Despite the excellent results obtained with standard laparoscopic cholecystectomy, the efforts for minimizing the ports needed to reduce postoperative pain, for a quicker recovery and to improve the patient's cosmetics continue. The aim of this study is to report the results of the first 100 cases of single port laparoscopic cholecystectomy performed in a secondary care hospital.
Material and methodsProspective, observational and unicentric study including 100 patients between January 2010 and April 2012. Inclusion criteria: symptomatic cholelythiasis patients over 16 years of age on whom a single port laparoscopic cholecystectomy was performed. Exclusion criteria: history of acute cholecystitis, pancreatitis or suspected choledocholithiasis, Endoscopic retrograde cholangiopancreatography, BMI>35 and previous laparotomies. We studied epidemiological, surgical and safety variables.
ResultsThe mean patient age was 39.89±11.5 years. The mean time of the surgical procedure was 67.94±25.5min. There were 2 cases of postoperative complications: a non-infected seroma and a biliar leak. In 2 cases the use of an accessory trocar was needed. The mean hospital stay was 1.13±0.8 days. A total of 35% patients were included in the major ambulatory surgery program. The overall patient satisfaction survey rating showed a high level of cosmetic satisfaction in 100% of patients.
ConclusionsSingle port laparoscopic cholecystectomy is a good technique when performed in selected cases by expert surgeons. It is feasible to include the single port laparoscopic cholecystectomy in a major ambulatory surgery program. We have not had serious complications. There is a high cosmetic satisfaction index with this technique.
Aunque los resultados de la colecistectomía laparoscópica estándar son excelentes, se continúa intentando minimizar el número de puertos con el objeto de disminuir el dolor postoperatorio, conseguir una recuperación más temprana y mejorar el resultado estético del paciente. El objetivo de este estudio es presentar los resultados de los primeros 100 casos de colecistectomía por puerto único practicados en un hospital de segundo nivel.
Material y métodosEstudio prospectivo, observacional, unicéntrico. Se intervino a 100 pacientes entre enero de 2010 y abril de 2012. Criterios de inclusión: pacientes mayores de 16 años con colelitiasis sintomática operados por colecistectomía simple mediante incisión umbilical única. Criterios de exclusión: antecedentes de colecistitis aguda, colangiopancreatografía retrógrada endoscópica, pancreatitis o sospecha de coledocolitiasis, IMC>35 y laparotomías previas. Se estudiaron distintas variables epidemiológicas, quirúrgicas y de seguridad.
ResultadosLa edad media de los pacientes fue de 39,89±11,5 años. El tiempo quirúrgico medio fue de 67,94±25,5min. Presentaron complicaciones postoperatorias 2 pacientes: seroma y fuga biliar. En 2 casos fue necesaria la utilización de trocar accesorio. La estancia media fue de 1,13±0,8 días. El 35% de los pacientes fueron tratados en régimen de cirugía mayor ambulatoria. Todos los pacientes se mostraron muy satisfechos con el resultado estético.
ConclusionesLa colecistectomía mediante incisión umbilical única es una buena técnica cuando se utiliza en casos seleccionados y por cirujanos expertos. Puede facilitar la práctica de la colecistectomía en régimen ambulatorio. No se han presentado complicaciones graves. El índice de satisfacción estética es muy elevado.
Although standard laparoscopic cholecystectomy is the method of choice for the treatment of symptomatic cholelithiasis, new technological advances attempt to reduce the number of ports necessary in order to minimize postoperative pain, achieve earlier recovery and improve esthetic results.
During recent years, devices and instruments have been developed for single-port umbilical laparoscopic access. With this access, cholecystectomy can be safely performed through the navel, while leaving a scar that is practically invisible.
It is important to mention that, in addition to improving esthetic results, the aim is to improve postoperative recovery and make it possible to carry out cholecystectomy in a major outpatient surgery (MOS) program.
The objective of this study is to present the results obtained from the first 100 cases of single-port cholecystectomy (SPC) at a secondary-level hospital.
Material and MethodsBetween January 2010 and April 2012, a total of 100 patients underwent cholecystectomy at our hospital using the single-port umbilical access. The procedure was done exclusively by 3 surgeons with large experience in conventional laparoscopic cholecystectomy.
We designed a descriptive, prospective, observational, single-center study. For the case reviews, data collection and statistical analysis, a Microsoft® Access 2007 database and the SPSS v16 program were used. All the case data were sent and included in the National Single-Incision Surgery Registry (in Spanish, RNCIU), an initiative promoted by the Endoscopic Surgery section of the Spanish Association of Surgeons (AEC), whose aim is to study the level of implementation of these techniques as well as the main clinical, technological and technical aspects related with their use.
