Due to the increase in breast-conserving surgery with adjuvant radiotherapy for the treatment of early-stage breast cancer, there has also been an increase in the incidence of radio-induced sarcomas.1 Angiosarcomas are malignant tumors derived from the vascular endothelium. Presentation in the breast can be primary or secondary to radiotherapy. Radiation-associated angiosarcoma (RAAS) is seen in primary breast cancer patients treated with breast-conserving surgery and radiotherapy. By definition, it is histologically different from the initial tumor requiring radiation. The recorded prevalence is 0.05% and incidence is 0.16%.2 The risk of developing RAAS of the breast is greater in the first 5–10 years after radiotherapy,3 while other radiation-associated sarcomas usually present more than 10 years afterwards.
The clinical course of the angiosarcoma depends on the tumor grade. A low tumor grade exhibits an indolent, insidious behavior similar to that of atypical vascular lesions,4 while a high-grade angiosarcoma is a highly aggressive tumor with explosive growth and local recurrences within a few months of radical resection. Poor histological differentiation is a negative prognostic factor for patients affected by angiosarcomas, and low-grade tumors can transform into high-grade angiosarcomas. Multifocality (appearance of two or more tumors post-radiation that are not contiguous, synchronous or metachronous, with or without identical histology, in the field of a cancer treated with radiation therapy) is usually seen in up to 30% in RAAS of the breast and even more frequently when more time has passed between radiotherapy and the development of the secondary cancer.5
We present the case of a patient who was treated surgically in 2005, at the age of 44, for breast cancer in the upper external quadrant of the left breast, involving breast-conserving surgery and axillary lymph node dissection. The pathology study identified invasive ductal carcinoma, pT1 pN0, estrogen receptors 90% (+++), progesterone receptors 30% (++) and negative HER2 (luminal A). After the procedure, the patient received radiotherapy (50Gy over the entire breast and a tumor bed boost of 10Gy) followed by treatment with tamoxifen. During follow-up, no metastatic lesions or lymphedema were detected.
In April 2012, the Dermatology Department surgically removed a dark red skin nodule from the lower internal quadrant of the left breast. The pathology diagnosis was epithelioid angiosarcoma, grade III. Upon examination in our Unit, we observed skin lesions that were erythematous/violet in appearance and affected both lower quadrants of the left breast, together with the scar from the described exeresis. Palpation detected no nodules or other signs of locoregional recurrence. Mammography identified no signs of malignancy. Surgical treatment was indicated, consisting of simple mastectomy with extensive skin exeresis and immediate reconstruction with a dorsal muscle-skin flap. The histopathology study detected multiple foci of varying sizes (some microscopic) of well-differentiated angiosarcoma (grade I) in an area of 4cm in diameter, with involvement of the skin and subcutaneous tissue. The surgical margins were tumor-free (Fig. 1).
