Surgery is the only potentially “curative” therapy for pancreatic cancer, which is still the most lethal gastrointestinal neoplasia.1,2 Unfortunately due to its rapid and insidious growth for years it has been highly unresectable.1
It is estimated, therefore, that around 80%–90% of cases are inoperable at the time of diagnosis, because they are locally advanced and/or metastatic, and they have an overall survival (five years) of 5%, rising to 25% in those susceptible to oncological resection.3
Although there is consensus that curative surgery is not feasible in the case of infiltration of the coeliac trunk or the superior mesenteric artery, there is less agreement about other forms of locally advanced disease.
In fact, over the past few decades, the concept of resectability has evolved and there is a tendency to take a more ambitious and individualised approach in tackling this typically aggressive tumour biology.
Therefore, benefits in selected patients have now been documented with respect to neoadjuvant chemo-radiotherapy.4 In this regard, comparable overall and disease-free survival has been noted between initially and secondarily resected neoplasias as long as free margins are achieved. Indeed, in some cases, paradoxically, it has been higher in the second group (20 compared to 33 months average survival).1
However, the therapeutic strategy adopted by different groups with experience in second-look pancreatic cancer surgery varies considerably; from the most conservative policies (MSKCC) in which re-exploration is only considered when there are at least partial responses with a priori curative possibility (R0), to the policy of the University of Duke where they indicate re-laparotomy as long as there is no portal thrombosis or arterial involvement, and to the policy promoted by Massucco et al. who consider resection not only in the case of partial regressions, but also in the case of stable disease with normalisation of tumour marker levels, assuming down-staging.4–6
In any case, resectability rates in secondary surgery vary between 42% and 100%, and survival rates of between 20.5 and 33 months have been documented in these cases, between 1.5 and 6 years in series comprising various tumour types.1
Furthermore, the involvement of the mesenteric-portal venous axis, which is not uncommon in light of the close link between the pancreatic head and the uncinate process with the superior mesenteric vein and artery, is a clear example of this evolution.7,8 Considered inoperable with curative intent for years, numerous authors and at least twelve series in the literature, attest to an increase in the resectability of these cases, with partial vascular exeresis, which is feasible and safe performed by experienced surgeons, with mortality rates of 0%–7.7% and morbidity of 16.7%–54%, and with no substantial differences with respect to resections with no portal- mesenteric involvement.1,4,7,8
It is also worth noting that it is a priority to correctly distinguish between infiltration per se and peri-tumoural adherences/fibrosis, especially at the mesenteric-portal and retro-portal lamina level, particularly when there has been adjuvant treatment beforehand (chemo-radiotherapy).4
The following is the case of a 40-year-old patient with a history of DMID and ulcerative colitis; an abdominal ultrasound was requested due to hypertransaminasaemia, which detected an SOL in the head of the pancreas.
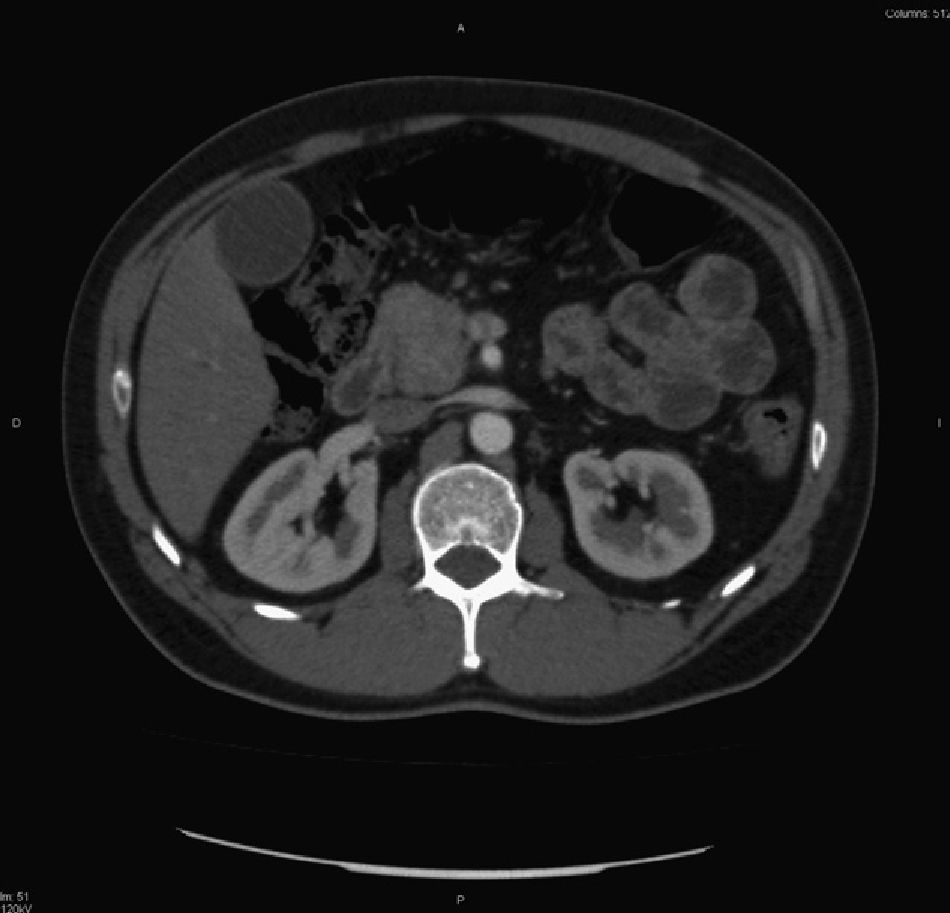
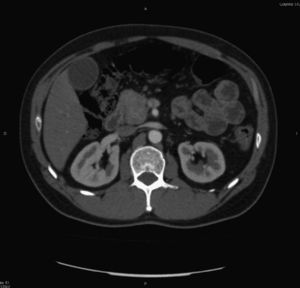
The study was completed using CT/MRI which revealed a 38mm×40mm neoplasia in the head of the pancreas, with ectasia of the duct of Wirsung and retrograde dilatation of the bile duct, with significant adenopathy and no apparent infiltration of the mesenteric-portal axis (Fig. 1).
