Laparotomy is the standard approach for the surgical treatment of acute small bowel obstruction (ASBO).
Patients and methodsFrom February 2007 to May 2012 we prospectively recorded all patients operated by laparoscopy in our hospital because of ASBO due to adhesions (27 cases) and/or internal hernia (6 cases). A preoperative abdominal CT was performed in all cases. Patients suffering from peritonitis and/or sepsis were excluded from the laparoscopic approach. It was decided to convert to laparotomy if intestinal resection was required.
ResultsThe mean age of the 33 patients who underwent surgery was 61.1±17.6 years. 64% had previous history of abdominal surgery. 72% of the cases were operated by surgeons highly skilled in laparoscopy. Conversion rate was 21%. Operative time and postoperative length of stay were 83±44min and 7.8±11.2 days, respectively. Operative time (72±30 vs 123±63min.), tolerance to oral intake (1.8±0.9 vs 5.7±3.3 days) and length of postoperative stay (4.7±2.5 vs 19.4±21 days) were significantly lower in the laparoscopy group compared with the conversion group, although converted patients had greater clinical severity (2 bowel resections). There were two severe complications (Clavien-Dindo III and V) in the conversion group.
ConclusionsIn selected cases of ASBO caused by adhesions and internal hernias and when performed by surgeons highly skilled in laparoscopy, a laparoscopic approach has a high probability of success (low conversion rate, short stay in hospital and low morbidity); its use would be fully justified in these cases.
La laparotomía suele ser la vía de abordaje de elección en los casos de intervención quirúrgica por obstrucción aguda de intestino delgado (OAID).
Pacientes y métodosDe febrero 2007 hasta mayo 2012 se registraron prospectivamente los pacientes intervenidos de urgencias en nuestro centro vía laparoscópica por OAID por adherencias (27 casos) y/o hernia interna (6 casos). Todos disponían de una TC preoperatoria. Se excluyeron del abordaje laparoscópico aquellos con peritonitis y/o sepsis. En caso de requerir resección intestinal se convirtió a laparotomía.
ResultadosLa edad media de los 33 pacientes operados fue de 61,1±17,6 años. El 64% tenían antecedentes de cirugía abdominal previa. El 72% de los casos fue operado por un cirujano experto en laparoscopia. La tasa de conversión fue del 21%. El tiempo operatorio y estancia postoperatoria medios fueron de 83±44min y 7,8±11,2 días, respectivamente. El tiempo operatorio (72±30 vs 123±63min), día de inicio de ingesta oral (1,8±0,9 vs 5,7±3,3 día) y estancia postoperatoria (4,7±2,5 vs 19,4±21 días) fueron significativamente menores en el grupo laparoscopia respecto al de conversión, si bien los pacientes convertidos presentaron mayor gravedad clínica (2 resecciones intestinales). Hubo 2 complicaciones graves (Clavien-Dindo III y V) en el grupo de conversión.
ConclusionesEl abordaje laparoscópico, en casos seleccionados de OIDA por adherencias y hernias internas, cuando es realizado por cirujanos entrenados en laparoscopia, presenta una alta probabilidad de éxito (baja tasa de conversión, corta estancia postoperatoria y baja morbilidad), por lo que su uso estaría plenamente justificado en estos casos.
Acute intestinal obstruction (AIO) is a frequent reason for consultation in the Emergency Department, and in up to 76% of cases there is involvement of the small bowel (SBO).1 The most common cause is postoperative adhesions in 60%–80% of cases.1–4 Retrospective cohort studies have shown that, with a minimum follow-up of 10 years, around 35% of patients with prior abdominal or pelvic surgery by laparotomy are admitted at least once for an acute SBO episode.5 Approximately 29% of hospitalizations for SBO due to adhesions require emergency surgical treatment.6 Currently, laparotomy is the most commonly used approach in cases that require surgical treatment for this cause. Although there are sufficient data about the safety and utility of the laparoscopic approach in the treatment of acute SBO,1,7–9 the majority of general surgeons do not consider its use in standard clinical practice and apply it only in selected cases. According to American healthcare data, only 11.4% of SBO cases were treated laparoscopically in 2002.10
The aim of our study is to analyze the results of our series of patients who have been treated laparoscopically for acute SBO due to adhesions and/or internal mesenteric hernias.