Inclusion criteria were: patients over the age of 16 years with symptomatic cholelithiasis, diagnosed by ultrasound, that underwent umbilical SPC.
Exclusion criteria were defined as: patients with clinical history of acute cholecystitis, patients who had previously undergone endoscopic retrograde cholangiopancreatography, history of pancreatitis or suspicion of choledocholithiasis, a body mass index greater than 35 and a history of previous laparotomies.
Patients were informed about the procedure and gave their signed consent.
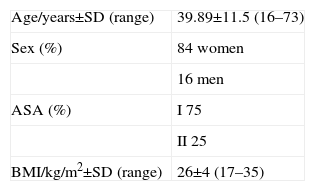
The epidemiological variables studied were: patient age and sex, American Society of Anesthesiologists (ASA) classification and body mass index. As for the surgical variables, we studied surgical time, hospital stay, postoperative complications, the use of accessory trocars and the number of conversions to open surgery, mortality and esthetic satisfaction.
The degree of esthetic satisfaction was evaluated with a postoperative survey one month after the surgery, where the patient was asked if he/she was unsatisfied, satisfied or very satisfied.
Surgical TechniqueFor the initial approach, a 2cm umbilical incision was made. The Quatriport trocar (Olympus®) was put in place under direct vision and the abdominal cavity was insufflated with CO2. Curved reusable (Olympus®) instruments were used with a 10mm all-in-one laparoscope with high definition 30° optic (Olympus®).
In the first 8 cases, the gallbladder was suspended with a transparietal stitch to achieve better handling and visualization of the structures. Later on, after having acquired greater experience with the technique, this was not considered necessary.
Standard cholecystectomy was performed with double clamping of the cystic artery and duct using 5mm surgical clips.
In most cases, the gallbladder was extracted without an extraction bag since the trocar itself was used as protection of the wall. In cases with risk of gallbladder rupture or contamination, however, extraction bags were used.
In all patients, anesthesia was instilled with 10ml of bupivacaine 0.25 without adrenalin in the subhepatic and suprahepatic spaces, in accordance with the anesthesia protocol. The degree of pain, however, was only studied in patients treated in the MOS setting, so we were therefore unable to draw conclusions to assess the effectiveness of this procedure.
The umbilical orifice was closed with non-absorbable interrupted stitches with subcutaneous anesthesia infiltration (10ml bupivacaine 0.5 with adrenalin), finalizing the procedure with an absorbable intradermal suture.
ResultsOne hundred laparoscopic cholecystectomies were performed with the SPC technique. The demographic data are shown in Table 1.
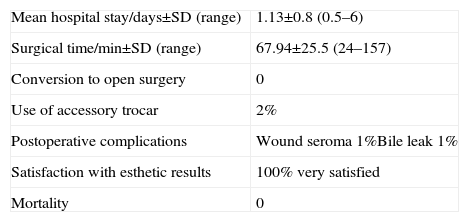
Mean surgical time was 67.94min (Table 2). In 55% of the patients, the surgical time was less than 1h. After the fifth procedure of each surgeon, mean surgical time dropped significantly.
Results of Surgical Variables.
| Mean hospital stay/days±SD (range) | 1.13±0.8 (0.5–6) |
| Surgical time/min±SD (range) | 67.94±25.5 (24–157) |
| Conversion to open surgery | 0 |
| Use of accessory trocar | 2% |
| Postoperative complications | Wound seroma 1%Bile leak 1% |
| Satisfaction with esthetic results | 100% very satisfied |
| Mortality | 0 |
Total n: 100.
Mean hospital stay was 1.13 days. 35% of the patients were included in the MOS program.
There were no conversions to open surgery, although in 2 patients it was necessary to use an accessory trocar due to the technical difficulty.
Postoperative complications included one case of non-infected seroma of the wound, which was followed-up in the outpatient consultation and showed no added complications. One case of biliary leak was diagnosed a few hours after the procedure, which required reoperation. The reoperation showed choleperitoneum secondary to a biliary leak due to defective clamping of the cystic duct. This was repaired laparoscopically with the use of 3 trocars. The patient was discharged 6 days after surgery. A patient in the MOS program was re-hospitalized after having been discharged due to poor control of abdominal pain, but was discharged 24h later without incident.
In the satisfaction survey, all patients responded that they were very satisfied. They had follow-up office visits both 1 and 3 months after the surgery. There was no mortality.