A multidisciplinary assessment was made and cephalic duodeno-pancreatectomy was suggested. Surgical exploration revealed a large tumour compromising the pancreatic head, body and tail. Mercadier's method was impossible due to widespread infiltration of the mesenteric-portal vessels. The diagnosis of adenocarcinoma was confirmed by intra-operative biopsy and, as it was unresectable, the decision was made not to proceed.
The patient was assessed by Oncology, and received five cycles of chemotherapy, Folfirinox scheme.
Significant tumour involution was observed, and second-look surgery was agreed.
Total duodeno-pancreatectomy and splenectomy were performed, clamping and section of portal vein and superior mesenteric and vascular reconstruction with 8mm Gore-Tex prosthesis creating the relevant mesenteric/portal anastomosis (total clamping time 60min) and reestablishing transit with a Braun-type hepaticojejunostomy/transmesocolic jejunostomy/gastrojejunostomy/jejuno-jejunostomy.
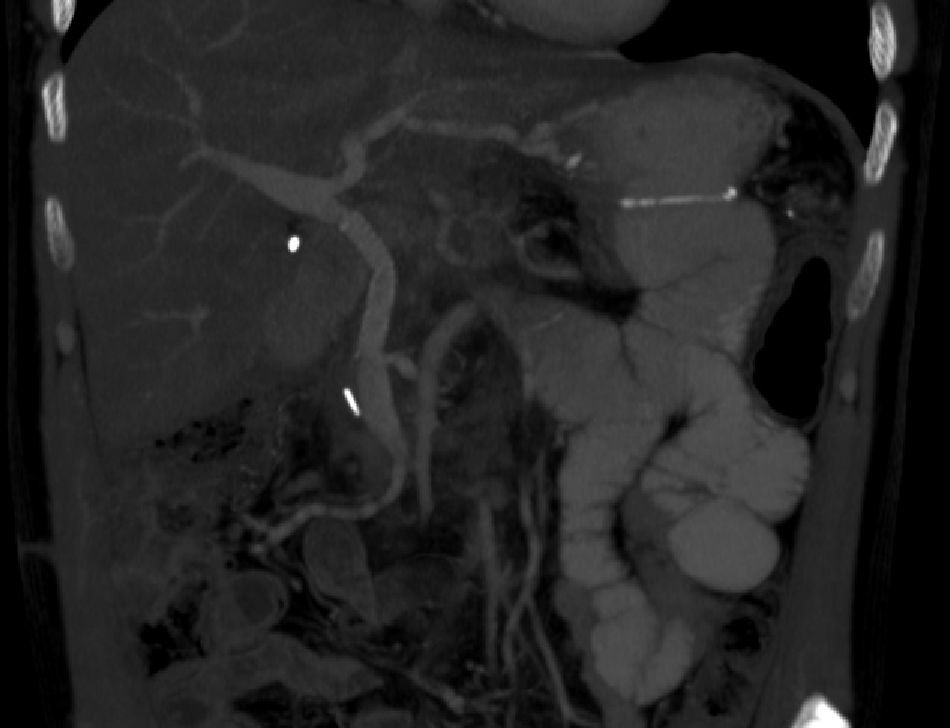
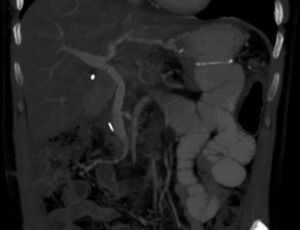
While the patient was hospitalised, the correct permeability and functioning of the portal prosthesis was checked by means of Doppler ultrasound and at present, twelve months after initial surgery and with pathology reporting of R0 resection and absence of malignant cells, the patient is undergoing capecitabine/gemcitabine chemo-radiotherapy on an outpatient basis with no evidence of disease (Fig. 2).
To conclude, we note the promising results in terms of resectability/survival achieved with neaodjuvant oncological treatment and rescue surgery3 such as in the case described here, an even better prognosis having been confirmed for tumours which, initially borderline, were subjected to a protocol of chemo-radiotherapy/prior to a second look in the case of downstaging/stable disease with a reduction in markers.4
Therefore, pending randomised studies providing scientific evidence, we consider that a multidisciplinary committee should assess and agree management strategies for pancreatic neoplasias at the limit of resectability and establish rescue criteria (second-look surgery) to identify patients who could benefit from this ambitious approach.1
As an added limitation, we end by highlighting that although there are data of similar morbidity and mortality rates with respect to conventional resection in resectable cases, this is certainly highly demanding and extremely difficult surgery which requires expert qualified specialists.4
Please cite this article as: Gómez García ME, Carbonell Castelló F, Alberola Soler A, Poves Gil PM, García Espinosa R. «Second-look» en adenocarcinoma de páncreas inicialmente irresecable tras quimioterapia neoadyuvante. Cir Esp. 2013;91:683–685.