Patients and MethodsStarting in February 2007, we prospectively registered all patients who were treated on an emergency basis with laparoscopy for SBO. The diagnosis of acute SBO was made based on the clinical history, physical examination and results of the different imaging tests (simple radiology and abdominal CT) of each patient. The approach used was chosen according to the personal criteria and experience of the surgeon treating the case at that moment.
Included in the SBO study groups were those patients whose final cause of the AIO was adhesions and/or an internal hernia associated or not with adhesions or defects in the mesentery. The adhesions were classified as simple or complex depending on whether they were caused by one single or multiple bands. They were also classified as either primary or secondary according to whether there was a previous history of any type of abdominal, pelvic and/or inguinal surgery. Following the same criteria, the internal hernias were considered either congenital or postoperative. In cases with suspicion of post-operative adhesions, we followed the protocol established in our center, which includes the administration of hydrosoluble oral contrast material, the placement of a gastric suction tube and sequential radiological monitoring according to the recommendations established by other groups.11 In all the patients who were operated on, informed consent was obtained for the laparoscopic approach and its possible conversion to laparotomy.
It was considered essential for the surgical team to have had experience in laparoscopic surgery. Patients with anesthesia contraindications for pneumoperitoneum, presence of clinical, analytical and/or radiological signs of peritonitis and/or severe sepsis were excluded from the laparoscopic approach. We also excluded from the analysis those patients who were treated surgically with laparoscopy for other causes of AIO, such as primary gastrointestinal neoplasm or peritoneal relapse of a previously known neoplasm, actinic enteritis, gallstone ileus, impacted foreign body or bezoar, intestinal invagination, as well as incarcerated incisional or inguinal-crural hernias.
Data were collected for age, sex, American Society of Anesthesiologists class (ASA), previous medical-surgical history, clinical and radiological presentation, surgery results (findings, procedure, surgical time) reasons for conversion and complications, date of start of diet, perioperative complications, length of hospitalization and mortality.
The surgical strategy (placement of the patient, monitor and sequential disposition of the placement of the trocars) was adjusted according to the characteristics of each patient. The most important determining factors for this were the suspected location of the cause of the obstruction and the number and type of previous abdominal incisions so that the first trocar was situated in an area far from previous incisions. In all the cases except one, the technique of choice for the pneumoperitoneum was the placement of a Hasson trocar. The optics used were 30°, and in none of the cases did the intra-abdominal pneumoperitoneum pressure exceed 12mmHg. When intestinal resection was necessary, we opted to create an assistance incision in all cases; this was considered a conversion to open surgery, regardless of the size. The surgeon was considered an expert in advanced laparoscopic surgery after having performed at least 50 complex procedures other than standard simple surgeries (cholecystectomy and appendectomy).
The statistical analysis for comparing the means between the laparoscopic and conversion groups was performed using the Mann–Whitney U non-parametric test for continuous variables and the chi-squared test for qualitative variables.
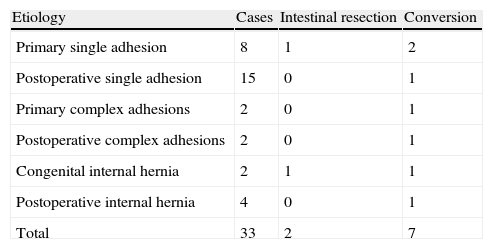
ResultsUp to May 2012, a total of 33 patients were included who had been operated on for acute SBO with laparoscopy due to adhesions or internal hernia, out of a total of 138 patients who had been treated surgically for SBO (24%). There were 18 men and 15 women, with a mean age of 61.1±17.6 (29–88). According to the ASA classification, 4, 21, 7 and 1 cases were grades i, ii, iii and iv, respectively. In all cases, preoperative abdominal CT had been performed, which was diagnostic for acute SBO. Table 1 shows the specific causes of SBO, the cases that required intestinal resection and the conversions to laparotomy. The overall conversion rate was 21%. Twelve patients (36%) had no history of previous surgery. Out of the patients with a history of previous surgery, 14 had been operated on only once, 2 twice, 4 three times and one on 6 occasions. Out of the 4 cases operated on for postoperative internal hernia, in 3 cases the previous surgery had been a laparoscopic gastric by-pass, and in one case hepatic-jejunostomy. In 24 cases, there was at least one expert surgeon in advanced laparoscopic surgery during the intervention.