DiscussionThe 1990s were witness to a laparoscopic revolution, and laparoscopy substituted conventional open surgical techniques in many procedures. Currently, this less-invasive technique has become the technique of choice for several procedures, which has contributed to the improvement of different surgical and postoperative aspects.1
In the beginnings of laparoscopic cholecystectomy, several studies demonstrated a higher number of bile duct injuries due to the change of the technique and the learning curve, although this complication decreased when greater experience was gained in laparoscopy.2
Single-incision laparoscopic surgery is the most feasible and reproducible (in most hospitals) of all the innovations that have appeared in recent years in order to minimize the laparoscopic approach. In our series, with the first 100 cases of three different surgeons and their consequent learning-curves, there have been no cases of bile duct injury or any other serious complications.
In spite of the efforts made by manufacturers, the instruments used often make it difficult to perform the surgery optimally. The main disadvantage of single-incision surgery is that the instruments are very close together, which reduces the surgical field of vision and impedes the triangulation achieved with conventional laparoscopic surgery. In our study, we have tried to resolve this question by using pre-curved materials and all-in-one optics, thus reducing the contact with the instruments at the access port. Other authors use different types of specially developed instruments,3 although this makes the procedure significantly more expensive.
In this series, mean surgical time decreased after the fifth procedure done by each surgeon. Although surgical times are disparate due to the variability of each case, we believe that there is not a large difference with the conventional technique, and even in some patients the surgical time used may be shorter in SPC.4–6
The fact that we have not had any cases of conversion to open surgery is attributable to that fact that the procedure was limited to only 3 surgeons of the department with great experience in conventional laparoscopy, in addition to the strict selection of patients included in the study. In only 2 cases it was necessary to use an accessory trocar, which was given absolute priority to guarantee patient safety and reduce the risk of complications.
Currently, we avoid using traction of the gallbladder with transparietal stitches as these can lead to intraperitoneal biliary leak. Nonetheless, it is important to mention that in the first cases of the series, when this leak occurred, there was no postoperative morbidity while Calot's triangle was better exposed during the learning period.
The navel can be considered a natural scar where trocars and optics can be introduced.7 Unlike other authors,8–10 we prefer the trans-umbilical approach to the infra-umbilical approach as it offers patients a higher degree of esthetic satisfaction, and in our experience we have observed no cases of wound infection.
As the incision is larger than the incision of conventional trocars, some authors have reported an increase in the incidence of incisional hernias.11 In our series, for the moment we have observed no incisional hernias, although the follow-up is still not sufficiently long to be able to draw conclusions.
Aside from this, the larger skin incision facilitates the closure of the aponeurosis, so we doubt that there would be a larger number of umbilical hernia incisions compared with conventional laparoscopy.
One of the main limitations of our study, although it is prospective, is that it is a descriptive, observational, non-comparative, non-randomized study. Nevertheless, the experience obtained with this paper has allowed us to design another randomized prospective study yet to be finalized.
Furthermore, the perception of the patient as well as the surgeon that it is a less-invasive surgery means that it is often done in an MOS program.12 In our center, MOS cholecystectomy procedures were initiated with the advent of the SPC technique.
It is interesting to emphasize that what would explain the lack of acceptance and implementation of this technique in most hospitals are most likely its technical difficulty, learning curve and economic aspects. The price of the trocars used for conventional laparoscopic cholecystectomy has been ostensibly reduced in recent years, while this has not happened with the price of single-port devices.
While we did not prospectively evaluate costs per patient in this study, we can deduce that, despite using reusable instruments and conventional laparoscopy material, the price of the device continues to make the procedure too expensive. The added cost can be justified with the savings in the outpatient surgery program. In the near future, hopefully the prices of these devices and instruments will become reduced so that the use of the procedure becomes generalized.
The results obtained demonstrate that it is a safe, reproducible technique13–16 when patients, as well as the surgeons who perform it, are strictly selected.
After the initial learning period of the technique, it is possible to extend its application to more complex cases,17 facilitate the learning of the technique by other surgeons in the department, and use this approach to carry out other laparoscopic procedures.18,19
Because single-incision laparoscopic surgery is a technique with a great potential for innovation, we believe that multi-center clinical registries, such as RNCIU, are important to compile data about the efficacy and safety of the procedure in order to have greater information about the results obtained by the different groups that perform it in our country.20
In conclusion, the results obtained in this study can be extrapolated to any type of hospital as long as strict patient selection criteria are used and the technique is carried out by surgeons who are experts in laparoscopic cholecystectomy.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Subirana Magdaleno H, Jorba Martín R, Barri Trunas J, Robres Puig J, Rey Cabaneiro FJ, Pallisera Lloveras A, et al. Resultados de las 100 primeras colecistectomías por puerto único en un hospital de segundo nivel. Cir Esp. 2014;92:324–328.
This paper was originally presented as an oral presentation at the 29th National Congress of Surgery held in Madrid on November 13%3Fndash;15, 2012.