Calcifying fibrous tumour (CFT) is a very rare benign soft tissue lesion1,2. The most common site is the gastrointestinal tract, with very few documented cases of retroperitoneal CFT in the literature3–5. We present a case of retroperitoneal CFT involving the inferior vena cava (IVC) and right renal vein (RV).
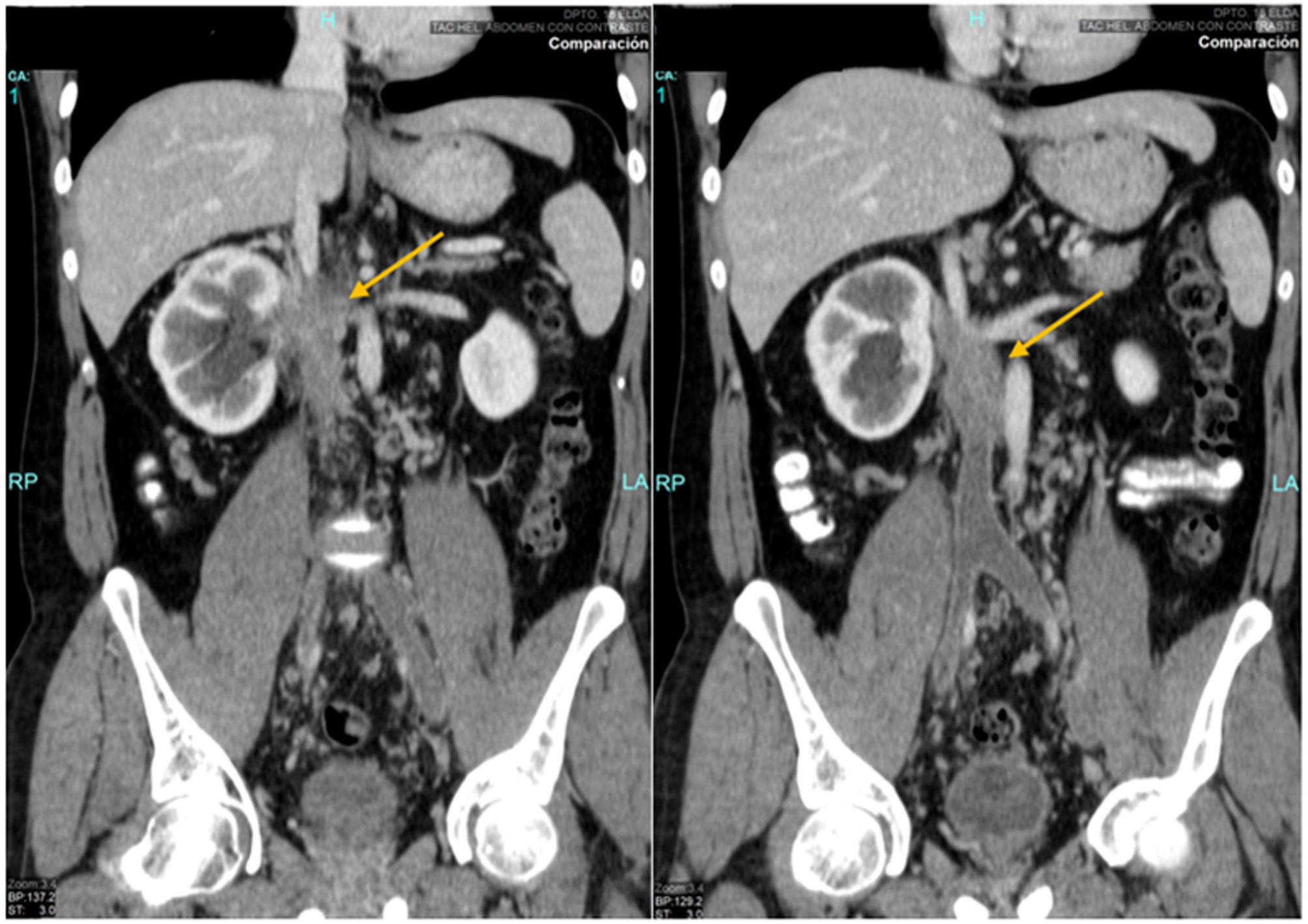
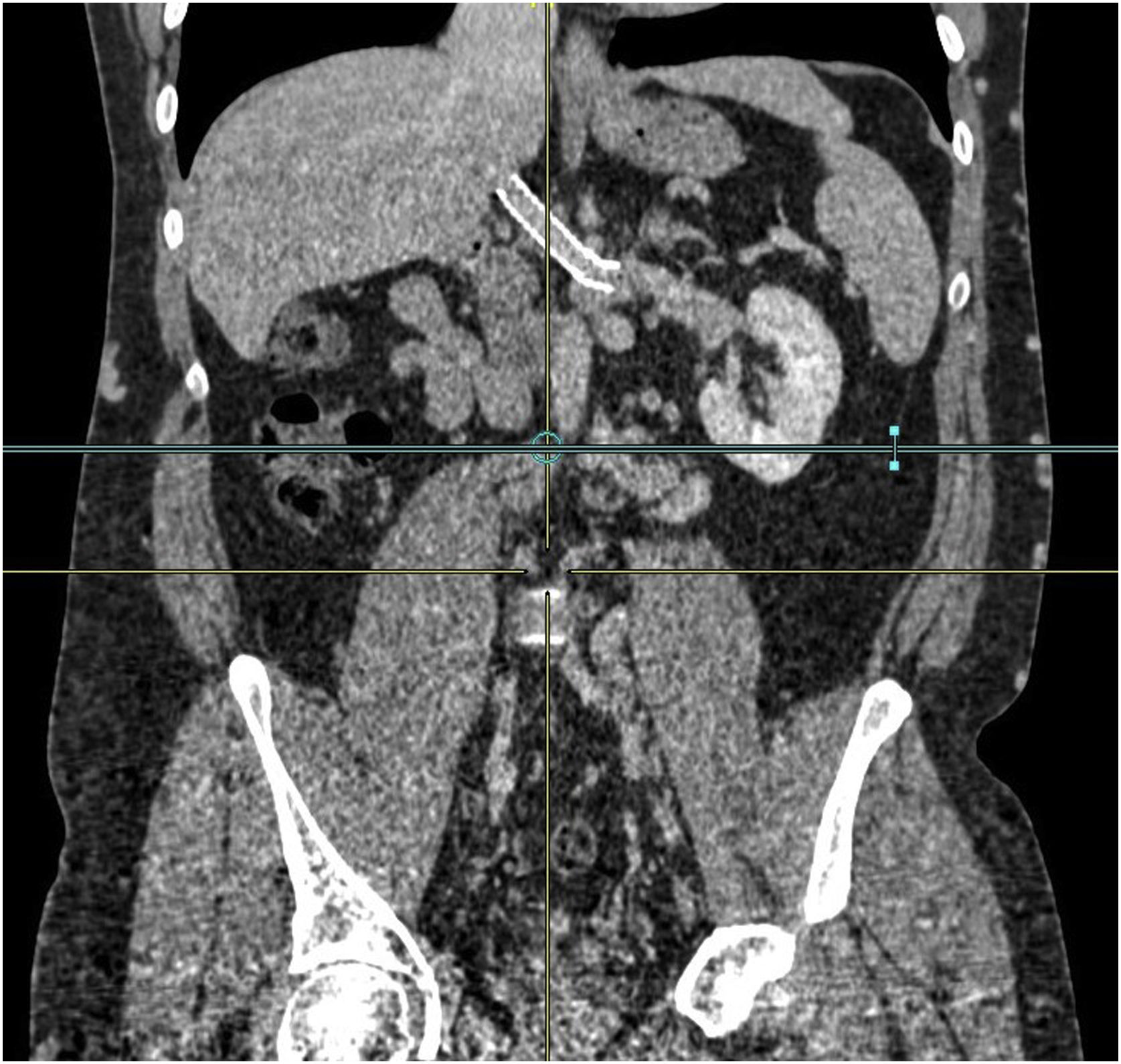
A 31-year-old male presented with paraesthesia in the left lower limb. Of note was an increase in CRP (24.18 mg/dL) and leukocytosis (14,400). Doppler ultrasound was performed, showing obstruction of the femoral, saphenous, and popliteal veins. A thoraco-abdominal-pelvic computed tomography (CT) scan was performed (Fig. 1) showing a tumour with enhancement and irregular margins (9 × 3 cm) at the level of the right renal hilum with involvement of the IVC and right RV, causing complete thrombosis of the IVC up to the infrarenal level, external and common iliac veins (IV). More than 90° contact with the aorta and third duodenal portion. Multiple retroperitoneal and right perirenal venous collaterals were observed (Fig. 2).