Causes of Intestinal Obstruction According to Intraoperative Findings, Need for Intestinal Resection and Conversions to Open Surgery.
| Etiology | Cases | Intestinal resection | Conversion |
| Primary single adhesion | 8 | 1 | 2 |
| Postoperative single adhesion | 15 | 0 | 1 |
| Primary complex adhesions | 2 | 0 | 1 |
| Postoperative complex adhesions | 2 | 0 | 1 |
| Congenital internal hernia | 2 | 1 | 1 |
| Postoperative internal hernia | 4 | 0 | 1 |
| Total | 33 | 2 | 7 |
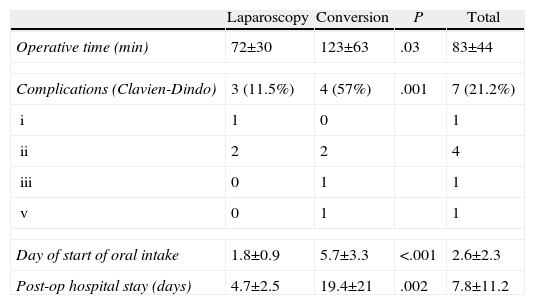
The causes for conversion were (Table 1): 2 cases due to intestinal ischemia that required intestinal resection, 2 cases due to unidentifiable causes (single adhesion), 2 cases due to complex adhesions (in one of these, the only intestinal perforation of the series occurred during the exploration maneuvers) and one case due to abdominal wall hemorrhage in a trocar orifice. Table 2 shows the results of the operative time, the day oral intake was initiated and postoperative hospital stay, both for the patients as a whole as well as broken down into total laparoscopy and conversion groups. In the postoperative period, mild complications (Clavien-Dindo I/II) were seen in 5 patients: 3 wound infections (2 trocar wounds and one conversion incision), one urinary tract infection (laparoscopy) and one paralytic ileus (conversion). Two patients of the conversion group presented serious complications (Clavien IV–V): one patient had a pelvic abscess that required surgical drainage, and one patient died on the 37th day post-op due to massive hemoperitoneum secondary to paracentesis in the course of a torpid postoperative recovery caused by complications unrelated to the surgical technique (severe renal failure and respiratory infection).
Overall Results and Differences Between Laparoscopic and Conversion Groups for Operative Time, Complications, Days Until the Start of Oral Intake and Postoperative Hospital Stay.
| Laparoscopy | Conversion | P | Total | |
| Operative time (min) | 72±30 | 123±63 | .03 | 83±44 |
| Complications (Clavien-Dindo) | 3 (11.5%) | 4 (57%) | .001 | 7 (21.2%) |
| i | 1 | 0 | 1 | |
| ii | 2 | 2 | 4 | |
| iii | 0 | 1 | 1 | |
| v | 0 | 1 | 1 | |
| Day of start of oral intake | 1.8±0.9 | 5.7±3.3 | <.001 | 2.6±2.3 |
| Post-op hospital stay (days) | 4.7±2.5 | 19.4±21 | .002 | 7.8±11.2 |
Out of the 105 patients operated on with the open approach, 22 required intestinal resection (21%). Mortality was 8.5% (9/105), which was 9.1% (2/22) and 8.4% (7/83) if they had required intestinal resection or not. Mean hospital stay of those with open surgery was 16.9 days.
DiscussionThe laparoscopic approach has been used more frequently in the management of acute SBO since Bastug12 published the dissection of a single band with this approach in 1991. Nonetheless, and even though different series have demonstrated that the laparoscopic approach is safe and effective in selected cases,1,9,13 the conversion rate is relatively low,9,10 and that patients benefit from shorter hospital stays, less postoperative pain and especially less postoperative morbidity3,14 and a reduction in the formation of possible new postoperative adhesions,15–18 the reality in daily practice is that there is still a low percentage of patients treated with this approach.10 The reasons are clear: difficult management and manipulation of the intestinal loops, which in these cases are distended and full of liquid; supposed risk of perforation during manipulation of the loops due to the increased friability of their walls; and difficult surgical field of vision due to less work space. In spite of this, the growing experience in laparoscopic surgery in all fields and improved surgical instruments have increased the percentages of cases treated with this method.1,8,9
There are no specific consensus guidelines on the indications of laparoscopic treatment in acute SBO; to date, no prospective, randomized studies have been published comparing the laparoscopic and conventional approach.1,8 The majority of the studies available are single-center and only 3 compile an experience of more than 100 cases.9,19,20 Some authors3,14 have published retrospective comparative studies of paired cases and controls. Most consensus guidelines used in the laparoscopic approach in emergency surgery show recommendation grades B and C for SBO.21–23 Keeping these deficiencies in mind, some papers and review articles24–26 propose a series of recommendations to choose the laparoscopic approach based on careful patient selection: (a) previous history of less than 2 laparotomies, because with more the conversion rate increases from 37 to 56%19; (b) less than 24h of evolution from the onset of symptoms and absence of any signs of peritonitis and/or sepsis; (c) incomplete obstructions; (d) history of previous surgery limited to a single abdominal quadrant; (e) moderate distension of intestinal loops; (f) definite preoperative diagnosis, based on CT findings, both of the obstructive cause (the most favorable are single bands and internal hernias) as well as their location.