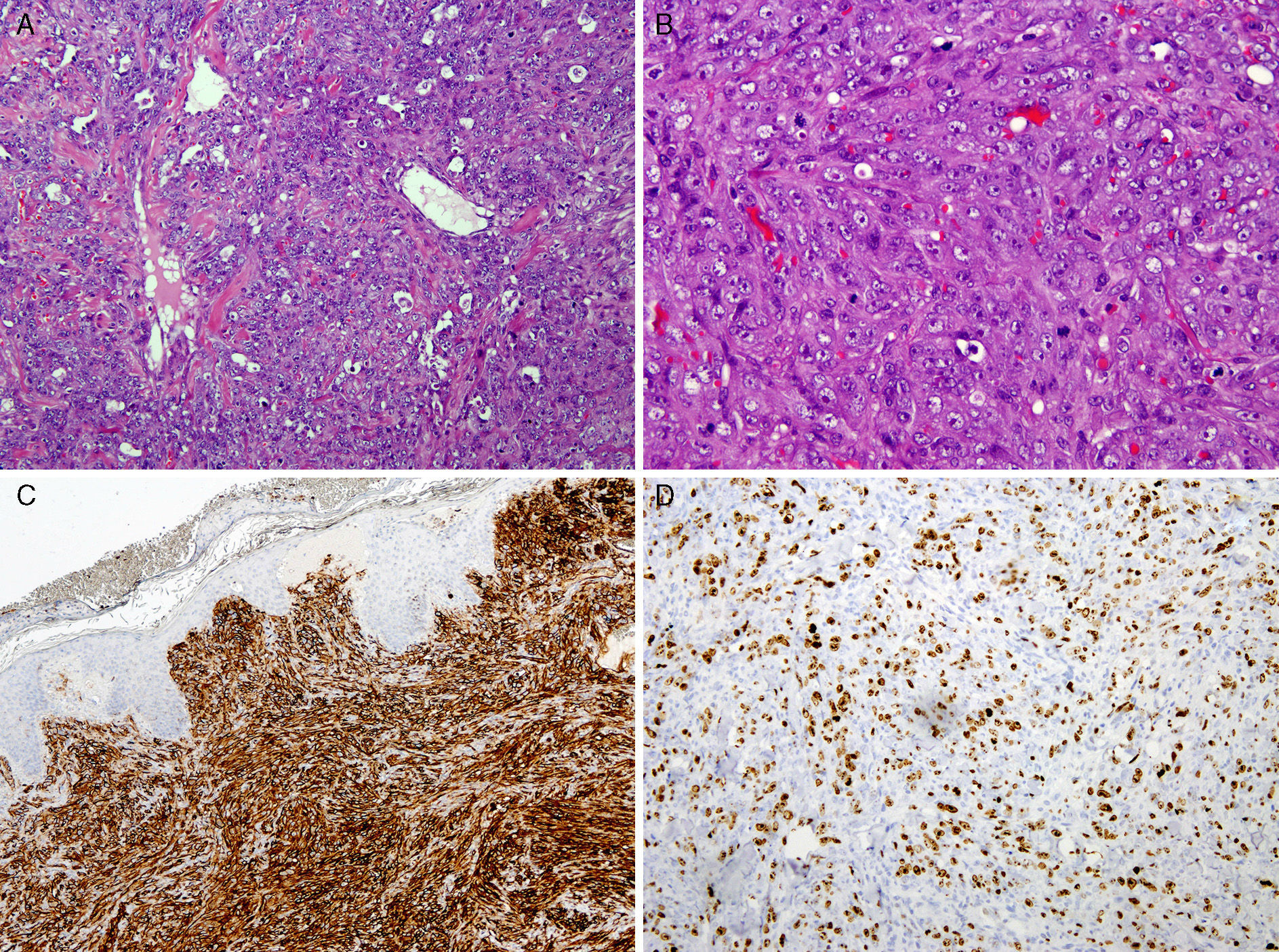
Anatomic pathology study of the mastectomy specimen: (A) epithelioid pattern of the tumor (H&E x4); (B) red blood cells are observed inside some cells, and there is a high number of mitoses per field (H&E x10); (C) immunohistochemistry CD-31+ demonstrates the vascular origin; (D) Ki-67, high proliferation rate, typical of the nature of high histology grades.
After one month, circumscribed dark red macules appeared on the cutaneous island of the reconstructive flap, with no invasion of the remaining radiated skin from the inferior pole (Fig. 2). Given the patent's history, the lesions were removed with a wide margin; these were identified as well-differentiated angiosarcoma (grade I), with foci that had no continuity, one of which was 12mm in the dermis and another subcutaneous lesion measuring 3mm (immunohistochemistry: CD31+; Ag factor VIII+, CD34+ and Ki67: 45%).
Because of the aggressive local behavior, we extended the excision to 15cm×7cm around the area, with removal of part of the flap (skin, subcutaneous tissue and muscle), periprosthetic capsule and much of the remaining radiated skin. The results were negative for neoplastic infiltration. Currently, after 6 months of follow-up, the patient has presented no local recurrence or systemic disease.
The case we present is interesting due to its atypical development, with the evolution of secondary angiosarcoma from high grade to low grade, while early multifocal recurrence was low grade, circumscribed in the post-mastectomy reconstruction flap, but with no involvement of the radiated area or the mastectomy scar.
In conclusion, RAAS appears after a mean of approximately 7 years as a consequence of radiation therapy after breast-conserving surgery of a tumor with a different histology, typically high-grade, with a skin rash being the main symptomatic sign,6 although other presentations are possible7 (patches, papules or red-purple nodules with irregular surfaces, which are not painful and are frequently surrounded by satellite lesions, with a variable presence of skin changes, such as discoloration, erythema or edema). They usually develop in the center of the radiation field, which is the area that receives the maximum radiation of 50Gy. Radical surgery (simple/radical modified mastectomy, or extensive local excision) is the treatment of choice; it is sometimes associated with chemotherapy regimens based on anthracyclines and, more recently, taxanes, in order to obtain a safety margin of at least 3cm. Local recurrence and distant metastasis are common, even if the cancer is low-grade.8
Early detection is very important for survival. Therefore, patients with previous radiation treatment who present with suspicious vascular cutaneous lesions should be biopsied in order to rule out this pathology.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Navarro Cecilia J, Jiménez Anula J, Luque López C, Martín Salvago MD, Dueñas Rodríguez B. Angiosarcoma secundario de mama: recidiva multifocal en colgajo autólogo utilizado en la reconstrucción. Cir Esp. 2015;93:260–262.