Given the suspicion of a possible sarcoma in the IVC, a biopsy was not performed due to the risk of bleeding and surgical intervention was decided. Via a mid-laparotomy, after the Cattel and Kocher manoeuvre, no duodenal involvement was observed. After complete control of the IVC (supra and intratumoural), left RV and IV, the IVC was sectioned above the bifurcation of the IV. After thrombectomy of both IVs, no significant venous flow was observed, and as there were retroperitoneal and subcutaneous collaterals, the stump of the IVC was sutured. The suprarenal IVC and left RV were sectioned and the tumour, IVC and right kidney were excised en bloc. Reanastomosis was performed of left RV to suprarenal IVC with “cone” cavoplasty.
Histology revealed a whitish tumour measuring 11 × 4.5 cm at the level of the renal hilum, benign and mesenchymal in appearance. It showed hypocellular fibroblastic proliferation and hyalinised stroma, variable chronic inflammation and occasional dystrophic calcifications, compatible with CFT. Immunohistochemistry showed positivity for vimentin, alpha-actin, desmin and local positivity for CD34.
Postoperatively, the patient presented persistent haematuria and a CT scan was requested, showing an absence of adequate flow from the left RV to the IVC with preferential drainage to the gonadal vein and pelvic and retroperitoneal venous congestion. Phlebography showed no evidence of thrombosis, but confirmed inadequate flow, and therefore an expandable stent was placed in the IVC and an uncoated metallic stent in the left RV, normalising venous return (Clavien IIIA). After making good progress, the patient was discharged on the ninth day. Currently, after six years, he has post-thrombotic syndrome of the lower limbs and subcutaneous venous collateral circulation, with good kidney function.
CFT was first described in 1988 by Rosenthal and Abdul-Karim as “childhood fibrous tumours with psammoma bodies”6. Fetsch et al. described 10 cases in 1993, using the term “calcifying fibrous pseudotumour”7. The WHO eventually established the term “calcifying fibrous tumour” in 2002.
It has been associated with IgG4 multiorgan lymphoproliferative syndrome, with increased plasma IgG4 and infiltration of different tissues have been observed in some cases1,2,8. The exact frequency is not known, but is estimated at one case/year worldwide. There is slight predominance in females (1:1,27) and trimodal distribution (0–4, 25–29 and 30–34 years)1.
The most common sites are stomach (18%), small intestine (8.7%), pleura (9.9%), neck, mesentery, mediastinum and peritoneum; it is less common in lower limb omentum, adrenal gland, back, lung and pericardium1. Multiple lesions may occur (5.7%)1. Our case is exceptional as only three articles have been published with a total of six cases of retroperitoneal CFT, only one case involving the IVC and no intravascular cases3–5.
Most cases are asymptomatic, with incidental diagnosis1,2. CT shows irregular and scattered calcifications delimiting the tumour1. MRI shows a hypointense signal on T1- and T2-weighted images and isointense on T1-weighted with gadolinium1. If vascular sarcoma is suspected, percutaneous biopsy is not indicated due to the risk of massive haemorrhage (.1%–8.3%), making it difficult to rule out malignancy preoperatively9.
Macroscopically it is a whitish, well-circumscribed, unencapsulated mass1,2. Microscopically it is a benign fibrous lesion with abundant densely hyalinised hypocellular collagen, with psammomatous or dystrophic calcifications and mononuclear inflammatory infiltrate, spindle cells and lymphoid aggregates1–3. Focal positivity for CD342 is always observed. The main differential diagnosis is inflammatory myofibroblastic tumour1,2.
Surgical excision is the main treatment1,2. The gold standard for an IVC sarcoma (primary suspicion in our case) is complete excision with free margins, including affected organs. The surgical challenge is the involvement of other organs, venous drainage of the liver, kidneys and lower extremities (LE) and reconstruction of the IVC9. In our case, the site of the lesion made for technically demanding surgery.
To manage the IVC, it is recommended that it is controlled above and below the tumour, at the level of the iliac bifurcation and suprarenal vena cava. When more than 75% of the IVC is occluded by the tumour, as in our case, it can be ligated for at least one year due to extensive venous collateral development. If the iliac bifurcation is not involved, the venous return of the LE is ensured by the internal iliac vein and the pelvic venous anastomoses9.
There is no medical treatment. The prognosis is excellent, long-term survival is 100%, with a recurrence rate of 9%–10%1. To conclude, CFT is a very rare benign tumour. We have only found one case of retroperitoneal CFT with severe involvement of the IVC in the literature. This site implies very complex surgery.
FundingNone.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Llopis-Torremocha C, Rodríguez-Laiz G, Sevila-Micó S, Campo-Betancourth CF, Ramia JM. Tumor fibroso calcificante retroperitoneal con afectación de vena cava inferior. Cir Esp. 2022;100:595–597.