The conversion rate published in the cases of laparoscopic approach in acute SBO ranges from 7% to 45%.2,4,10 O’Connor et al.,8 in a review of the literature that included 29 series and more than 2000 cases, showed an overall conversion rate of 36%, even though in cases of single adhesions this decreased to 27%. We feel that the main factor for the low rate of conversion of our series is attributable to the fact that 72% of the cases were treated by an expert surgeon in advanced laparoscopy. Depending on whether the intervention was done by an expert laparoscopic surgeon or not, the conversion rate was 12.5% or 44.4%, respectively. Although it could be attributed to an exquisite selection of cases, we do not feel this is true because the surgeon who completed the most procedures in the series (19/33) during the same period of time did not use laparotomy in any cases of SBO according to the conditions of the selection and exclusion criteria. The rate of conversion specific to this surgeon was 10.5% (2/19). These data confirm the conclusions suggested by other authors who consider the experience of the surgeon in laparoscopic surgery as one of the most important key factors for success.8
Elevated conversion rates have been related with higher morbidity and mortality.9,14,27 In our series, we have also confirmed this fact, although we do not attribute it to factors that directly depend on the surgical approach but instead on the intrinsic serious nature of the process and medical conditions of the patient. The causes that are frequently described as risk factors for conversion,8,9 including firm adhesions, no visualization of the site of the obstruction, intraoperative complications (fundamentally intestinal perforation) and the need to perform a laparotomy for intestinal resections, were also found in our study. In this context, we agree with the recommendation of not delaying conversion if the cause of the obstruction cannot be correctly visualized or in situations of prolonged manipulation of the loops in cases with complex adhesions.
Conventional surgical treatment of acute SBO by laparotomy is associated with high morbidity and prolonged postoperative hospitalization. Wullstein et al.,14 in their comparative study between the laparoscopic and conventional approaches, obtained significant differences in favor of laparoscopy in a lower rate of postoperative complications (19% vs 40%), faster recovery of peristaltism (3.5 vs 4.4 days) and shorter hospital stays (11.3% vs 18.1 days). In a similar study, Khaikin et al.3 reproduced the same results. In their population-based observational study about SBO treated with open surgery, Kössi et al.6 obtained a postoperative hospital stay of 11 days, and the mean operative time was 79min. In our series, the overall surgical time, including the cases of conversion, was comparable; meanwhile, the rate of postoperative complications, the day that oral intake was begun and postoperative hospital stay have been considerably less than those reported in the open approach (Table 2). Although the results that we have obtained are significantly better in the laparoscopy group compared to the conversion group, we do not feel they are comparable because the patients of the conversion group presented greater symptom severity (the 2 intestinal resections due to associated ischemia were from this group) as well as a greater likelihood of technical complexity (complex adhesions).
In conclusion, the laparoscopic approach in the surgical treatment of acute SBO due to adhesions and internal hernias seems not only safe and feasible in a high percentage of cases, but, also to present even better results when compared with the results published for the open approach. The careful selection of patients and the experience of the surgeon are crucial factors in order to obtain a low rate of conversion and success. In the absence of prospective and randomized studies, which are difficult to carry out due to the variability of the pathology being treated and location, we consider that the use of this laparoscopic approach is completely justified in the treatment of SBO, especially since its safety, utility and benefits have been demonstrated.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Poves I, Sebastián Valverde E, Puig Companyó S, Dorcaratto D, Membrilla E, Pons MJ, et al. Resultados del abordaje laparoscópico en el tratamiento de la obstrucción aguda del intestino delgado por adherencias y hernias internas. Cir Esp. 2014;92:336-340.