 2011 and June 2014, and were invited to participate in the study. However, 16 of these patients were not interested in participating. All of the remaining 44 patients (28 women and 16 men) met the criteria and were finally included in the study (Fig. 1). Of the 44 patients who completed the ISS at baseline, 17 were lost to follow-up.
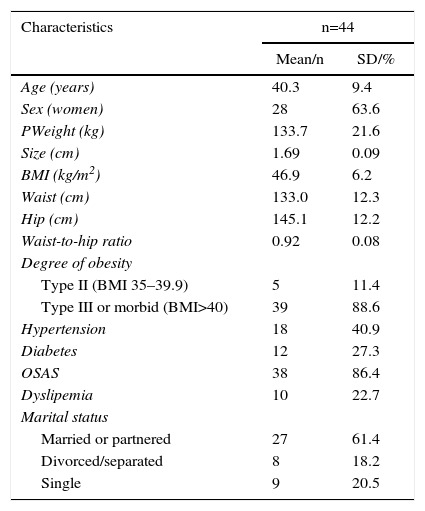
Sociodemographic characteristics are shown in Table 1. The mean age was 40.3 years, the average weight was 133.7kg, and the BMI was 46.9kg/m2. The main associated pathologies were obstructive sleep apnea syndrome (OSAS) (86.4%), hypertension (HTN) (40.9%), and diabetes mellitus (DM) (27.3%). 61.4% of the sample were married or with a steady partner, 20.5% were single, and 18.2% were separated or divorced. The procedures performed were 20 GBP and 24 LSG. No intraoperative complications were observed. During the postoperative period, one patient presented bleeding that required surgical revision to control (by heat sealing) small-vessel bleeding. After 12-month follow-up, the mean BMI was reduced to 31.7kg/m2 (P<.001). The %EBMI was 73.2% (36.78%–107.1%). Regarding the associated pathology, there was a significant reduction in OSAS (7.4%; P<.001) and dyslipidemia (3.7%; P<.001). The number of patients with HTN was reduced by 7.4% (P=.016) and DM by 11.1% (P=.125).
Baseline Characteristics of Patients With Severe/Morbid Obesity Who Are Candidates for Bariatric Surgery.
| Characteristics | n=44 | |
|---|---|---|
| Mean/n | SD/% | |
| Age (years) | 40.3 | 9.4 |
| Sex (women) | 28 | 63.6 |
| PWeight (kg) | 133.7 | 21.6 |
| Size (cm) | 1.69 | 0.09 |
| BMI (kg/m2) | 46.9 | 6.2 |
| Waist (cm) | 133.0 | 12.3 |
| Hip (cm) | 145.1 | 12.2 |
| Waist-to-hip ratio | 0.92 | 0.08 |
| Degree of obesity | ||
| Type II (BMI 35–39.9) | 5 | 11.4 |
| Type III or morbid (BMI>40) | 39 | 88.6 |
| Hypertension | 18 | 40.9 |
| Diabetes | 12 | 27.3 |
| OSAS | 38 | 86.4 |
| Dyslipemia | 10 | 22.7 |
| Marital status | ||
| Married or partnered | 27 | 61.4 |
| Divorced/separated | 8 | 18.2 |
| Single | 9 | 20.5 |
SD, standard deviation; BMI, body mass index; OSAS, obstructive sleep apnea syndrome.
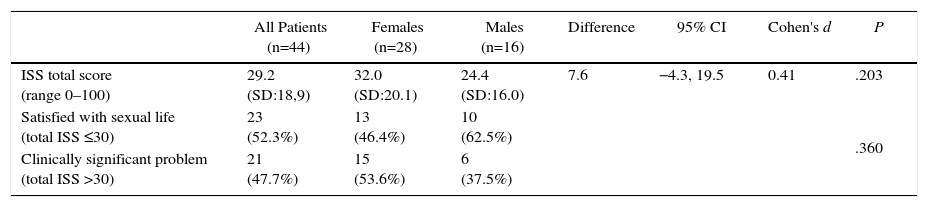
Before bariatric surgery (baseline; objective 1), the average sexual satisfaction was 32.0 (SD=20.1) units in women and 24.4 (SD=16.0) in men (P>.05). 54% of women and 36% of men presented a clinically relevant problem (ISS total score >30 units) at baseline (P>.05; Table 2).
Index of Sexual Satisfaction (ISS) in Men and Women Who Are Candidates for Bariatric Surgery.
| All Patients (n=44) | Females (n=28) | Males (n=16) | Difference | 95% CI | Cohen's d | P | |
|---|---|---|---|---|---|---|---|
| ISS total score (range 0–100) | 29.2 (SD:18,9) | 32.0 (SD:20.1) | 24.4 (SD:16.0) | 7.6 | −4.3, 19.5 | 0.41 | .203 |
| Satisfied with sexual life (total ISS ≤30) | 23 (52.3%) | 13 (46.4%) | 10 (62.5%) | .360 | |||
| Clinically significant problem (total ISS >30) | 21 (47.7%) | 15 (53.6%) | 6 (37.5%) |
SD, standard deviation; CI, confidence interval; Cohen's d, standardized mean difference; ISS, Index of Sexual Satisfaction.
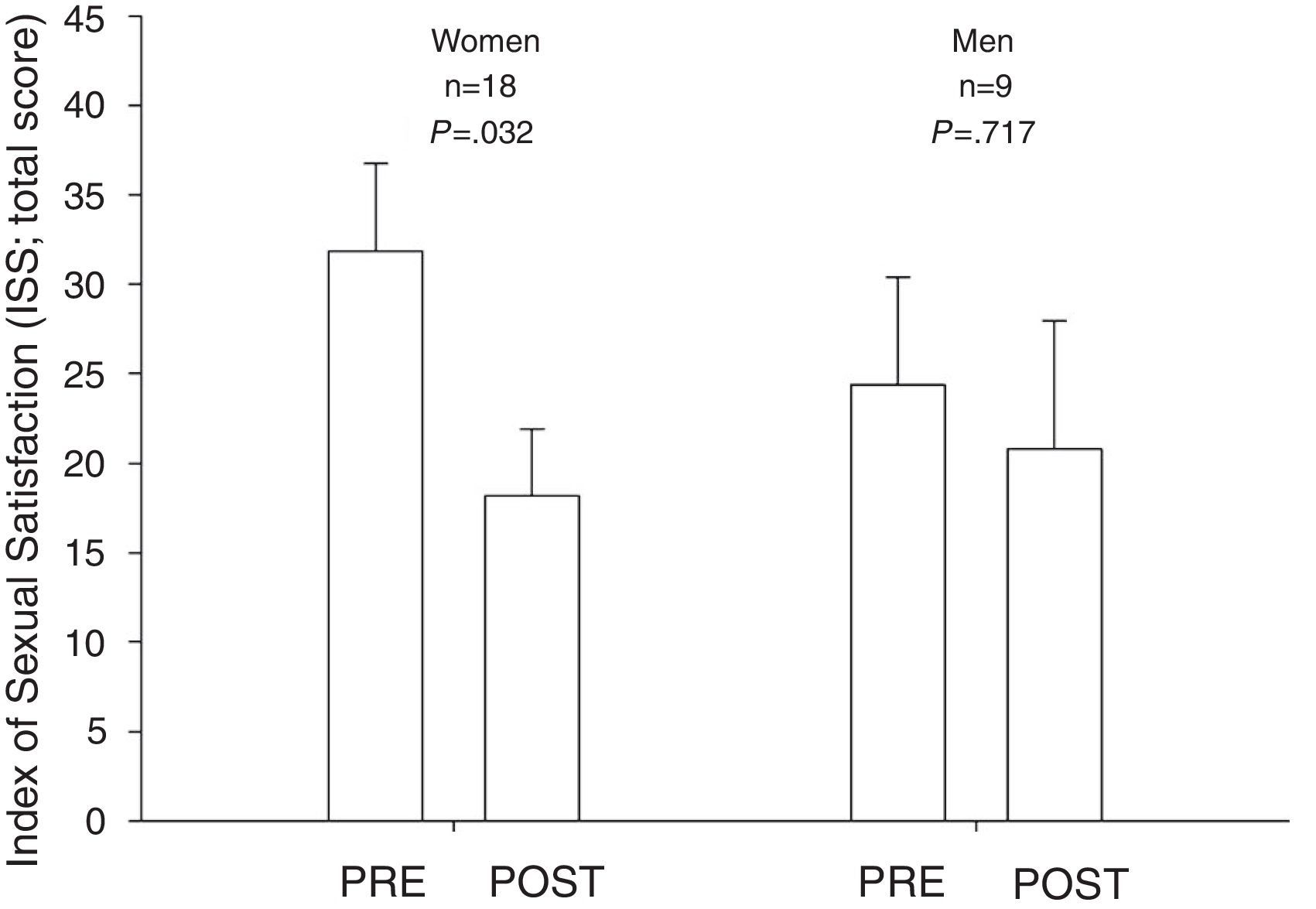
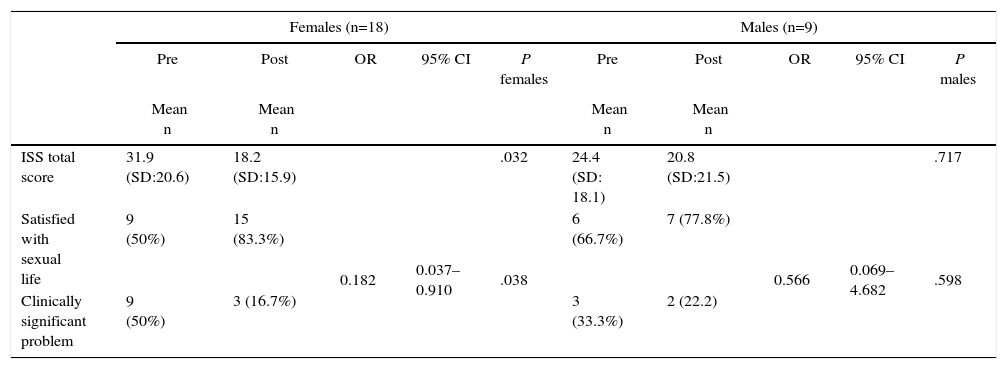
The effects of bariatric surgery on sexual satisfaction at 1-year follow-up are presented in Table 3. At 12-month follow-up, a significant reduction of the ISS total score (i.e. −13.7 units) was observed in women (P=.032). The odds of presenting a clinically significant sexual satisfaction problem was 81.8% lower at 12-month follow-up compared to baseline (P=.038). Among men, an improvement was also observed in the ISS total score (i.e. -3.6 units), although it was not statistically significant (Fig. 2).
Changes in the Index of Sexual Satisfaction (ISS) in Patients With Morbid Obesity 12 Months Following Bariatric Surgery.
| Females (n=18) | Males (n=9) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | OR | 95% CI | P females | Pre | Post | OR | 95% CI | P males | |
| Mean n | Mean n | Mean n | Mean n | |||||||
| ISS total score | 31.9 (SD:20.6) | 18.2 (SD:15.9) | .032 | 24.4 (SD: 18.1) | 20.8 (SD:21.5) | .717 | ||||
| Satisfied with sexual life | 9 (50%) | 15 (83.3%) | 0.182 | 0.037–0.910 | .038 | 6 (66.7%) | 7 (77.8%) | 0.566 | 0.069–4.682 | .598 |
| Clinically significant problem | 9 (50%) | 3 (16.7%) | 3 (33.3%) | 2 (22.2) | ||||||
ISS, Index of Sexual Satisfaction; SD, standard deviation; OR, odds ratio.
The association of %EBMIL following bariatric surgery with changes in sexual satisfaction (objective 3) did not reach statistical significance (B=−0.59; SE=0.34; 95% CI −1.32 to 0.14; P=.106).
DiscussionTo the best of our knowledge, this is the first study examining the effects of bariatric surgery on sexual satisfaction over a 1-year follow-up using a validated questionnaire. The main findings of the present study indicate that a relatively high percentage of severely/morbidly obese women and men present clinically significant problems regarding sexual satisfaction before undergoing bariatric surgery. Importantly, at 12-month follow-up there is a significant improvement in sexual satisfaction, particularly in women. Weight changes were not associated with changes in sexual satisfaction, although further research is warranted.
Sexual dysfunction in obese patients is a common and complex disorder that can significantly affect the patients’ quality of life.23 Steffen et al.29 and Bond et al.24 observed that women attribute their lack of sexual activity mainly to feeling tired, uninterested or not having a partner, whereas men attribute it mainly to physical difficulties. Several factors have been associated with sexual dysfunction such as depression and related medication, physical problems and a large number of obesity-related comorbidities (cardiovascular diseases, HTN, DM…).23,29
Over recent years, several articles that assess changes in sexual function after bariatric surgery, mainly in women, have been published. Thus, Janik et al.30 studied a series of 153 women, who underwent LSG or GBP, that answered the questionnaires (FSFI and Sexual Quality of Life–Female [SQoL-F]) by e-mail (20% response rate) versus a preoperative control group of 23 patients (85% response rate). The desire and arousal domains were significantly higher in the experimental group (P<.01). Nevertheless, the other domains showed no differences. Bond et al.24 followed 54 women after bariatric surgery (GBP and gastric banding), who completed the FSFI questionnaire in the preoperative period and after 6-month follow-up. Before surgery, 63% of the women presented an indicative score of sexual dysfunction and, after 6 months, this dysfunction was resolved in 23 of the 34 patients (68%). In the regression analysis, being young (P=.012), married (P=.036), and with a worse sexual function in the preoperative period (P<.001) were associated with a greater increase in sexual function. Assimakopoulos et al.8 assessed sexual function using the FSFI questionnaire which patients completed one week before surgery and one year later. They included 60 patients (98.3% response rate), who showed statistically significant differences after follow-up: sexual desire (P=.005), arousal (P=.001), lubrication (P=.003), sexual satisfaction (P=.012) and total sexual function (P=.003). Efthymiou et al.9 found a significant improvement in all domains of sexual function (assessed using the FSFI questionnaire) following a 1-year follow-up after surgery.
In the same way, several studies assessed the response to surgery in male sexual function. Thus, Sarwer et al.31 present a cohort of 32 male patients following GBP whose sexual function was assessed using the International Index of Erectile Function (IIEF) questionnaire. The patients showed improvement in all subscales following surgery. However, there were no statistically significant differences. These results support those published by Ranasinghe et al.,32 who reported in a retrospective study on 36 male patients who underwent laparoscopic adjustable gastric banding (LAGB) that 83.3% of the patients reported erectile dysfunction preoperatively. Nevertheless, no improvement was found in the total score of the IIEF questionnaire despite weight improvements (P=.96). Other authors,9 however, did find improvement after bariatric surgery using the same questionnaire. As we can observe, the results of bariatric surgery on sexual response in men's case are not as consistent as in women.
Different studies have shown that sexual function and sexual satisfaction are not conceptually the same.26,33 In fact, there are people who seek sexological consultation because of sexual function problems who may show adequate levels of sexual satisfaction. Psychological factors such as distress caused by sexual dysfunction, rather than the alteration itself, could explain this phenomenon.33 Others have shown that sexual satisfaction may not be a reflection of physiological function, depending on factors such as expectations about the normal or ideal sexual functioning level and beliefs about aspects related to sexual and intimate experiences.26 Therefore, it is important to assess sexual satisfaction specifically and independently of sexual function.
Sexual satisfaction, which is a key factor in sexual health and general well-being, has been widely studied in the general population.26 Several studies have related obesity to sexual dissatisfaction in both women and men. In women, there are studies finding a positive relationship between sexual health, sexual satisfaction and all body image measurements.33 Sexual satisfaction was predicted by body self-esteem and low frequency of distracting thoughts related to physical appearance during sexual intercourse.33 Women with low satisfaction may benefit from treatments that specifically address aspects related to body image, such as bariatric surgery. In relation to men, Carr et al.34 found lower sexual satisfaction compared to those with normal weight.
Our results showed that, prior to surgery, women were more affected than men, as the average ISS score in women (32 units), but not in men (24 units), indicated a clinically relevant problem regarding sexual satisfaction, as it surpassed the limit of 30 units. Sexual disatisfaction includes loss of pleasure in sexual activity, loss of desire, difficulties in sexual intercourse and avoidance of sexual encounters.23 Our results may also support those who argue that women are still today more affected by body-image demands (an aspect that has been clearly related to sexual satisfaction).20 In this sense, there are also studies showing that women are more dissatisfied with their body image than men, and that body image correlates negatively with BMI, especially in women.10 In the case of men, some studies show that being a male increases the probability of having a positive body image and, in turn, being sexually satisfied. This would agree with our results,10 rather than those which do not find differences in sexual satisfaction according to gender.11
Importantly, our results indicate that at 12-month follow-up, the percentage of sexual dissatisfaction decreased significantly by 33% in women, which might reflect the improvements in sexual function as reported by others.8 The magnitude of this improvement was not the same in men, although sexual dissatisfaction diminished by 11.1%. These sex-related differences in sexual satisfaction improvements following bariatric surgery may be related to the previously reported improvements in sexual function in women,31 whereas there is more controversy in men.9,31
Another interesting, although surprising, finding of the present study indicates that weight reduction (%EBMIL) following bariatric surgery was not associated with improvements in sexual satisfaction either in women or men. Therefore, it is potentially possible that other factors might explain the sexual satisfaction improvements observed in women after bariatric surgery. Among these factors, improvements in body image or perceived intimacy with partner could partially explain the results observed in this study. As the sample size was relatively low, these results cannot be ascertained and further research with larger sample size is needed.
The findings of this exploratory study extend current knowledge about the effects of bariatric surgery on sexual satisfaction, which is a relevant aspect associated with quality of life of the obese patient. In addition, our results will lead to future research on the effects of bariatric surgery on sexual health (including longer follow-up periods) and the factors explaining the benefits in sexual satisfaction observed, particularly in women, at follow-up.
This study has limitations that must be underlined. The sample size was relatively small and, consequently, some analyses might have been underpowered to detect significant effects. For instance, the association of %EBMIL with improvements in sexual satisfaction showed a potential trend that should be examined in future studies with larger sample sizes. Loss to follow-up was also a challenge, as a relatively large number of participants were not willing to respond to the questionnaire at follow-up. Potential reasons for not completing the questionnaire at follow-up (despite having participated at baseline) involve differential motivations before and 1 year after surgery. This might have led to participation bias. However, we undertook ancillary analysis to find out whether participants lost to follow-up differed from participants completing the study at baseline, and there were no appreciable differences (data not shown). It must be taken into account that sexual behaviors are still a “taboo” topic in our society. Therefore, future studies should make efforts to ensure conditions to encourage response (e.g. ensure privacy, perhaps by means of online anonymous surveys, doctors highlighting the importance of understanding sexual issues, etc.). In addition, there was no homogeneity in the surgical techniques employed in this study, which induced differential weight loss and hormonal changes that can affect sexual behavior. Future studies should consider these issues.
In conclusion, a relatively large percentage of severely/morbidly obese women and men present sexual satisfaction problems before undergoing bariatric surgery. Sexual satisfaction improves significantly 12 months following bariatric surgery, particularly in women. Weight loss was not significantly associated with improvements in sexual satisfaction. However, further research with larger samples is warranted to confirm or contrast these findings.
Conflict of InterestThe authors declare that they have no competing interests.
These authors contributed equally to this work.
Please cite this article as: Ferrer-Márquez M, Pomares-Callejón MÁ, Fernández-Agis I, Belda-Lozano R, Vidaña-Márquez E, Soriano-Maldonado A. Satisfacción sexual tras cirugía bariátrica: estudio observacional prospectivo. Cir Esp. 2017;95:521–528.